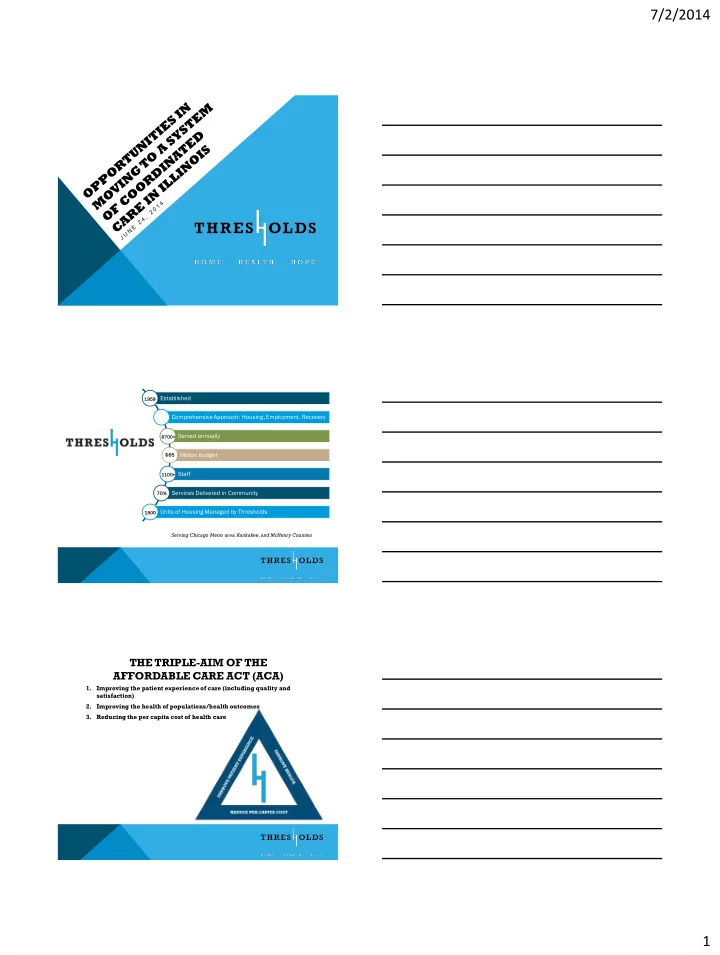
7/2/2014 Established 1959 1959 Comprehensive Approach: Housing, Employment, Recovery Served annually 6700+ Million budget $65 $65 Staff 1100+ 70% 70% Services Delivered in Community Units of Housing Managed by Thresholds 1500 Serving Chicago Metro area, Kankakee, and McHenry Counties THE TRIPLE-AIM OF THE AFFORDABLE CARE ACT (ACA) 1. Improving the patient experience of care (including quality and satisfaction) 2. Improving the health of populations/health outcomes 3. Reducing the per capita cost of health care 1
7/2/2014 FEE-FOR-SERVICE PAYMENT MODEL INCENTIVES VOLUME OVER OUTCOMES 1. The historic payment structure of Medicaid – Fee for Service (FFS) – incentivizes the wrong behavior: volume rather than good health outcomes. 2. Restrictive FFS billing rules inhibit care delivery. 3. Health outcomes are irrelevant under FFS. 4. The ACA and the triple aim moves the health care system to an outcomes-based system. SERIOUS MENTAL ILLNESS (SMI) POPULATION C H A L L E N G E S T O T H E S Y S T E M • Between 2009-2012, hospital ER visits for psychiatric/substance abuse crisis in Illinois increased by 19% — more than 35,000 additional visits — 12% higher than other medical ER visits. This cost Illinois $71.5 million. ILLINOIS AND MEDICAID REFORM M E D I C A I D R E D E S I G N I N L I N E W I T H T H E A C A • P.A. 96-1501 requires 50% of Medicaid enrollees to be in a system of coordinated care by 2015. (An integrated delivery system that includes primary care, diagnostic and treatment services, behavioral health care, hospital services and long-term care). • A patient-centered system with a focus in improved health outcomes. • Breaking down system, state and provider silos. Partnerships are key. • Multiple provider models being tested rather than only the MCO model. • Medicaid Expansion implementation: Over 350,000 new enrollees to date, many of whom have significant mental and behavioral health needs. Pursuit of 1115 Medicaid Waiver. 2
7/2/2014 March 2014 Care Coordination Roll-Out by Health Plans Illinois Health Connect Children with Newly eligible Seniors and Persons with Children/family and (IHC) complex health adults under ACA Disabilities (SPD) - in caregivers – in needs (CCEs) (Adults 19-64) mandatory managed care mandatory managed Primary Care Case - Statewide (growth based – in mandatory regions care regions Management (PCCM) managed care regions on capacity) program JUL 2014 JAN 2014 – All - outside mandatory JUL 2014 * counties managed care regions except Cook Integrated Care Program Medicare Medicaid 6 awarded (4 in Chicago area, 2 Ca (ICP) Alignment Initiative downstate) and additional projects Demo Area – Suburban (MMAI) statewide as they become available Cook/Collar MAY 2011 Accountable Care County Care (Cook County MAR 2014 - voluntary Entities (some to only) enrollment Mandatory JUN 2014 - mandatory begin JUL 2014 ) Cook County Waiver - Managed Care First Enrollment - NOV enrollment MCOs 2012 Expansion Same regions as ICP, Rockford JUN 2014 MCO CCEs MCCNs same MCOs as MMAI, (Aetna, s plus Harmony and County Care MCCN: (5) (1) IlliniCare, Greater Chicago 1) Be Well Partners Community Care JUL 2014 Family Health Network CCAI) Area: in Health (Chicago Alliance of ( May serve SPD & (FHN) JUL 2013 (SP 1 and Central IL (Molina, Aetna Better area) - FEB 2014 Illinois (CCAI) = children/families) 2) Health Meridian, Health Subsidiary of Illinicare Health Types of managed care entities: Alliance, Macon 2) EntireCare- Family Health Plan County CCE) Healthcare Consortium Network Meridian Health Plan of MCOs – Accepting full-risk capitation payments SEP 2013 (SP 1 and of Illinois (Chicago area) Rockford -JUL Illinois 2) - FEB 2014 2013 Chicago only HealthSpring of MCCNs – Provider-organized entities accepting Metro East 3) My Health Care – MAR Illinois full-risk capitation payments (Molina, Coordination-Macon 2014 Humana Health Meridian) County (down state) - Collar Counties Plan CCEs – Provider-organized networks SEP 2013 (SP 1 and SEP 2013 – JUL 2014 Blue Cross/Blue Shield of 2) 4) Precedence Care providing care coordination Quad Cities Illinois Coordination (down (IlliniCare, Central Illinois: state) - OCT 2013 ACEs – Provider-organized entities on a 3 year path to Precedence CCE) * Molina CCMN/CCEs NOV 2013 (SP 1 and full-risk capitation payments Healthcare 5) Together4Health 2) Lurie Children ’s Chicago (Greater Health Alliance Medical (Chicago area) – FEB CCE Chicago MMAI plans Plans 2014 La Rabida & CCAI) CCE Expand to - Managed Long Term Medical Home Targeted start dates in red OSF CCE Cook – MAR 2014 Supports & Services (MLTSS) – Network bold Collar – JUL 2014 All MMAI Plans (MHN) OPPORTUNITIES FOR PROVIDERS IN MOVING TO AN OUTCOMES-BASED PAYMENT MODEL 1. Flexibility in service delivery aimed at achieving good health and mental health outcomes for clients. 2. Innovation in service delivery. 3. Getting out from under restrictive FFS rules. CASE STUDY: ILLINICARE PILOT This partnership between Thresholds and IlliniCare brought together community-based mental healthcare with high-cost insurance users . Thresholds proposed to utilize our extensive experience in community-based care and wraparound services to help reduce costs for 50 of IlliniCare’s highest-cost users with a diagnosis of + serious mental illness. By paying Thresholds a flat per-user rate that was below the average pre-pilot cost, IlliniCare received guarenteed cost savings, while Thresholds had a guaranteed rate and high motivation to both improve health outcomes and significantly reduce costs. This pilot project’s stellar initial outcomes was featured in May 2014 at the National Council for Behavioral Health Conference in Washington, D.C. 3
7/2/2014 THE THRESHOLDS/ILLINICARE/CENP ATICO PILOT O V E R V I E W HOW THE PILOT CAME ABOUT Both Illinicare and Thresholds were looking Development of the partnership What Payers Want to Know • How will you help solve our problem? • Use of Evidence Based Practices • How do you measure outcomes? • Client satisfaction • Readmissions • How do you know someone is ready to leave care? • HEDIS scores (7 day follow up) • Integration between medical and behavioral • Internal monitoring of utilization management 12 4
7/2/2014 What Providers Want to Know • What are the payer’s business problems? • Will the payer share data? • How big a priority is this? • Invested in the collaboration? • Are they moving toward a shared risk mindset? • How much do they care about the lives of the people in their plans? • Will the payer consider alternate payment arrangements? 13 RUTHIE’S STORY IMPACT ON PEOPLE’S LIVES Housing was key Connection to family Linked to psychiatry (telepsychiatry) Connected with primary care A few were employed Not 100% success, but outcomes overall were very good 5
7/2/2014 OUTCOME DATA • 50% reduction in behavioral health admissions • 55% reduction in 30 day readmissions • 58% reduction in 90 day readmissions • 63% reduction in costs for behavioral health inpatient (with 12 months in pilot) • Optimistic about future: 69.2% 92.3% • Contact with friends 61.5% 80.8% • Living independently 42.3% 57.7% #NatCon14 17 CONTACT INFORMATION Heather O’Donnell Vice President, Public Policy and Advocacy hodonnell@thresholds.org (773) 572-5438 Debra Howard-Frye Associate Director, Chief Clinical Officer debra.howard-frye@thresholds.org (773) 572-5401 6
Recommend
More recommend