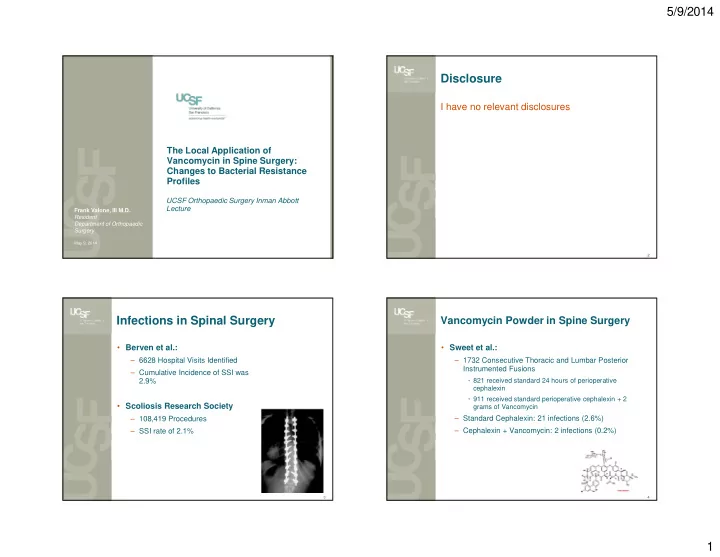
5/9/2014 Disclosure I have no relevant disclosures The Local Application of Vancomycin in Spine Surgery: Changes to Bacterial Resistance Profiles UCSF Orthopaedic Surgery Inman Abbott Lecture Frank Valone, III M.D. Resident Department of Orthopaedic Surgery May 9, 2014 2 Infections in Spinal Surgery Vancomycin Powder in Spine Surgery • Berven et al.: • Sweet et al.: – 6628 Hospital Visits Identified – 1732 Consecutive Thoracic and Lumbar Posterior Instrumented Fusions – Cumulative Incidence of SSI was 2.9% • 821 received standard 24 hours of perioperative cephalexin • 911 received standard perioperative cephalexin + 2 • Scoliosis Research Society grams of Vancomycin – Standard Cephalexin: 21 infections (2.6%) – 108,419 Procedures – SSI rate of 2.1% – Cephalexin + Vancomycin: 2 infections (0.2%) 3 4 1
5/9/2014 Determining Resistance to Vancomycin Vancomycin in Spine Surgery in Spinal Surgery • Molonari: – 1512 Consecutive Spinal Surgeries – All received 1 gram Vancomycin beneath the fascia • Research within the Department of – 15 patients (0.99%) infection rate Orthopaedic Spine Surgery • Sweet et al: • Two part: – 1001 posterior cervical spine surgical procedures 1. Global changes to bacterial resistance patterns at a from1995 to 2010 retrospectively reviewed tertiary academic spine center – Infection rate of 0% in group with the addition of 2. Retrospective Data Analysis of all patients from 2011 500mg of Vancomycin to current - Statistical correlation between Vancomycin use and Vancomyci resistant microbe development 5 6 Part 1: Global Changes to Microbial Determining Microbial Resistance Resistance Profiles Patterns to Vancomycin in Spine Surgery • 126 bacteria were isolated from 81 surgical site infections from 2007-2013 • Bacterial Resistance profiles were analyzed by Microbiologic Profile of SSI in Spine Surgery 2007 epoch (No Vancomycin resistance isolates) Staph Aureus (MSSA) Staph Aureus (MRSA) Ent erobacter Cloacae Psuedomonas Eschericia Coli Klebsiella pneumonia 7 8 2
5/9/2014 Determining Microbial Resistance Determining Microbial Resistance Patterns to Vancomycin in Spine Surgery Patterns to Vancomycin in Spine Surgery Microbiologic Profile of SSI in Spine Surgery 2009 (No Vancomycin Resistant iIsolates) Microbiologic Profile of SSI in Spine Surgery 2008 (One Vancomycin Resistant iIsolate - Enterococcus Faecium) St aph Aureus (MSSA) Staph Aureus (MSSA) St aph Aureus (MRSA) Staph Aureus (MRSA) St aph Epidermidis (MSSE) Proprionobacterium Acnes St aph Epidermidis (MRSE) Staph Epidermidis (MRSE) Ent erobact er Cloacae Proprionobact erium Acnes Eschericia Coli Eschericia Coli Pseudomonas Klebsiella pneumonia Klebsiella Oxyt oca Corynebacterium Corynebact erium Enterococcus faecalis Acinet obact er lwof f i Proteus Mirabelis Cit robact er f reundii Ent erococcus f aecalis Prot eus Mirabelis Ent erococcus Faecium (Vanc Resist ant ) Cit robact er Koserii Sweet’s Article Presented 9 10 Determining Microbial Resistance Determining Microbial Resistance Patterns to Vancomycin in Spine Surgery Patterns to Vancomycin in Spine Surgery M i c r obi ol ogi c P r of i l e of S S I i n S pi ne S ur ge r y 2 0 11 M icro bio lo gic Prof ile of SSI in Sp ine Surgery 2 0 10 ( No Va nc omy c i n Re si st a nt i I sol a t e s) ( N o V ancomycin R esist ant iIsolat es) S taph Aur eus (MSS A) Pr opr ionobacter ium Acnes Escher icia Coli S taph Epider m idis (MRS E) St aph Aur eus (M SSA) Enter ococcus f aecium St aph Aur eus (M RSA) Cor ynebacter ium Ci tr obacter Fr eundi i Enter ococcus f aecalis St aph Epi der mi di s (M RSE) Pr oteus Mir abelis Escher i chi a Col i Enter obacter Cloacae Peptostr eptococcus Klebsiella Pneum onia Pseudom onas 11 12 3
5/9/2014 Determining Microbial Resistance Determining Microbial Resistance Patterns to Vancomycin in Spine Surgery Patterns to Vancomycin in Spine Surgery Microbiologic Profile of SSI in Spine Surgery 2013 M i c r obi ol ogi c P r of i l e of S S I i n S pi ne S ur ge r y 2 0 12 ( One Va nc om y c i n R e si st a nt i I sol a t e - Ent e r oc oc c us Fa e c i um) (No Vancomycin Resistant iIsolates) Staph A ur eus (M SSA ) Str ept ococcus angi nosus Pseudomonas E s cher i c hi a Col i Staph E pi der mi di s (M RSE ) Citrobacter Freundii Staph E pi der mi di s (M SSE ) P s eudomonas Staph Epidermidis (MSSE) Cor ynebacter i um E nter ococcus Faeci um (V anco Resi s tant) Staph Epidermidis (MRSE) P r opr i onobacter i um A cnes Escherichia Coli M or ganel l a M or gani K l ebsi el l a P neumoni a 13 14 Bacterial Resistance Patterns Part 2: Figure 1: Microbiologic changes in Spinal Surgery Infection (2007 - 2013) Retrospective Analysis of consecutive cases 2011 - Current: 12 Staph Aureus (MSSA) • Number of Cases 1013 Staph Aureus (MRSA) 10 Staph Epidermidis (MSSE) • Vancomycin 1 gram free 134 Staph Epidermidis (MRSE) Enterobacter Cloacae Number of Bacteria isolated per year • Vancomycin 1 gram with bone graft 41 8 Proprionobacterium Acnes Eschericia Coli • Vancomycin 2 gram free 236 Klebsiella pneumonia 6 Klebsiella Oxytoca • Vancomycin 2 gram with bone graft 63 Corynebacterium Acinetobacter lwoffi 4 • None 538 Citrobacter freundii Enterococcus faecalis Proteus Mirabelis 2 Enterococcus Faecium (Vanc Resistant) Enterococcus Faecium (Vanc • No patient given local application of Sensitive) Citrobacter Koserii Vancomycin developed a vancomycin resistant 0 Pseudomonas 2007 2008 2009 2010 2011 2012 2013 microbe Peptostreptococcus * * Year Streptococcus Anginosus Morganella Morgani 15 16 4
5/9/2014 Conclusions Discussion • Part 1: 1. How do bacteria become resistant to antibiotics: • Vancomycin resistant Microbes are rare in spine surgical site infections (2) • Preventing the antibiotic from getting to its target • There has not been a significant increase in • Changing the target Vancomycin resistant surgical site infections since Sweet’s study was introduced • Destroying the antibiotic • Part 2: 2. Transformation, plasmid, transposons, mutation • There was no significant correlation between Vancomycin placed intra-operatively and 3. Antibiotic effects on resistance: Vancomycin resistant microbes 1. Bacteriostasis 2. Exposure of bacteria to subtherapeutic antibiotics 1. Selection for resistant bacteria 17 18 Vancomycin Application Limitations/Future • Short term follow up 1. Produce high antibiotic levels at the site of the – Necessary step possible infection, yet safe drug levels in the • Continue follow up globally and for each patient systemic circulation that receives Vancomycin application • Vancomycin: • Thank you: – BacterioCIDAL: when concentration is 4 x MIC – Serena Hu, M.D. – Example: – Sigurd Berven, M.D. • 2 x MIC for common spine pathogen (MRSA) – Shane Burch, M.D. – Trough of 32-40 – Bobby Tay, M.D. – High Risk of Toxicity – Vedat Deviren, M.D. 19 20 5
Recommend
More recommend