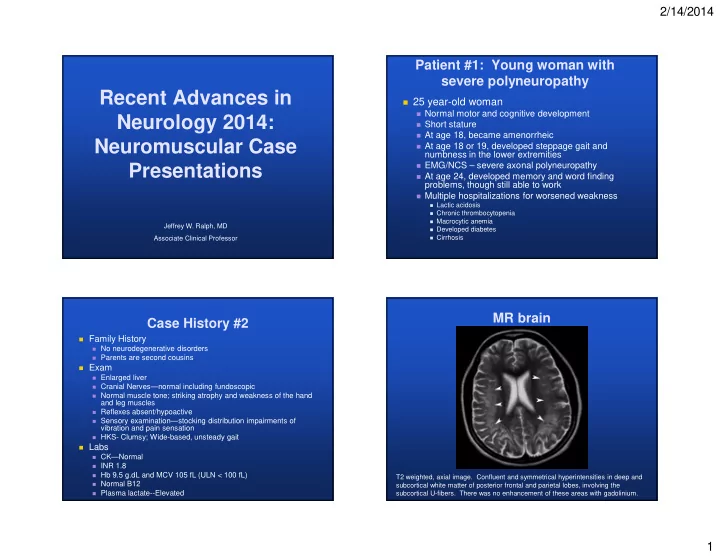
2/14/2014 Patient #1: Young woman with severe polyneuropathy Recent Advances in � 25 year-old woman � Normal motor and cognitive development Neurology 2014: � Short stature � At age 18, became amenorrheic Neuromuscular Case � At age 18 or 19, developed steppage gait and numbness in the lower extremities � EMG/NCS – severe axonal polyneuropathy Presentations � At age 24, developed memory and word finding problems, though still able to work � Multiple hospitalizations for worsened weakness � Lactic acidosis � Chronic thrombocytopenia � Macrocytic anemia Jeffrey W. Ralph, MD � Developed diabetes Associate Clinical Professor � Cirrhosis MR brain Case History #2 � Family History � No neurodegenerative disorders � Parents are second cousins � Exam � Enlarged liver � Cranial Nerves—normal including fundoscopic � Normal muscle tone; striking atrophy and weakness of the hand and leg muscles � Reflexes absent/hypoactive � Sensory examination—stocking distribution impairments of vibration and pain sensation � HKS- Clumsy; Wide-based, unsteady gait � Labs � CK—Normal � INR 1.8 � Hb 9.5 g.dL and MCV 105 fL (ULN < 100 fL) T2 weighted, axial image. Confluent and symmetrical hyperintensities in deep and � Normal B12 subcortical white matter of posterior frontal and parietal lobes, involving the � Plasma lactate--Elevated subcortical U-fibers. There was no enhancement of these areas with gadolinium. 1
2/14/2014 Which is true? Leukoencephalopathy Each mitochondrion has multiple copies 1. of mtDNA mtDNA is double stranded and linear Poly- 2. Cirrhosis neuropathy 60% mtDNA only replicates during cell 3. division Mitochondrial disorders are only 4. inherited maternally 19% 17% Lactic Acidosis 4% PLEASE SHOW RESPONSES!! . . . . . . . . . . . d . l p b a l n u e i o o r r h y d d n c n l o s o o t i h i A A c Mitochondrial syndrome was suspected. m N N o h D t D M i c t t a m m E Mitochondrial DNA Depletion Mitochondrial DNA Depletion Syndromes Syndromes TESTING: Hepatocerebral-DNA depletion syndrome panel: � Autosomal recessive Apparent homozygous mutations of MPV17 � Most syndromes present very early in life, but greater appreciation of adult-onset cases � nDNA genes encode key proteins Mitochondria Nucleus � Mitochondrial nucleotide synthesis � mtDNA replication � nDNA mutations � Cause depletion (reduced copy number) of mtDNA � May also cause multiple mtDNA deletions 2
2/14/2014 MPV17 Mitochondrial DNA Mitochondrial DNA Depletion Syndromes Depletion Syndrome Mitochondrial Gene Typical Age of Common Clinical Features Depletion Syndrome Onset Phenotype � Autosomal recessive TK2 Myopathic Infancy or early Muscle weakness, hypotonia, bulbar childhood weakness, elevated CK � Function of MPV17 is not known SUCLA2, Encephalomyopathic Neonatal- Hypotonia and muscle weakness, � In addition to mtDNA depletion, patients accrue multiple SUCLG1, Infancy psychomotor delay, short stature, mtDNA deletions RRM2B lactic acidosis, epilepsy DGUOK, � Clinical: Hepatocerebral Neonatal- Hepatic dysfunction, psychomotor MPV17, childhood delay, hypotonia, neuropathy, ataxia, � Severe axonal, mixed fiber polyneuropathies POLG, lactic acidosis, stroke or stroke-like � Liver: Steatohepatitis, cholestasis, cirrhosis and liver failure C10orf2 episodes, myoclonus and (Twinkle) choreoathetosis, epilepsy, � Lactic acidosis leukoencephalopathy, hearing loss � Leukoencephalopathy: Disabling cognitive problems and upper TYMP Neurogastrointestinal Late childhood- GI dysmotility, weight loss, motor neuron signs not common adolescence neuropathy, ptosis, ophthalmoplegia, � Novel in this case: Amenorrhea elevated thymidine and deoxyuridine in plasma, leukoencephalopathy Mutations in the nuclear DNA Mitochondrial DNA depletion may cause? syndromes: Reduced amounts of mtDNA in tissues Are autosomal recessive 1. 1. Multiple mtDNA deletions Usually present in infancy or early childhood 2. 2. Abnormalities on respiratory chain May have different phenotypes at different 3. 3. 85% enzyme testing ages of presentation 91% All of the above All of the above 4. 4. 10% 3% 3% 5% 2% 2% . . . . . . . . . PLEASE SHOW RESPONSES!! . A . . PLEASE SHOW RESPONSES!! n t s o N e b . . . u i a . . . . . o D t . n . e . . t i e l e f o m m a l a f b m h m s i a a t e d e o r e e d l r o f s p h e p o o v i n l t y a t c t l u l l h f u l b A a o d u A a u y e M e a l l U s M A R A r 3
2/14/2014 Patient #2: Myotonia congenita…or something else? 25 year-old man � � Lifelong muscle pain � Exercise was pain-limited since childhood � No bouts of visible myoglobinuria; no muscle contractures Family history: Mother and Maternal GF --similar � symptoms; MGF US Army dx: congenital myotonia Exam: � � Normal tone; normal or inc bulk; no grip myotonia � Percusssion of muscles produced: � Rapid contractions � Mounding of the muscles � Some rippling � Reflex, sensory, and gait examinations normal � Testing: CK 693 U/L Muscle Channelopathies Mutations of which of the following genes is not associated with myotonia? � Chloride Channelopathies: Myotonia � Myotonia Congenita � Autosomal Dominant – Thomsen disease 49% SCN4A –sodium channel � Autosomal Recessive – Becker disease 1. � Sodium Channelopathies: Myotonia or Paralysis or Both CACNA1S –calcium channel 2. � Potassium-Aggravated Myotonia CLCN1 –chloride channel 3. � Paramyotonia Congenita 24% � Hyperkalemic Periodic Paralysis All of the above 4. 16% � Other Cation Channelopathies: Paralysis without 11% Myotonia � Calcium Channelopathy � Hypokalemic Periodic Paralysis (*some SCN4A) . . . . . . . . . . e . . c u o � Potassium Channelopathy d m c i b i l r a u a o c e i l PLEASE SHOW RESPONSES!! d – h h o S c t s 1 – f � Andersen-Tawil syndrome – A 1 o A N N l 4 C C A l N A L C C C S � Thyrotoxic Periodic Paralysis 4
2/14/2014 Myotonia: Electrodiagnostic Testing Myotonia Congenita � Symptoms: Stiffness; falls; TESTING: INCREASED difficulty letting go; warm-up INSERTIONAL ACTIVITY BUT phenomenon NO MYOTONIA; NO DECREMENT OF CMAP ON � Onset: Early childhood REPEATED SHORT � Despite limitations, usually do well; EXERCISE TESTING can play some sports � Exam: Muscle hypertrophy; clinical and EMG myotonia; ? Becker patients may have fixed weakness � Caused by mutations of CLCN1 � AD (Thomsen) � AR forms (Becker) � AR > AD: Transient weakness shortly after initiating exercise Fournier et al., Annals, 2006 Could it be genetic rippling Caveolinopathies muscle disease? � Caveolinopathies Not again. � CAV3-Related Distal Myopathy � CAV3-Related Hypertrophic Cardiomyopathy � CAV3-Related Isolated HyperCKemia � CAV3-Related Rippling Muscle Disease � Limb-Girdle Muscular Dystrophy Type 1C � Patient TR: Mutation in CAV3 � Arginine 27 � Glutamine 5
2/14/2014 Rippling Muscle Disease Rippling Muscle Disease � Rippling Muscles � Historical � The direction of rippling is perpendicular to the orientation of the muscle fibers. � 1975: Torbergsen described a � Propogation of contraction is 10x slower than muscle family with dominant hereditary fiber action potential propagation. “myotonia,” muscular hypertrophy, � Rippling is ( mostly ) electrically silent. and muscular irritability. � Percussion-Induced Rapid Muscle Contractions � Distinct from myotonia congenita � Percussion-Induced Myoedema � 1980: Alberta probably reported � Muscular Hypertrophy the first sporadic case. � Mild CK elevations (<10x upper limit of normal) � “Increased mechanical muscle irritability syndrome.” Show Video of Rippling Rippling Muscle Disease Hereditary Acquired/Autoimmune Muscles Main Symptoms Myalgias ; Stiffness ± Stiffness; Weakness if MG Weakness also present CK Mildly elevated Mildly elevated EMG Increased Insertional Increased Insertional Activity Activity Treatment Dantrolene or Immunosuppressive Calcium Channel medications; Given benign blockers (single case natural history, may not be reports) necessary Disease None Myasthenia gravis Associations Thymoma Other lab None + Anti-striated muscle findings… antibodies + Ach Receptor antibodies Symptom Onset Childhood 33-60 years old 6
2/14/2014 Normal Neuromuscular Rippling Muscle Junction Disease CONTRACTION Ca++ Ca++ Ca++ Ca++ Abnormal Abnormal Ca++ Ca++ Ca++ Ca++ Ca++ Ca++ Ca++ Ca++ Ca++ Ca++ mV mV Pathophysiology of Rippling � Mechanical stretch activates the ryanodine receptor � sarcomere contracts � resulting stretch activates adjacent ryanodine receptors � etc. � Problems with hypothesis: � Very large, rapid stretches do not induce direct activation of SR Ca++ release in neonatal rat muscle fibers. � Activating 220,000 sarcomeres per second to cause the contraction seems implausible. � Why would a stretch affect the T-tubule system anyway? � Possible Explanation: Combined Propogation of the Region Mechanical and Electrical Hyperexcitability of Contraction 7
Recommend
More recommend