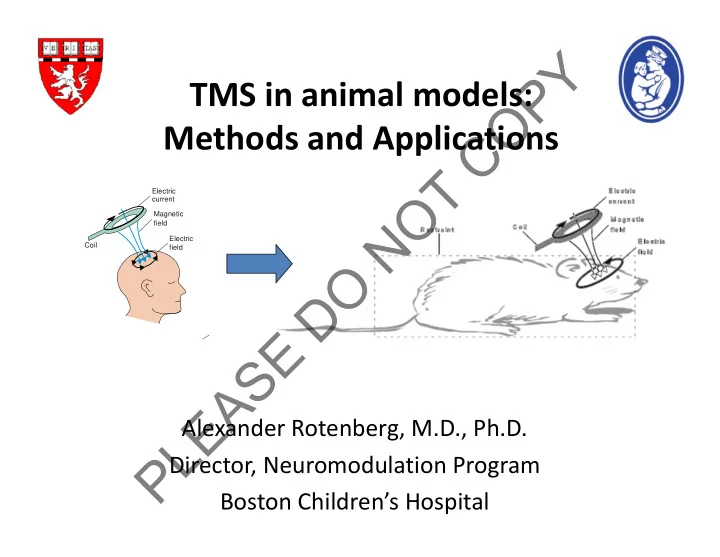
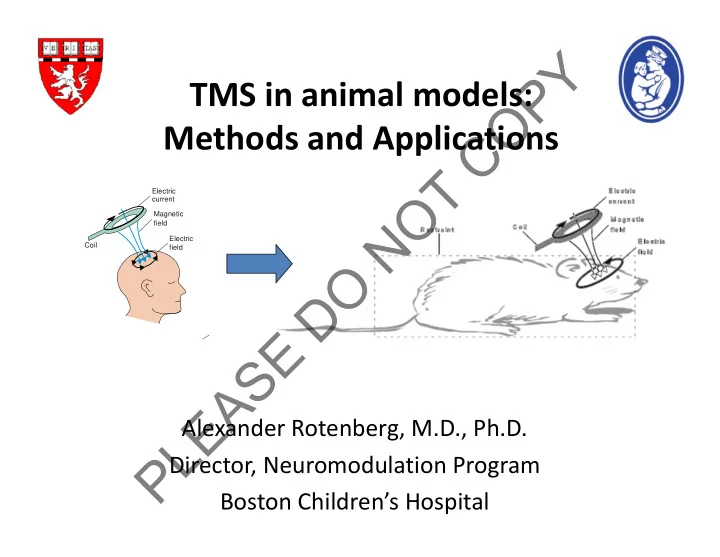
Y P TMS in animal models: O Methods and Applications C T O Electric current Magnetic N field Electric Coil field O D E S A E Alexander Rotenberg, M.D., Ph.D. L P Director, Neuromodulation Program Boston Children’s Hospital
Y TMS in animals P O C T O N O D E S A E L P
Y P Why TMS studies in animals? O C – Basic Science T O – Translational N Research O D E S A E L Poma et al., 2006 P
Y Advantages of animal subject P O C • Subject homogeneity T • Available histology O N • Genetic / disease models O D E S A E L P Liebetanz et al., 2003
Y P Translational Relevance O C • Disease modeling T O • TMS safety N • Neuronal connectivity O • Synaptic plasticity D E • Cortical organization S A E L P Charlet de Sauvage et al. 2007
Y P No injury after prolonged TMS O C • Counter, 1995: T O – No deleterious effect on AEP after 1000 pulses at 1Hz n rabbits N • Nishikiori, 1996: O – No cortical or brainstem lesions after ~1 month of daily D TMS in rabbits E • Liebetanz et al., 2003: S – No MRS or histologic changes after 5 days of 1 Hz rTMS A • Charlet de Sauvage et al., 2007 E – No DNA damage after 2000 TMS pulses L P
Induced dysfunction: neglect following Y P rTMS in cats O C T O N O D E S A E L P Valero Cabre et al., 2005
Frequency ‐ Dependent 14 C ‐ 2DG uptake Y P modulated in cat O C T O 20 Hz on-line N O D 1 Hz on-line E S A E 20 Hz off-line L P Valero-Cabre et al. 2006
Most translational research is with Y P rodents O C • Well ‐ described disease models T • Inexpensive O N • Experiments may be translated to clinical care O • TMS effect can be examined at multiple levels: D whole animal, brain slice, single cell, etc. E S Kistsen et al., in progress A E L P
Y Disadvantages of rat model P O – Compromised stimulus focality C – Slightly more difficult EEG T O – Required restraint or anesthesia N O D E S A Kamida et al., 1998 E L P Luft et al., 2001
Y Stimulation protocols P O C T O N O D E S A E L P Frye, Rotenberg, et al. Child Neurol 2007
Ground EMG Y P O C T O N EMG O D E Off ‐ Center Coil S A E Rotenberg et al., 2009 L P
Lateralized brachioradialis MEP Y P O C T O N O D E S A E L P
Y TMS in a Deployable Automated P O Anesthesia Unit (DAAU) C T O N O D E S A E L P Roteberg, Goldie, Leroy (Vivonics Inc., and Boston Children’s Hospital)
Y Proposed use: a closed loop autonomous P analgesia system O C T O N O D E S A E L P Roteberg, Goldie, Leroy (Vivonics Inc., and Boston Children’s Hospital)
Y P MEP response to propofol bolus O C 0.1 T 0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 55 57 59 O ‐ 0.1 MEP amplitude change N ‐ 0.2 (Log %baselne) O ‐ 0.3 D ‐ 0.4 E ‐ 0.5 S ‐ 0.6 A E ‐ 0.7 L ‐ 0.8 P Control 10mg 20mg Gersner et al., in progress
Y P MEP response to propofol rate change O C T Log ‐ transformed 0.2 O MEP amplitude change 0.1 N 0 (Log %baselne) 1 4 7 10 13 16 19 22 25 28 31 34 37 40 43 46 49 52 55 58 61 64 67 70 73 76 79 82 85 88 91 94 97 100 103 O ‐ 0.1 D ‐ 0.2 ‐ 0.3 E ‐ 0.4 S ‐ 0.5 A ‐ 0.6 E ‐ 0.7 L ‐ 0.8 P Control 2to1
Y Stimulation protocols P O C T O N O D E S A E L P Frye, Rotenberg, et al. Child Neurol 2007
GABAergic cortical inihibition measures Y P by paired ‐ pulse TMS (ppTMS) O C Conditioning TMS T Paired-pulse MEP inhibition 1 O Test TMS 2 N GABA-mediated O inhibition D E S A 50 ms Rotenberg and Pascual-Leone, 2010 E L P
Y P O C MMG (Mechanomyography) T O N O D E S A E L P Accelerometer
Y EMG vs MMG P O C Input–output curve of MMG 0.15 0.10 T MMG (V) 0.05 O 0.00 -0.05 50ms -0.10 N 60%MO 70%MO 80%MO 90%MO 100%MO -0.15 O D E S EMG (Tibia anterior m.) A E L P MMG
Y GABA A ‐ mediated cortical inhibition following pentobarbital (PB) P and pentylenetetrazole (PTZ) O C 200ms ISI T Saline O PB 80 * PTZ * * % of unconditioned MMG N 60 O D 40 E 20 *** *** *** S Left Right Ave (L+R) A Pre P10 P60 Pre P10 P60 Pre P10 P60 Condition E L reduced inhibition with PTZ and increased inhibition with PB P
Y TBI: The most common cause of acquired epilepsy in P young adults O C Causes of Epilepsy: T O N O D (PTE) E S A E L P Annegers JF. Lippincott Williams & Wilkins, 2001:165-72 .
Y P O C T O N O D E S A E L P
Y Fluid Percussion Injury: a post ‐ traumatic P epilepsy model O C T O N O D E S A Nature Protocols, 2011 E L P McIntosh et al., 1989
Y P Loss of cortical paired ‐ pulse inhibition after TBI O C T 200ms ISI 1.0 Sham control O * TBI N * 0.8 * ** * O * 0.6 Ratio D 0.4 E S 0.2 A E 0.0 L Pre 1WK 2WKS 3WKS 4WKS 5WKS 6WKS P Time
Y General cortical architecture is not affected by TBI P Sham control TBI (contra-lesion) TBI (lesion) O 2 4 6 2 4 6 2 4 6 NeuN I C II/III T O N V O VI D E NeuN S A E L P Hsieh et al., Cerebral Cortex 2016
Y Parvalbumin (PV) interneurons are the major P sub-type of cortical inhibitory neuron… O and vulnerable to oxidative stress C T O N O D E S A E L P Gonchar et al., 2007, Front Neuroanat.
Y Progressive PV loss after TBI P O Post-TBI (contra-lesion) Sham control Post-TBI (peri-lesion) C 2 4 2 4 6 2 4 6 6 PV I T O II/III N V O VI D Peri-lesion Contra-lesion * E *** S n.s. n.s. * *** A E L P
Y Delayed increase in oxidative stress after TBI P (8-oxo-DG) O Sham control Post-TBI (peri-lesion) Post-TBI (contra-lesion) 2 4 6 2 4 6 2 4 6 C 8-oxo-dG I T II/III O N V O VI D Peri-lesion Contra-lesion E *** n.s. ** *** n.s. S A n.s. E L P
Disruption of perineuronal nets (PNN) after TBI Y P O C T O N O D E S A E L P
Y P O C T O N O D E S A E L P
Y Ceftriaxone treatment prophylaxes against P posttraumatic seizures O C T O N O D E S A E L P
Y ppTMS as a biomarker in TBI treatment P O C T O N O D E S A E L P Hameed et al., in progress
Y Ipsilesional Parvalbumin Expression after TBI P O C T 2 weeks 4 weeks 6 weeks O N * * O D E S A E L P * p<0.05
Y Implications for Therapy P O Antioxidant C (N ‐ acetylcysteine) T Neuroprotection Oxidative stress O (Otx2) N O ↓ Otx2 ↓ Perineuronal nets Impaired inhibition D E TBI Loss of PV ‐ cells S PTE A E Epileptic seizure L P Lee et al., 2013
Y Stimulation protocols P O C T O N O D E S A E L P Frye, Rotenberg, et al. Child Neurol 2007
Y P O C T O N O D E S A E L P
Y P Rat “ deep ” TMS during seizure O C electric current T magnetic field coil O electric field N O D E EEG analysis torso strap restraints S (seizure detection) A E L P
Y rTMS during KA seizure P O C T O N O D E S A E L P Rotenberg et al., Clin Neurophys 2008
rTMS during KA seizures Y P 150% O C 125% Relative Average Seizure Duration T O (% untreated control) 100% N * O * 75% D E 50% S A 25% E L P 0% untreated active sham untreated active sham untreated active sham 0.25 Hz 0.5 Hz 0.75 Hz Rotenberg et al., 2008
Combination therapy: lorazepam + rTMS in seizure suppression Y P ½ LZP + ½ LZP ½ LZP + rTMS ½ LZP + Sham O Baseline C LZP T O 2 nd treatment N O Follow-up D 1.4 E 30 sec Normalized spike frequency (auto-count) 1.2 S ½ LZP + sham TMS ½ LZP + ½ LZP 1 A ½ LZP + rTMS 0.8 E 0.6 L 0.4 P ** *** 0.2 0 Gersner et al., 2016. 2 nd Treatment BL 1st 2nd FU Baseline LZP Follow-up
Better seizure suppression in Y P humans with 1 Hz O C % reduction in Seizure Frequency After rTMS T 150 O N 100 O D c 50 h a E n g 0 e S A E -50 L P -100 0. 3 0. 5 1 H z Rotenberg et al., unpublished data
Y Frequency ‐ response in vitro LTD P O approximates rTMS data C T O N O D E S A E L P Nakano et al., 2004
Y P Molecular Basis: Does rTMS induce LTP/LTD? O C T O N O D E S A E L P Kandel, 2001
Y Can 1 Hz TMS suppresses motor excitability P rats anesthetized with pentobarbital ? O C * T O N O 1 S1 0.5 S0.5 0.25 S0.25 Stimulation Condition (Hz) D E S A E L Reduced cortical P excitability Muller et al., PLOS One 2014
Y P O C T O N O D E S A E L P
Y P rTMS mechanisms O C T O N O D E S A E L P Kandel, 2001
Y P CREB phosphorylation by 20 Hz rTMS O C 300% T O 250% pCREB (% control) N 200% O 150% D 100% E 50% S 0% A 20 Hz rTMS Sham E L P 20 Hz rTMS Sham
Y P rTMS mechanisms O C T O N O D E S A E L P Kandel, 2001
Recommend
More recommend