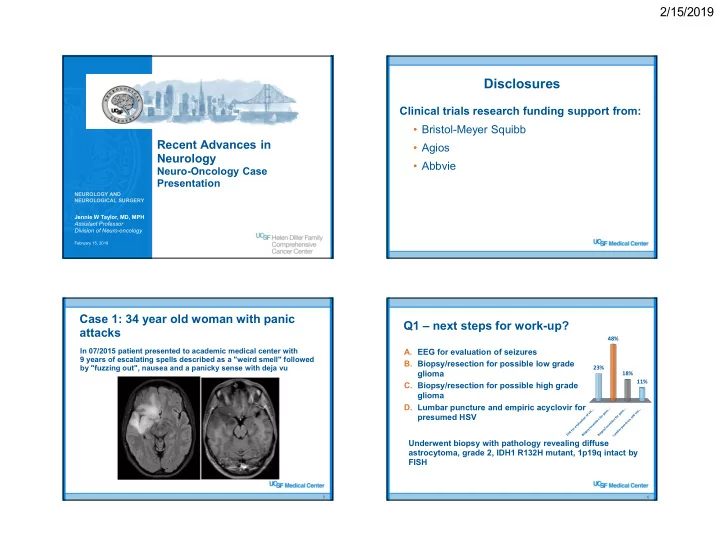
2/15/2019 Disclosures Clinical trials research funding support from: • Bristol-Meyer Squibb Recent Advances in • Agios Neurology • Abbvie Neuro-Oncology Case Presentation NEUROLOGY AND NEUROLOGICAL SURGERY Jennie W Taylor, MD, MPH Assistant Professor Division of Neuro-oncology February 15, 2019 Case 1: 34 year old woman with panic Q1 – next steps for work-up? attacks 48% In 07/2015 patient presented to academic medical center with A. EEG for evaluation of seizures 9 years of escalating spells described as a "weird smell" followed B. Biopsy/resection for possible low grade by "fuzzing out", nausea and a panicky sense with deja vu 23% glioma 18% 11% C. Biopsy/resection for possible high grade glioma D. Lumbar puncture and empiric acyclovir for . . . . . . . s . s . . . i . s s m e o o s e presumed HSV p p f d o r r n o o n f f a o n n e t i o o r a u u t i t i c c c t l e e a n v s s u e e e p r r r / / r o y y a s s f p p b G m o o E i i u E B B L Underwent biopsy with pathology revealing diffuse astrocytoma, grade 2, IDH1 R132H mutant, 1p19q intact by FISH 3 4 1
2/15/2019 Risk stratification of grade 2 gliomas Q2 – next steps in treatment? Construction set • EORTC 22844 and 22845 Overall survival • Prognostic index for low- A. Chemotherapy alone Low risk grade glioma: B. Chemotherapy with radiation – Age ≥ 40 High risk C. Radiation alone – Tumor diameter ≥ 6 cm D. Observation – Tumor crossing midline Validation set 46% – Astrocytic histology Overall survival – Pre-operative deficit Low risk 22% 22% • Low risk = < 2 factors High risk 10% – mOS ~ 7 years • High risk = ≥ 3 factors e . e n n . n o o d . o t i – mOS ~ 3 years a l a a l a r v y h n r p t o e a i i s r w t b e a Pignatti et al, J Clin Oncol 2002 y i O h d t p a o a m r R e e h h t C o m e h C 5 Radiation alone does not improve survival Radiation and chemotherapy improve in low-grade gliomas outcomes in low-grade glioma • EORTC 22845 Progression Free Survival • RTOG 9802 Progression Free Early radiation Upfront radiation versus – Upfront radiation versus Survival radiation at progression in radiation + low-grade gliomas Radiation at progression chemotherapy (PCV) in newly diagnosed high • Improvement in risk patients progression free survival (5.3 v 3.4 years; HR 0.59) • Improvement in Early radiation progression free survival • No improvement in overall Overall Survival Overall Survival (10.4 v 4.0 years; HR 0.50) survival (7.4 v 7.2 years; Radiation at progression HR 0.97) • Improvement in overall survival (13.3 v 7.8 years; • Improves seizure control HR 0.59) at one year (41% v 25%) Buckner NEJM 2016 van den Bent et al, Lancet, 2005 2
2/15/2019 06/2018 – Progressive Q2 – next steps in treatment? disease A. Chemotherapy alone • MRI revealed increased mass-like FLAIR and new B. Chemotherapy with enhancement with necrosis radiation • Clinically with increased C. Radiation alone fatigue, headaches, D. Observation inattention, and word finding difficulties • Recommended to undergo resection • Subtotal resection with pathology revealing glioblastoma, IDH mutated Temozolomide for 23 months (08/2017) 9 10 Q3 – next steps in treatment? UCSF500: Targeted sequencing • Pathology consistent A. Chemotherapy alone with anaplastic 80% oligodendroglioma B. Chemotherapy with radiation • > 50 non- C. Radiation alone synonymous somatic mutations D. Immunotherapy with either radiation and/or chemotherapy • Virtually all mutations are C>T/G>A 15% • No germ line 3% 2% alternations • These findings are indicative of Chemotherapy alone Radiation alone Chemotherapy with radi... Immunotherapy with eit... hypermutated phenotype from temozolomide 11 12 3
2/15/2019 Temozolomide-induced hypermutation Q3.5 – next steps in treatment? 100% • Defined as C>T/G>A A. Chemotherapy alone transitions predominantly B. Chemotherapy with radiation occurring at CpC and CpT C. Radiation alone dinucleotides, which is a D. Immunotherapy with either radiation distinct signature of TMZ- and/or chemotherapy induced mutagenesis not seen in other tumors 0% 0% 0% tumors e e n . . n o . o . . i . • Implicated is some cases l d l t a a a i e y r n p o h h a t i t r i t w i e w a i of malignant h d y y t p a p o R a m a r r e e e h h h t C t o transformation o m n u e m h m C I Immunotherapy with either radiation or chemotherapy • True incidence is not Johnson B, Science, 2014 known 13 14 Just a word on neurologic complications High mutational burden is predictive of response to immunotherapy checkpoint inhibition of checkpoint inhibitors... Cuzzubbo S, Eur J Cancer, 2017 Outcome of neurological adverse events correlated with a partial or complete neurological recovery in 73% of cases (20/27), with a median delay of 4 weeks. Yarchoan M, NEJM, 2017 15 16 4
2/15/2019 11/2018 – post-radiation Case 2: 57 year old woman with acute and immunotherapy onset of slurred speech • MRI revealed • MRI revealed enhancing mass with favorable response significant surrounding edema to treatment • Past medical history notable for • Expected post lupus, eczema, and thyroid disease surgical changes • Exam notable for dysarthria and • Decreased mass- right arm weakness like FLAIR • Clinically stable with improved seizure control 17 18 Case 2: 57 year old woman with acute Q1 – Next steps? onset of slurred speech • She underwent biopsy of left frontal A. Consider surgery for high suspicion of recurrent mass. Pathology: glioblastoma, IDH disease wildtype, MGMT unmethylated B. Continue adjuvant temozolomide 53% • Completed standard of care with C. Repeat radiation fractionated radiation and D. Start bevacizumab 37% temozolomide • 4 cycles of adjuvant temozolomide • MRI with increased enhancement 7% 3% and neurologic worsening expressive aphasia and right sided weakness Start bevacizumab Repeat radiation Consider surgery for high... Continue adjuvant temo... 19 20 5
2/15/2019 Underwent extensive resection Extent of resection (EOR) improves with sequencing 05/2015 outcomes for newly diagnosed GBM (9 months from diagnosis) • Retrospective review of Pathology revealed 10% recurrent 500 patients with newly glioblastoma and 90% treatment effect diagnosed GBM Genomic Alteration Drug MGMT unmethylated • EOR evaluated by 48 hour EGFR (V292L) Afatinib post-op MRI Erlotinib Ibrutinib • EOR was an independent Lapatinib Propranolol predictor of outcome Vandetanib when adjusting for age NF1 (T956fs) Trametinib and KPS PALB2 (S700fs) Carboplatin Cisplatin • Improvement in OS was Mitomycin Olaparib seen with incremental Oxaliplatin increase in EOR, starting TLK1 (K433N) Perphenazine Thioridazine at 78% Trifluoperazine Sanai, J Neurosurg, 2011 Treatment recommendation by Treatment recommendation by molecular tumor board molecular tumor board • Continued on trametinib monotherapy from 03/2016 • PALB2 mutation – 06/2017 (34 months from diagnosis) – Carboplatin : alkylating agent impairs DNA synthesis • Developed new seizures and increased mass-like FLAIR concerning for progressive disease – Olaparib : PARP inhibitor further damages DNA in platinum sensitive 03/2016 06/2017 tumors • NF1 mutation – Trametinib : MEK inhibitor blocks MAPK/ERK pathway of dysregulated cell growth • Stable disease after 10 months of carboplatin/trametinib from 06/2015 - 03/2016 (19 months from diagnosis) 23 24 6
2/15/2019 Q2 – Next steps? Re-irradiation to 35 Gy in 10 fractions A. Consider surgery for high suspicion of recurrent disease B. Restart temozolomide 52% C. Repeat radiation D. Start bevacizumab 37% 11% 0% e n b . d o a . . m i i m h t g a u o i i d z h o l i a c r z r a o o t v f m a e y e e b r p e t t g e r t R a r r u a t s t S s r e e R d i s n o C 25 26 Q3 - What are radiologic changes most Subacute radiation consistent with? • CNS complications of radiation occur in 3 clinical phases 90% – Acute (during treatment) A. Tumor progression – Subacute (within 6 months of treatment) B. Pseudoprogression – Delayed (within years of treatment) • Subacute effects (i.e. pseudoprogression) felt to be exaggerated response to radiation • Radiographically appears similar to tumor progression with increased enhancement at the site of maximum 10% radiation, increased edema, and mass effect. Often without significant diffusion restriction • Treatment includes steroids though anti-angiogenic Pseudoprogression Tumor progression therapy (i.e. bevacizumab) may be needed 27 28 7
Recommend
More recommend