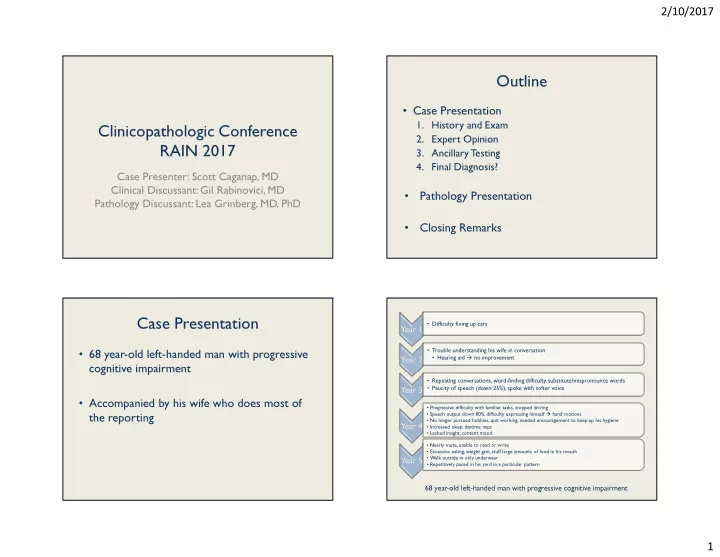
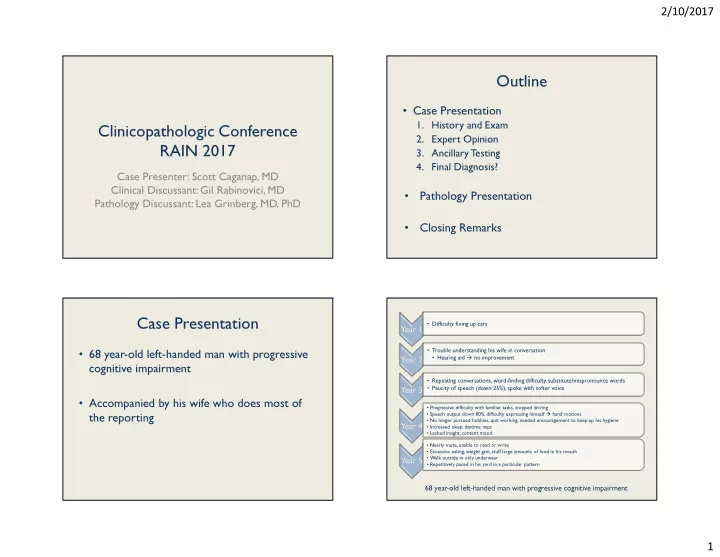
2/10/2017 Outline • Case Presentation 1. History and Exam Clinicopathologic Conference 2. Expert Opinion RAIN 2017 3. Ancillary Testing 4. Final Diagnosis? Case Presenter: Scott Caganap, MD Clinical Discussant: Gil Rabinovici, MD • Pathology Presentation Pathology Discussant: Lea Grinberg, MD, PhD • Closing Remarks Case Presentation • Difficulty fixing up cars Year 1 • 68 year-old left-handed man with progressive • Trouble understanding his wife in conversation • Hearing aid � no improvement Year 2 cognitive impairment • Repeating conversations, word-finding difficulty, substitute/mispronounce words • Paucity of speech (down 25%), spoke with softer voice Year 3 • Accompanied by his wife who does most of • Progressive difficulty with familiar tasks, stopped driving • Speech output down 80%, difficulty expressing himself � hand motions the reporting • No longer pursued hobbies, quit working, needed encouragement to keep up his hygiene Year 4 • Increased sleep, daytime naps • Lacked insight, content mood • Nearly mute, unable to read or write • Excessive eating, weight gain, stuff large amounts of food in his mouth • Walk outside in only underwear Year 5 • Repetitively paced in his yard in a particular pattern 68 year-old left-handed man with progressive cognitive impairment 1
2/10/2017 Review of Systems Review of Systems • Cognition: • Psychiatric: – No fluctuations in cognition or level of arousal – Approximately 10 years ago, he had a recurrent – Unclear if memory is an issue because he speaks delusion in which he suspected his wife of infidelity, but this resolved with marriage so rarely counseling – Does not get lost in familiar environments – No illusions, misperceptions, or hallucinations – No issues recognizing his family, but may not recognize former co-workers occasionally Review of Systems Personal History • PMH: BPH s/p laser surgery • Neurologic: • MEDS: tamsulosin, NKDA – No changes in vision • FH: two healthy sons; biological family not known – Difficulty swallowing (pills, large solids); coughs • Social History: during meals – Raised in foster care. Lost foster parents at a young – Intermittently kicked his legs while sleeping age. – Grew up in central California. Completed the twelfth – Generally slower movements grade without difficulty. – No tremor, weakness, incoordination, or recurrent – Most recently worked a part-time job as a dishwasher. Previously employed as a mechanic at an auto shop. falls – Rare alcohol consumption. No tobacco or illicit drug – Occasional urinary incontinence use. 2
2/10/2017 Examination Mental Status Exam • General: • Alert, DSF 4 – Normal vital signs, 137 lbs., 5’7” • Flat affect, slow to respond – Cooperative, well-groomed • Unable to spell WORLD backward, DSB 0 • Oriented to self, city, month, and date, but not season, year, or place • Word registration 3/3, recall 0/3 Mental Status Exam Mental Status Exam • Sparse speech, up to 4-word sentences, • Unable to copy intersecting pentagons • Could not pantomime blow-a-kiss or whistle grammatically correct • Used hand gestures when attempting to speak • Unable to perform 3-step hand movement • Named only a few simple objects task (Luria test) on both sides • Can repeat a simple sentence • Unable to perform multi-step tasks • MMSE 8/30 3
2/10/2017 Cranial Nerve Exam Cranial Nerve Exam • VFF, no extinction to DSS • Mild hypophonia and guttural dysarthria • PERRLA • Moderate hypomimia, full facial strength • EOMI except for limitation in up-gaze, gaze • Mildly diminished hearing bilaterally • Symmetric palate elevation impersistence • Normal saccades, no nystagmus • Normal tongue movements, no fasciculation Motor Exam Coordination Exam • Occasional BUE fasciculation • Intention tremor during FNF testing on R • Paratonia in all extremities • No dysmetria • Slowing of movements in all extremities (R>L) • Unable to perform RAMs • Reduced amplitude finger/foot tapping • No postural or rest tremor • Full strength 4
2/10/2017 Reflex Exam Reflex Exam • R palmar grasp • R palmomental & rooting reflex • Snout reflex Sensory Exam Gait Exam • Normal sensation to all modalities • Slow, cautious • No extinction to DSS • Short-stride length • Normal stereognosis • Decreased arm-swing bilaterally • No instability during Romberg testing • One step backwards during retropulsion testing 5
2/10/2017 Expert Opinion • What are your thoughts Dr. Rabinovici? Clinicopathological Conference: – Differential Diagnosis? 68 year-old with 5 years of cognitive and – Further Workup? behavioral decline – Leading Diagnosis? Gil Rabinovici, M.D. – Expected Underlying Pathology? Associate Professor of Neurology, UCSF 50 th Annual Recent Advances in Neurology February 10, 2017 Approach to Patient with Disclosures Cognitive Complaints • Research support • HPI probes cognitive domains – Avid Radiopharmaceuticals/Eli Lilly, GE Healthcare, – Memory: misplacing items, repetitive questions, missing Piramal Imaging appointments or bills, remote memory – Visuospatial: navigation, spatial relationships, object and – NIH (NIA, NINDS, NCATS), American College of face recognition Radiology, Alzheimer’s Association, Tau – Language: production and comprehension, motor speech, Consortium, Association for Frontotemporal reading and writing Degeneration, Michael J Fox Foundation – Executive: decision-making, judgment, multi-tasking, concentration/focus • Consulting/honoraria – Behavior: personality changes, depression, anxiety, apathy, disinhibition, psychosis – Eisai, Genentech, Lundbeck, Merck, Putnam, Roche – Motor • First or early symptoms particularly helpful • PMH, Meds, FH, SH may offer valuable clues 6
2/10/2017 Approach to Patient with Approach to Patient with Cognitive Complaints Cognitive Complaints • Labs: exclude “treatable” metabolic or • Mental Status exam and neuro- infectious causes psychological testing – Mandatory – Better define cognitive domains • Chem 20, CBC, B12, TSH – Discretionary • Physical neurological exam • RPR/FTA-ABS, HIV, homocysteine/methylmalonic acid, – Cranial nerves LP, rheumatologic, paraneoplastic, heavy metals, etc. – Motor: UMN/LMN, parkinsonism – Imaging (MRI preferred) – Exclude tumor, SDH, NPH, etc. – Sensory loss – Evaluate for vascular lesions – Ataxia – Pattern of atrophy – Gait Common Causes of From Clinical Syndrome to Pathology Neurodegenerative Dementia Aβ Disease Protein Anatomy Early Sxs Neuropsych Medial temporal Memory loss, Episodic memory Aβ, tau AD Posterior temporoparietal spatial disorientation Visuospatial Behavior spared Dysexecutive Tau Frontal Parkinsonism, RBD, Visuospatial α-synuclein DLB Occipital/temporal Psychosis, fluctuations Dysexecutive Aβ Basal ganglia Memory relatively spared Brainstem Frontal Disinihibition, apathy, Dysexecutive Tau FTD personality changes Anterior temporal Memory may be spared TDP-43 Aphasia, executive Visuospatial usually spared dysfunction TDP-43 FUS Motor-neuron disease Often frontal predominant Often dysexecutive, Often executive functions N/A VascD (but variable) memory, visuospatial, worst, though variable behavioral α-synuclein 7
2/10/2017 History: Behavioral History: Cognitive Symptoms Symptoms • First symptom: “difficulty performing skilled tasks” • Apathetic! (e.g. car repairs) – Loss of initiative, interest in hobbies, personal – Executive, motor planning or output, procedural memory hygiene, hyper-somnolence • Language decline • Blissfully unaware – “Difficulty understanding his wife” – comprehension, attention – Poor insight, not perturbed by deficits – Decreased speech output, short sentences – Mispronouncing words, soft voice, mutism - motor speech • Repetitive motor behaviors, pacing – Repeating previous conversations • Disinhibition • Episodic memory, perseveration – Walking around in underwear – Unable to read or write: pervasive language deficits • Overeating Frontal Circuits: Cognition & Behavior Speech Production Networks Key nodes: inferior frontal gyrus (BA 44), supplementary motor area (SMA), caudate Aberrant Motor Behavior T-score Executive Control Salience Network – Apathy T-score Network – Lateral, Medial, fronto-insular Key tracts: aslan tract (AT), superior longitudinal fasciculus (SLF), Disinhibition fronto-parietal Social-emotional T-score fronto-striatal Cognitive behavior Gorno-Tempini et al. Neurology 2006 Rosen et al. Brain 2005 Mandelli et al. Brain 2016 Seeley et al. J Neurosci. 2007 8
Recommend
More recommend