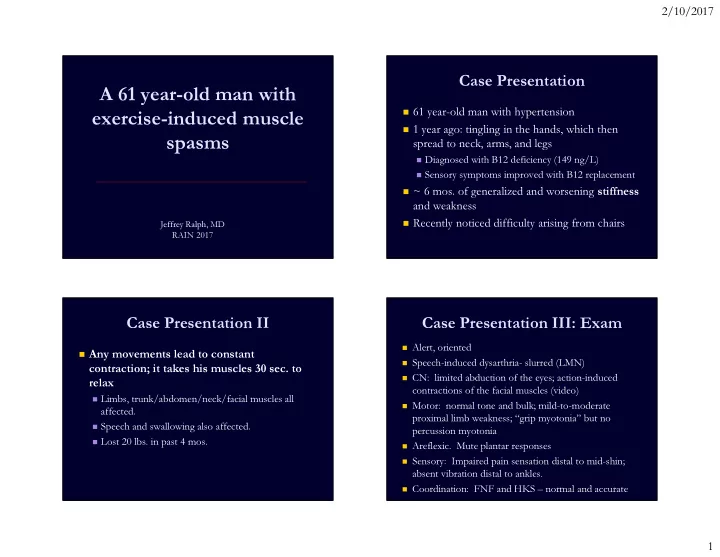
2/10/2017 Case Presentation A 61 year-old man with � 61 year-old man with hypertension exercise-induced muscle � 1 year ago: tingling in the hands, which then spasms spread to neck, arms, and legs � Diagnosed with B12 deficiency (149 ng/L) � Sensory symptoms improved with B12 replacement � ~ 6 mos. of generalized and worsening stiffness and weakness � Recently noticed difficulty arising from chairs Jeffrey Ralph, MD RAIN 2017 Case Presentation II Case Presentation III: Exam � Alert, oriented � Any movements lead to constant � Speech-induced dysarthria- slurred (LMN) contraction; it takes his muscles 30 sec. to � CN: limited abduction of the eyes; action-induced relax contractions of the facial muscles (video) � Limbs, trunk/abdomen/neck/facial muscles all � Motor: normal tone and bulk; mild-to-moderate affected. proximal limb weakness; “grip myotonia” but no � Speech and swallowing also affected. percussion myotonia � Lost 20 lbs. in past 4 mos. � Areflexic. Mute plantar responses � Sensory: Impaired pain sensation distal to mid-shin; absent vibration distal to ankles. � Coordination: FNF and HKS – normal and accurate 1
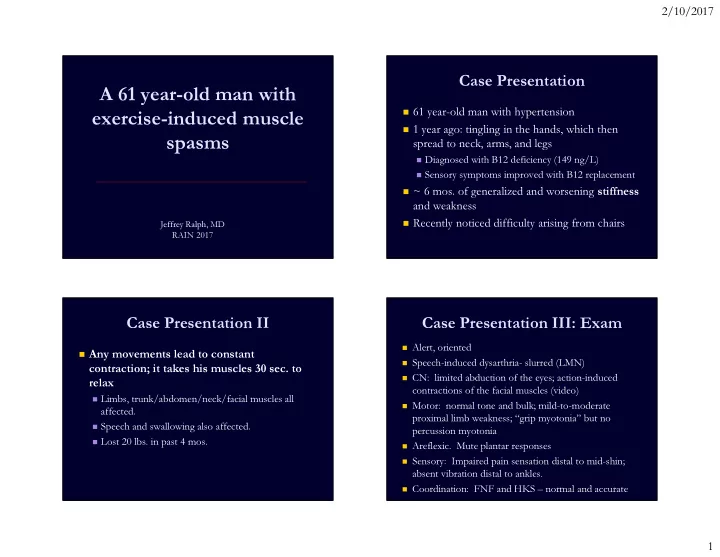
2/10/2017 Other information: Video I � Elevated anti-GAD antibodies (>250 IU/mL) � Normal MRI imaging of the brain and cervical spinal cord TRANSFER TO UCSF: STIFF PERSON SYNDROME What would you do next? Always do an EMG/NCS first! * A. 1. Full serum paraneoplastic panel � Nerve Conduction Studies – abnormal findings: � Reduced motor nerve conduction velocities in two B. 2. Lumbar puncture for CSF analysis 54% nerve segments (R median elbow-axillary and R C. 3. Toxicology consultation ulnar AE-axillary segment) D. 4. Genetic testing 27% � Prolonged F waves for 2/4 nerves 14% � Absent SNAPs in the lower extremities 5% � EMG very abnormal… All good answers, but something else 4. Genetic testing 1. Full serum paraneopla... 3. Toxicology consultation 2. Lumbar puncture for ... done in this case… * Just kidding…sort of 2
2/10/2017 Video II: EMG Which is most likely? A. Positive Caspr2 Abs B. A CTG trinucleotide repeat expansion 59% C. Frequently consumes local seafood D. Multiple sclerosis 35% 6% 0% s s b . . i . . . s A e a o p c 2 r e o e r l l p r c s e s s a e d m e C i l t u p e o i v s t e n l i l u i t c o M s u c o n y P i r t l t n G e T u C q e A r F The discharges Electrographic Neuromyotonia remind me of What was that EMG? Isaacs Syndrome A burst of motor unit action potentials which � originates in motor axons firing at high rates (150 to 300 Hz) for a few seconds Sounds like a Formula 1 Car � Often start and stop abruptly. � The amplitude of the waveforms typically wanes. � Discharges may occur spontaneously or be � initiated by needle electrode movement, voluntary effort, ischemia, or percussion of the nerve. These discharges should be distinguished from � Electrographic myotonic discharges and complex repetitive discharges. Neuromyotonia Miss Him 19,000 RPM x 1 min/60 sec = 317 Hz 3
2/10/2017 On motor nerve conduction studies, trains of after- Neuromyotonic Discharge, II discharges are often seen after supramaximal stimulation of nerves. Sections from longer continuous EMG recordings illustrating decremental patterns and varying partial motor unit size occurring within high frequency bursts of neuromyotonia . Maddison P. Neuromyotonia Clinical Neurophysiology, Volume 117, Issue 10, 2006, 2118–2127 Tibial motor nerve conduction study Neuromyotonia Additional Results Fasciculations or Cramps or Doublets, VGKC, VGCC, Hu, Yo, Ri – � � TPA - neg Myokymia Neuromyotonia Cramp Fasciculation Triplets negative � SPEP - Hypoalbuminemia, Syndrome CSF WBC 2 protein 45 mg/dL; � normal pattern PERIPHERAL NERVE HYPEREXCITABILITY SPECTRUM glucose 64 mg/dL Peripheral Nerve Hyperexcitability � Light chains - WNL CK - 181 � • Causes • Hemoglobin A1c - 5.2 (6/2) � IFE - Neg � Immune • Genetic TSH - 8.22, T3 3, T4 9 � � Anti-Intrinsic Factor: • Idiopathic/Miscellaneous Anti-thyroglobulin antibodies - � Positive 2.21 � Clinical neuromyotonia includes the following: � Anti-GAD65 > 250 Anti-thyroperoxidase antibodies � � Muscle twitches � ESR 39 167 � Muscle stiffness B12 - >2000 � � Cramps Activity-induced neuromyotonia. HIV - neg � � PET/CT – neg for � Hyperhidrosis Only seen in a minority of hypermetabolic lesions patients. � Pseudo-myotonia 4
2/10/2017 Disease Associations with Neuromyotonia Neuromyotonia � Autoimmune � Paraneoplastic � Generalized Neuromyotonia = Isaacs Syndrome � Myasthenia gravis � Small cell lung carcinoma � Muscle twitches, Muscle stiffness, Cramps, � Diabetes mellitus � Lymphoma Hyperhidrosis, Pseudo-myotonia � CIDP/GBS � Plasmacytoma � Celiac disease � Thymoma (with or without � Morvan’s fibrillary chorea MG) � Pernicious Anemia � Morvan in 1890: “La chorée fibrillaire” � Hyperthyroidism/hypothyroidism � Drugs � Vitiligo � Gold, oxaliplatin � Clinical features: � Infections � Genetic � Neuromyotonia � Staphylococcal infections � Hereditary neuropathy, � Insomnia KCNA1 mutations � Toxins � Delirium � Herbicides, insecticides, toluene, � Dysautonomia timber rattle snake Channels and Nerve/Muscle Hyperexcitability Clinical Course Monophasic K+ “Channelopathy” Neuromyotonia Symptoms � Symptoms � Sodium Channelopathy Time � Myotonia Time � Chronic Progressive Chloride Channelopathy Relapsing-Remitting 5
2/10/2017 VGKCs and Neuromyotonia The Expanding World of Auto- antibodies � Antibody in neuromyotonia discovered when dendrotoxin used in VGKC ABS Caspr2 radiolabeled Abs immunoprecipitation assay � VGKCs found in about Lgi1 Abs 40% of patients with neuromyotonia Scatter plot of serum VGKC antibody titres in 39 patients with the neuromyotonia phenotype of autoimmune peripheral nerve � Limited yield partially related hyperexcitability. Patients with thymoma are shown separately. Titres were considered positive if more than the mean plus 3 SDs. to dendrotoxin failure to Maddison P. Neuromyotonia. Clinical Neurophysiology, Volume Turns out that the VGKC antibodies 117, Issue 10, 2006, 2118–2127 Lgi1 = leucine-rich are mostly targeting non-channel Caspr2 = contactin- block all members of the associated protein-like 2 glioma inactivated 1 proteins complexed with Kv1 VGKC family The Expanding World of Auto-antibodies Which would be the wrong treatment for the patient? Caspr2 CNS dysfunction/ 43% Neuromyotonia Limbic Encephalitis A. 3,4 Diaminopyridine LGI1 30% B. Dronabinol C. Gabapentin • LGI1 – Is the main autoantigen of limbic encephalitis previously attributed to 14% 13% VGKCs D. Carbamazepine • CASPR2 – Is the autoantigen of encephalitis and PNH previously attributed to VGKCs • It is possible (rare) to have antibodies to LGI1 and CASPR2 but not VGKCs • Positive VGKCs but negative LGI1 and CASPR2 of debatable clinical e l n e o n i n n t i n i d i p b e e i r a p z y significance. n a a p o b m o r a n D a G i b • TAKE HOME: If neuromyotonia � Check VGKC and CASPR2 m r a a C i D 4 , 3 (Many patients with neuromyotonia are negative for both VGKC and CASPR2) 6
2/10/2017 Neuromyotonia Treatments Patient Follow-Up � Symptomatic � Initial diagnosis was stiff person syndrome � Sodium Channel Blockers � Referring Hospital � Carbamazepine, Phenytoin � Valium and IVIG prescribed � no benefit � Miscellaneous � UCSF � Dronabinol (cannabinoid) � Carbamazepine 400 mg twice daily � marked improvement � Gabapentin � PLEX � additional improvement � Immune � Outpatient – still symptomatic but not limited in his activities � In paraneoplastic form, removal of neoplasm � usually � PLEX 1.5 plasma volume x 4, repeated monthly minimal effect � CBZ 400 mg three times daily � PLEX more effective than IVIG � Azathioprine 200 mg QD � Prednisone, azathioprine Acknowledgements � Laura Rosow � Kaitlin Greene � Claire Clelland � Maulik Shah Thanks for your attention! 7
Recommend
More recommend