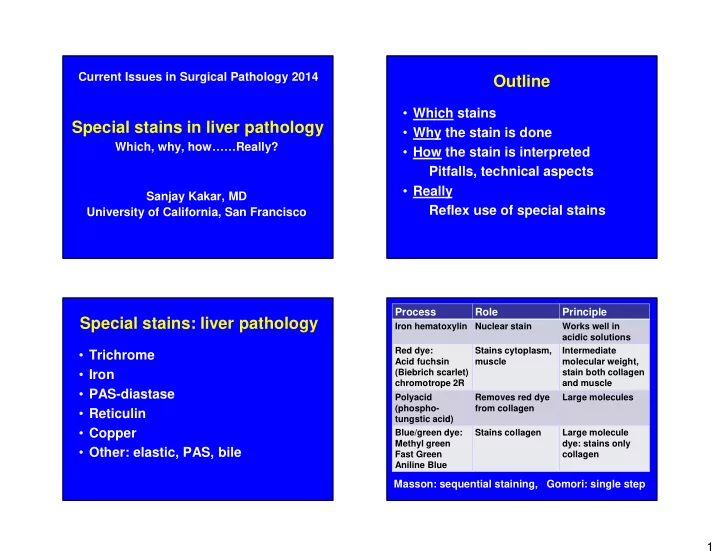
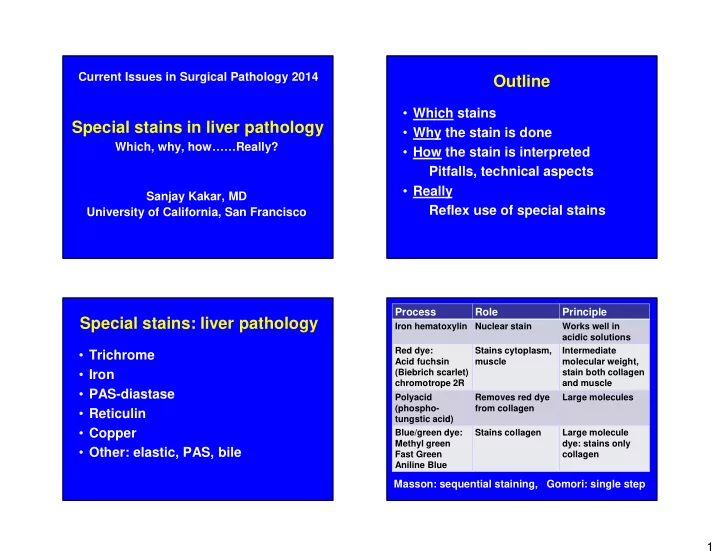
Current Issues in Surgical Pathology 2014 Outline • Which stains Special stains in liver pathology • Why the stain is done Which, why, how……Really? • How the stain is interpreted Pitfalls, technical aspects • Really Sanjay Kakar, MD Reflex use of special stains University of California, San Francisco Process Role Principle Special stains: liver pathology Iron hematoxylin Nuclear stain Works well in acidic solutions Red dye: Stains cytoplasm, Intermediate • Trichrome Acid fuchsin muscle molecular weight, • Iron (Biebrich scarlet) stain both collagen chromotrope 2R and muscle • PAS-diastase Polyacid Removes red dye Large molecules (phospho- from collagen • Reticulin tungstic acid) • Copper Blue/green dye: Stains collagen Large molecule Methyl green dye: stains only • Other: elastic, PAS, bile Fast Green collagen Aniline Blue Masson: sequential staining, Gomori: single step 1
Pale staining, no nuclear staining Trichrome stain • Why Staging: viral hepatitis, steatohepatitis Diagnosis of steatohepatitis Regression of cirrhosis Fibrosis vs. necrosis Recognizing unsuspected amyloidosis • How Interpretation and pitfalls Steatosis Steatohepatitis: essential features mild inflammation AASLD/NASH Clinical Research Network • Steatosis • Inflammation • Hepatocellular injury Ballooned hepatocytes Pericellular fibrosis 2
Steatosis Pericellular fibrosis Steatosis vs. steatohepatitis • Disease progression • Treatment Steatohepatitis guidelines 3
Pitfall in staging - histiocytic aggregate Overstained trichrome Chronic venous outflow obstruction Trichrome stain • Staging: viral hepatitis • Steatohepatitis • Regression of cirrhosis • Fibrosis vs. necrosis 4
Alcoholic cirrhosis with regression Cirrhosis regression • Thin fibrous septa with perforations • Prominent vessels and ductular reaction disappear • Nodularity may persist Wanless, Arch Pathol Lab Med, 2000 Friedman, Hepatology 2006 Chang, Hepatology, 2010 Thin septa: no shunting vessels or ductular reaction Regression: perforated fibrous septa 5
42 M with jaundice,hepatomegaly x 4 wks Live in the moment : Stephanie Page ALT, AST >1000 U/L Ultrasound: cirrhosis Dark: portal collagen, Light: necrosis Repeat trichrome 6
Orcein stain: no elastic fibers in necrotic area Amyloid: pale deposits Globular amyloid deposits: subtle on HE stain Globular amyloid: highlighted by trichrome → → → 7
Special stains: liver pathology Perls iron stain (not Perl’s) • Trichrome • K ferrocyanide + HCl • Iron • Ferric ferrocyanide (Prussian blue) • PAS-diastase • Max Perls: German pathologist • Reticulin • Copper • Other: elastic, PAS, bile Starry Night: van Gogh Entombment of Christ: Peter van der Werff, 1709 8
Normal iron regulation Iron stain • Why Distinguish from other pigments Semiquantitative analysis • How Patterns of hepatic iron overload Grading of iron overload Hepcidin • Activity depends on iron stores • Binds ferroportin • Genetic/acquired Hepcidin Ferroportin Transferrin • Increased iron Dietary Hemolysis Fig: Textbook of Liver Pathology: Kakar, Fig: Textbook of Liver Pathology: Kakar, Ferrell, Eds. Chapter by M Torbenson Ferrell, Eds. Chapter by M Torbenson 9
Iron storage Primary Pattern of siderosis Mechanism HFE HFE gene Hepatocellular Storage form Distribution hemochromatosis Starts periportal mutation Non- HFE Non- HFE Ferritin Mostly hepatocellular Iron oxyhydroxide and Virtually all cells hemochromatosis Some: macrophages mutations apoferritin Trace amounts in the plasma Hemosiderin Secondary Pattern of siderosis Mechanism Aggregates of iron Reticuloendothelial system oxyhydroxide crystals including Kupffer cells Hemolysis, multiple Macrophages Excess iron without apoferritin transfusions from RBC Chronic diseases Macrophages Excess iron in macrophages Hemosiderin Ferritin blush Iron stain: interpretation • Grading of iron overload • Patterns of hepatic iron overload 10
Deugner-Turlin grading scheme Modified Scheuer grading scheme Grade Definition Grade 0 Granules absent or barely discernible at 400x Grade 1 Granules discernible at 250x Grade 2 Granules discernible at 100x Grade 3 Granules discernible at 25x Grade 4 Masses visible at 10x or naked eye Iron: quantitative analysis Iron grading: simple method Can be performed from paraffin embedded tissue Grade Extent of iron Allows correlation with H&E morphology Normal iron 10-36 µmol/g of liver tissue Minimal <5% Mild 5-33% Mild increase Up to 150 µmol/g of liver tissue Moderate 34-67% Moderate 151-300 µmol/g of liver tissue Marked 68-100% Marked >300 µmol/g of liver tissue Hepatic iron index • Separate grade: hepatocellular, Kupffer cell µ g iron per gram dry weight of liver/55.846 • Hepatocellular: periportal vs. random patient's age >1.9: suggests hemochromatosis (non-cirrhotic) 11
Iron stain: interpretation History • Grading of iron overload • 35/M with obesity • Patterns of hepatic iron overload • Elevated serum ferritin • Liver biopsy: steatohepatitis Periportal hepatocellular siderosis Periportal hepatocellular siderosis 12
Periportal siderosis Iron overload in NASH • HFE hemochromatosis • 20-50% serum ferritin elevated • Non- HFE hemochromatosis • 15-60% increased hepatic iron • Secondary iron overload Distribution Interpretation Steatohepatitis Kupffer or hepatocellular Secondary • Rare conditions mild/moderate, random Hepatocellular, periportal HH or secondary Porphyria cutanea tarda Hereditary aceruloplasminemia Diagnosis History HFE 282Y homozygous • 55/M with cirrhosis • No HFE mutation • Steatohepatitis • HFE hemochromatosis with mild • No known etiology periportal hepatocellular siderosis, no portal based fibrosis Significance of iron overload or HFE mutations in progression of steatohepatitis is not clear 13
HII>2, heterogeneous iron overload Cirrhosis with siderosis • Non HFE hemochromatosis • Secondary siderosis in cirrhosis of another etiology Hemochromatosis Siderosis in cirrhosis Ludwig, Gastroenterology, 1997 Genetics Liver biopsy Clinical presentation (n=447, HII>1.9) 3 rd or 4 th decade Type 1 Autosomal recessive Hepatocytes Hereditary hemochromatosis 100% (HFE HH) C282Y homozygous, Liver, pancreas, C282Y /H63D heart, skin, joints Alpha-1-antitrypsin deficiency 28% 1 st three decades Type 2 Autosomal recessive Hepatocytes Cryptogenic cirrhosis 19% (Juvenile HH) Hemojuvelin (2A) or More severe hepcidin (2B) disease than HFE Alcoholic cirrhosis 14% HH Chronic hepatitis B, hepatitis C 18%, 7% Type 3 Autosomal recessive Hepatocytes Similar to HFE HH Transferrin receptor type Intermediate PBC, PSC 1% each 2 mutation between HFE HH and juvenile HH • Marked siderosis can occur in the absence of HH 1 st subtype: 4 th or 5 th decade Type 4 Autosomal dominant • Siderosis rare in biliary diseases Ferroportin mutation hepatocytes Severity varies • Siderosis is an adverse risk factor* 2 nd subtype: with type of Kupffer cells mutation *Brandhagen, Hepatology, 2000 14
HFE HH: Homogeneous distribution Siderosis: periseptal, stroma, endothelial cells Image: Dr. Linda Ferrell Bile duct siderosis Cirrhosis: HH or secondary siderosis Hereditary Cirrhosis with marked hemochromatosis secondary siderosis Homogeneous distribution Heterogeneous Siderosis in bile ducts, Generally absent stroma, endothelial cells HFE mutation (in HFE HH) Not present Diagnosis: Cryptogenic cirrhosis with secondary iron overload 15
Collapse with ductular reaction with siderosis: often nonspecific -High grade dysplastic lesions -50% develop HCC on follow-up Image: Dr. L Ferrell Iron stain: role of the pathologist Iron stain: role of the pathologist Clinical setting Interpretation Clinical setting Interpretation HFE C282Y homo HFE not known Extent of iron Raise possibility of HH C282Y/H63D Extent of fibrosis Periportal siderosis, or HFE other mutations moderate to marked Extent of iron No risk for HFE HH hepatocellular iron Recommend HFE testing Chronic viral hepatitis Steatohepatitis Possible disease progression Cirrhosis Possible poor prognosis 16
Special stains: liver pathology PAS-diastase stain • Trichrome Glycogen, other carbohydrates • Periodic acid converts –OH component • Iron to aldehyde • PAS-diastase • Combines with Schiff reagent: magenta • Reticulin complex • Copper • Diastase digests glycogen • Other: elastic, PAS, bile Mallory hyaline A1AT deficiency PAS-D stain • Why Alpha-1-antitrypsin deficiency Highlight macrophages Glycogen (with PAS stain) Giant mitochondria Highlights basement membrane • How Pitfalls Interpretation 17
A1AT deficiency A1AT deficiency Giant mitochondria Incomplete digestion 50/F with cirrhosis, obese, serum A1AT normal Immunohistochemistry: alpha-1-antitrypsin 18
PAS-D stain Cytoplasmic globules Sweet Spot: Robert Langford Contemplating Space: Sandra Wilson 19
Recommend
More recommend