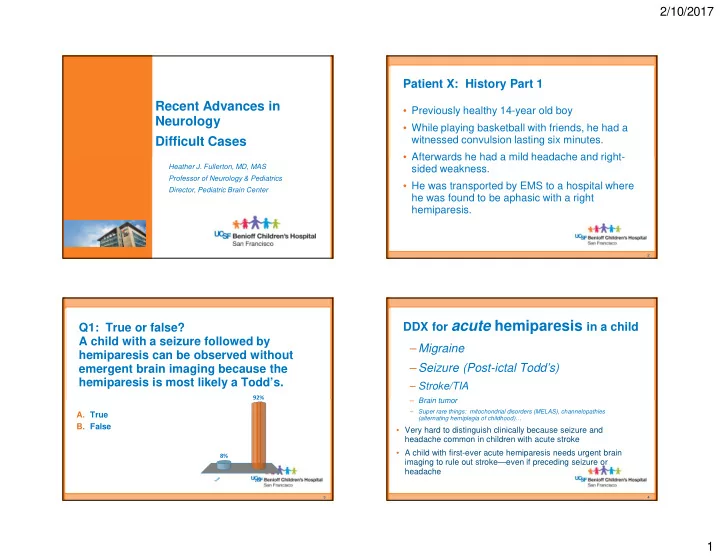
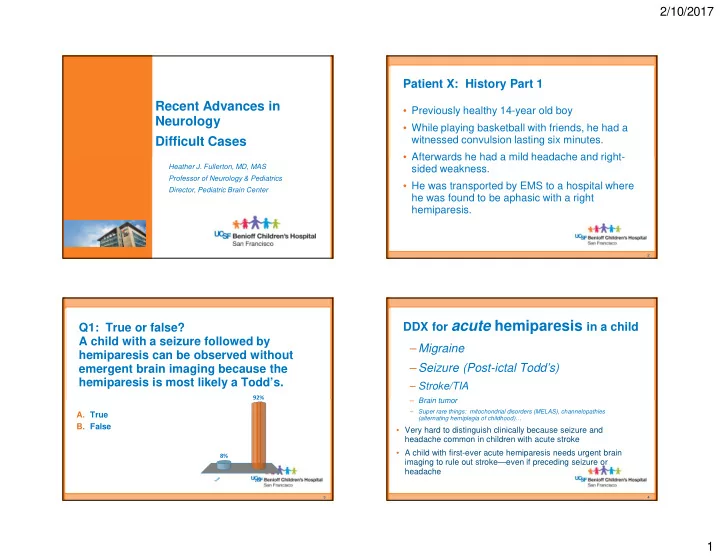
2/10/2017 Patient X: History Part 1 Recent Advances in • Previously healthy 14-year old boy Neurology • While playing basketball with friends, he had a witnessed convulsion lasting six minutes. Difficult Cases • Afterwards he had a mild headache and right- Heather J. Fullerton, MD, MAS sided weakness. Professor of Neurology & Pediatrics • He was transported by EMS to a hospital where Director, Pediatric Brain Center he was found to be aphasic with a right hemiparesis. 2 DDX for acute hemiparesis in a child Q1: True or false? A child with a seizure followed by – Migraine hemiparesis can be observed without – Seizure (Post-ictal Todd’s) emergent brain imaging because the hemiparesis is most likely a Todd’s. – Stroke/TIA 92% – Brain tumor – Super rare things: mitochondrial disorders (MELAS), channelopathies A. True (alternating hemiplegia of childhood)… B. False • Very hard to distinguish clinically because seizure and headache common in children with acute stroke • A child with first-ever acute hemiparesis needs urgent brain 8% imaging to rule out stroke—even if preceding seizure or headache e e s u l r a T F 3 4 1
2/10/2017 Half of strokes in kids are hemorrhagic Stroke does occur in Children: Children • Incidence: – 1 per 3,500 neonates – 4.6 per 100,000 children/year in US Adults Ischemic Hemorrhagic Hemorrhagic – About 5,000 US kids/year Ischemic Broderick, J Child Neuro, 1993 Agrawal, Stroke, 2009 Approach to Imaging for Suspected Stroke Approach to Imaging • What about CT/CTA? • Emergent MRI with DWI/ADC – Use sparingly: radiation more concerning in young • Followed by kids immediate brain MRA if + infarct – Useful if MR can’t be done • Especially if (pacer leads) or can’t be within 6 hour done quickly & thrombectomy thrombectomy would be window considered 10 hr old infarct in 5 month old • More thorough – Sensitive for hemorrhage, with congenital heart dz vascular imaging not acute infarct later – Don’t add CT perfusion (not worth the radiation) 2
2/10/2017 Q2: What is the most common cause of Patient X: History Part 2 arterial ischemic stroke in a previously healthy child? Back to our 14 year old boy with a convulsion followed by right hemiparesis and aphasia… A. Embolism from congenital heart disease • Emergent MRI: small infarcts 41% B. Embolism from endocarditis of L MCA territory 34% C. Sickle cell disease • MRA: mild narrowing of his left supraclinoid internal D. Genetic thrombophilia 17% carotid artery (ICA)— E. Arteriopathy thrombus versus 5% 2% arteriopathy? e s a y . i s i h . . t a l a i h i t d e a t r s p p i a i n d o o e c o b r i g l l m e n d e n c o t o r c e e r A h m m l k t c o o i c r r S i f f t e m m n e s s G i i o l o l b b m m E E 9 10 Kids with arteriopathy are at highest risk of recurrence Arteriopathy (disease of a cervical or 1.00 Proportion recurrent stroke free cerebral vessel) is the most common cause Almost 0.75 of childhood arterial ischemic stroke…. 1 in 4 0.50 And the strongest predictor of recurrent 0.25 stroke . 0.00 0 3 6 9 12 15 18 21 24 Fullerton, Time from index AIS to first recurrent stroke, months Stroke , Idiopathic 2015 Cardioembolic Possible arteriopathy Definite arteriopathy 11 3
2/10/2017 Patient X: History Part 3 MRA on transfer • Admitted to the hospital and placed on IV heparin. An echocardiogram was normal. His deficits improved dramatically over the next few days. • 3-days post stroke: severe left frontal headache. • 4-days post-stroke: agitated with worsened aphasia and right hemiparesis. • His deficits were positional, improving when placed flat, and responded to IV hydration and pressors. • Repeat MRI/A: new infarction in the left MCA territory and severe narrowing of his left distal ICA and proximal MCA . • Transferred to UCSF 13 14 FCAi Q3: What causes rapidly progressive stenosis of the distal ICA in children? Beading of M1 on conventional angiography Lenticulostriate infarcts A. Focal Cerebral Arteriopathy—Inflammatory (FCA-i), also known as Transient Cerebral Arteriopathy (TCA) B. Moyamoya disease (idiopathic moyamoya) C. Moyamoya syndrome (secondary moyamoya) 62% D. Kawasaki disease 18% 14% 5% e s . . . . a . . . . . e p o s o i ( i s d d r i i e e ( m i e k r t s o a A a s r a l e d a s n w r i a b d y s K e a a r y e o y C o m m l a a a c y o o y F M o M 15 16 4
2/10/2017 Natural History of FCA-i What causes FCA-i? • Monophasic disease • Varicella zoster virus (VZV)— strong evidence from histopathology studies • Initial progression • Other herpesviruses, like herpes simplex virus, type 1 • Nonprogression after (HSV-1)— evidence from case reports and a prospective case- 6 months control study (Vascular effects of Infection in Pediatric Stroke, VIPS study) • Improvement or stabilization; rarely • Other pathogens? normalization • Abnormal host immune response? – Chabrier & Sebire, J Child Neurol 1998; Danchaivijitr, Acute 2 months 12 months Ann Neurol 2006 Courtesy of G. DeVeber 18 Q4: What are proven therapies for FCAi? Patient X: History Part 4 • Admitted to the PICU, placed on IVF (1.5 x maintenance), head A. Aspirin of bed flat, on IV pressors B. Revascularization Surgery (STA-MCA bypass) • Had flow-dependent deficits: when upright, hemiparesis C. Acyclovir worsened 37% D. Corticosteroids • Serologies positive for HSV-1 E. None of the above • After several days of observation, with no improvement in flow- 23% dependent deficits, treated with IV corticosteroids and acylovir 18% 13% • After several days, patient stabilized 9% • Slowly weaned off IVF and pressors • 2 month follow-up: dramatic improvement in ICA stenosis n r s e i . i d r . v v i . o i o p y o r l r b s e c e a A y g c t r s e • 2 year follow-up: no further strokes u A o h S c t i n t f r o o o i e t C a n o z i N r a l u c s a v e R 19 20 5
2/10/2017 Before his arteriopathy progressed, Follow-up MRA could we have diagnosed him with FCAi? • FCA differential diagnosis: – FCAi – FCAd (focal cerebral arteriopathy, dissection subtype) • Intracranial dissection • Can also show early progression (spiral dissection) • Difficult to distinguish from FCAi • Vessel Wall Imaging (VWI) can help – Early, unilateral moyamoya • Lenticulostriate collaterals • Chronic, silent infarcts 21 22 Moyamoya disease/syndrome Enhancement on VWI: suggests FCAi • Slow narrowing of bilateral supraclinoid ICAs • 2ary lenticulostriate collaterals • Can be unilateral at onset • Secondary form: sickle cell disease, Down syndrome, NF-1, cranial radiation for cancer Courtesy of Max Wintermark, MD 6
2/10/2017 Childhood arteriopathy diagnosis important for management…and prevention of recurrent stroke Aspirin Heparin Revascularization Activity Hydration & Surgery (EDAS, Restriction BP STA-MCA bypass) augmentation FCAi x Rarely Acutely Dissection x Sometimes Lifelong Moyamoya x Routinely Long term Clinical trials planned for corticosteroids and acyclovir for FCAi. P.S. FCAi has also been reported in young adults 25 7
Recommend
More recommend