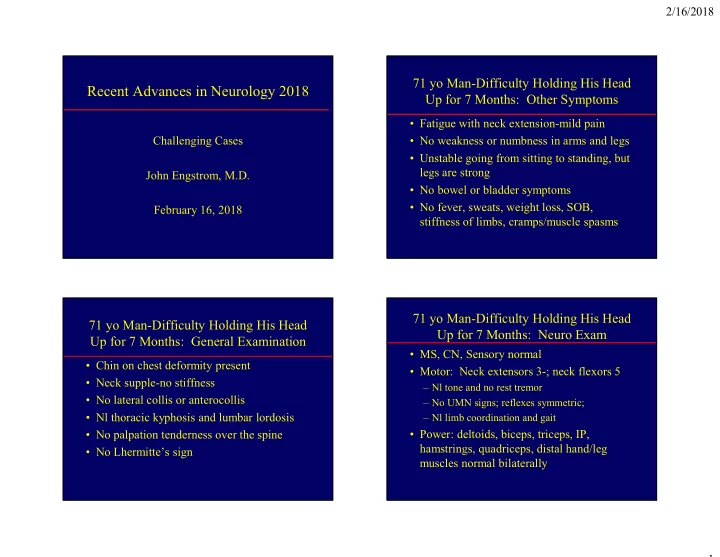
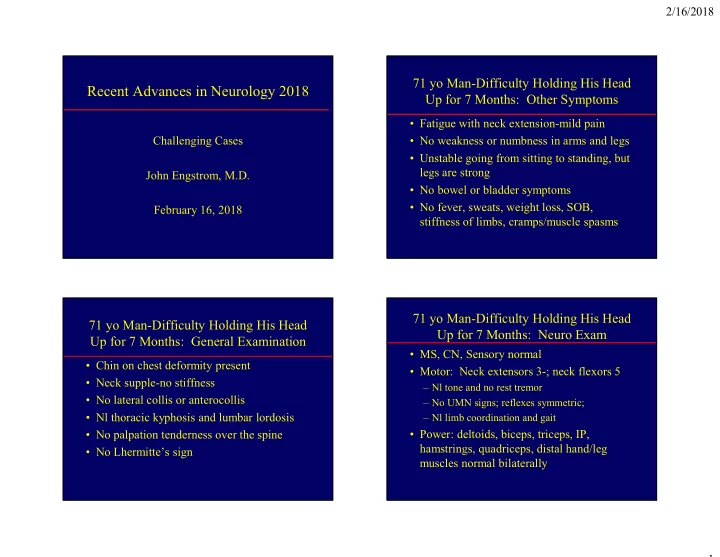
2/16/2018 71 yo Man-Difficulty Holding His Head Recent Advances in Neurology 2018 Up for 7 Months: Other Symptoms • Fatigue with neck extension-mild pain Challenging Cases • No weakness or numbness in arms and legs • Unstable going from sitting to standing, but legs are strong John Engstrom, M.D. • No bowel or bladder symptoms • No fever, sweats, weight loss, SOB, February 16, 2018 stiffness of limbs, cramps/muscle spasms 71 yo Man-Difficulty Holding His Head 71 yo Man-Difficulty Holding His Head Up for 7 Months: Neuro Exam Up for 7 Months: General Examination • MS, CN, Sensory normal • Chin on chest deformity present • Motor: Neck extensors 3-; neck flexors 5 • Neck supple-no stiffness – Nl tone and no rest tremor • No lateral collis or anterocollis – No UMN signs; reflexes symmetric; • Nl thoracic kyphosis and lumbar lordosis – Nl limb coordination and gait • No palpation tenderness over the spine • Power: deltoids, biceps, triceps, IP, hamstrings, quadriceps, distal hand/leg • No Lhermitte’s sign muscles normal bilaterally 1
2/16/2018 Q1-Which medical condition is Head Drop (aka “Head Ptosis”) associated with head drop? A. Upper cervical myelopathy • Upper cervical myelopathy 90% B. Anterocollis • Dystonia-anterocollis C. Bent spine syndrome • Assoc with PD, thoracic kyphosis, or both D. Parkinson’s disease • Orthopedic-Larsen syndrome E. All of the above • With camptocormia (bent spine syndrome) 5% 3% 2% 0% • As a neuromuscular disease s y e e e i m s h l l a v o o t o e a c s b p o r d i a o r d e n e e l t y s h ’ y n s n t A m e o f n s o a l i n l p i l c s k A i v t r n a r P e e c B r e p p U Camptocormia 71 yo man with Head Drop: Cervical Spine Flexion • Camptocormia (Bent Spine Syndrome)- anterior curvature of thoracolumbar spine – Orthopedic-Scheuermann’s kyphosis – Idiopathic – Parkinsonism – Motor neuron disease – Myopathies • Camptocormia and head drop can co-exist 2
2/16/2018 71 yo man with Head Drop: Cervical 71 yo man with Head Drop: Axial T2 Spine-Attempted Extension C4: Attn Paraspinal Muscles Q2-Which neuromuscular condition 71 yo man with Head Drop: Axial T2 is associated with head drop? C7-T1: Attn Paraspinal Muscles A. Motor neuron disease 88% B. Myasthenia gravis C. Polymyositis D. Muscular dystrophy E. All fo the above 5% 3% 2% 2% e s s y e i i s v t h v a i a s p o e r o o b s g y r a i d a m t s e n i y n y h l d t o e o r h o P r u t a e s f u l l n a l c A y r M s o u t M o M 3
2/16/2018 DDX of Head Drop as a Neuromuscular Disease 71 yo Man with Head Drop-Lab Studies • Motor Neuron disease (e.g.-ALS) • CK 67, AChRAb -, ESR 2, CRP 3.2-all nl • Proximal Polyneuropathy (e.g.-CIDP) • EMG-NCV/needle EMG studies nl except • Neuromuscular Junction Dz (e.g.-MG) right lower cervical paraspinal muscles • Myopathies – No fibs or positive waves – Inflammatory-Polymyositis, IBM – Short duration, low amplitude motor units with – Endocrine-Cushing syndrome, hypothyroidism early recruitment – Dystrophy-LGMD, FSH, a myotonic dystrophy – Myopathy-no muscle membrane instability – Idiopathic Cervical Paraspinal Muscle Normal Muscle biopsy-H and E Biopsy Results • Variation muscle fiber size-sugg dystrophy • Increased central nuclei • No perivascular or vascular inflammation • No significant mitochondrial abnormality • No degenerating or regenerating fibers • No inflammation • Not a treatable myopathy 4
2/16/2018 Head Drop: Cervical paraspinal Head Drop: Cervical paraspinal muscle biopsy-H and E muscle biopsy-NADH 71 yo Man with Head Drop: Head Drop: Cervical paraspinal Further Inquiry muscle bx-Electron Microscopy • Athena-Muscular Dystrophy Adv Eval – 33 dystrophy genes negative – 3 mutations (2 likely benign, 1 unknown signif) – 1 heterozygous mutation in Titin • Titin-”giant” muscle protein that regulates the length of the striated muscle thick filament with 363 coding exons – Assoc with 9 myopathies inclu LGMD type 2J – Adult recessive proximal muscular dystrophy 5
2/16/2018 Titin Shortens During Contraction- Q3-What Rx option is least attractive Stretches Myosin Thick Filament for management of head drop? 73% A. Hard collar B. Soft collar C. Physical therapy D. Cervical spinal fusion 18% 6% 3% r r y n a a p o l l l l a i o o r s u c c e h f d t f t l r o a a l S a n H i c p i s s y l h a P c i v r e C 71 yo Man with Head Drop: 71 yo Man with Head Drop: Initial Symptom Management Return to Clinic with Questions • Hard Collar • What is my prognosis? • Soft Collar • Will other muscles deteriorate? • Physical Therapy • Specific subtype of muscular dystrophy? • Adapted brace found online • How does this information influence the decision to have surgery at this point? • Initially declined to seriously consider surgery 6
2/16/2018 71 yo Man with Head Drop: 71 yo Man with Head Drop: Surgery Post-Surgery • Decision 2/17 for surgery to improve QOL – Limits lateral neck motion post-op understood – Cannot live well looking at the ground – Deferred until his wife’s affairs settled • Surgery 8/30/17-two stage procedure – C3-T2 posterior screw and rod fixation – C5-T1 ACDF Take Home Points: Head Drop Outcome in the Patient’s Words: What Has Surgery Done to Your Self-Image? • Axial weakness is best considered as a form of proximal weakness in neurologic Ddx • Can be neurologic or non-neurologic origin • What are the limitations of the surgery? • Can be disabling both in terms of physical • How do you interpret and mange the long and psychosocial function term risks? • In the context of long term management, • What has surgery change your self-image patients (and physicians) are allowed to and improved your quality of life? change their minds regarding management 7
Recommend
More recommend