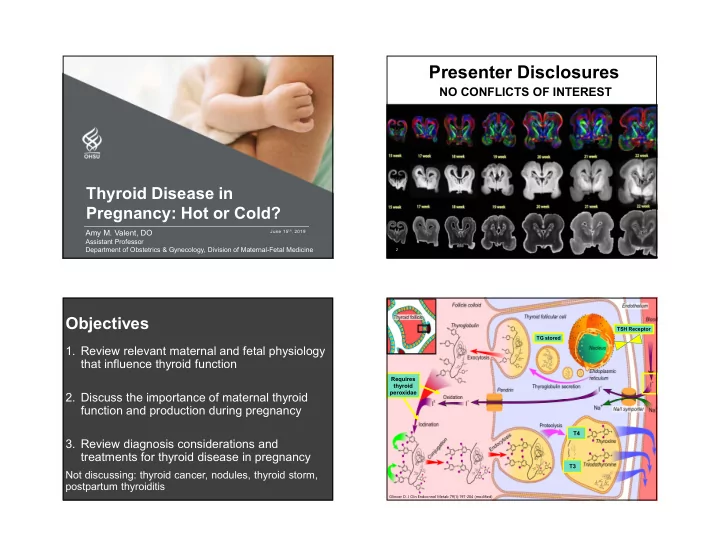
Presenter Disclosures NO CONFLICTS OF INTEREST Thyroid Disease in Pregnancy: Hot or Cold? Amy M. Valent, DO June 15 th , 2019 Assistant Professor Department of Obstetrics & Gynecology, Division of Maternal-Fetal Medicine 2 Objectives TSH Receptor TG stored 1. Review relevant maternal and fetal physiology that influence thyroid function Requires thyroid peroxidae 2. Discuss the importance of maternal thyroid function and production during pregnancy T4 3. Review diagnosis considerations and treatments for thyroid disease in pregnancy T3 Not discussing: thyroid cancer, nodules, thyroid storm, postpartum thyroiditis Glinoer D. J Clin Endocrinol Metab 79(1):197-204 (modified)
How much does iodine clearance What are the 2 main driving factors increase during pregnancy? that increase thyroid hormone? A.10-20% A. Progesterone & Estrogen B. Estrogen & hCG B.30-50% C. plasma volume & hCG C.50-70% D. GFR & plasma volume D.80% Relative Changes in Thyroid Function Pregnancy Physiology T4 Renal Iodine production excretion HCG • Pregnancy & lactation 220- 290mcg/day • 150 mcg/day through PNV (kelp? KI?) Thyroxine Placental binding deiodinases • Whole food sources : globulin Thryoid seafood, eggs, meat, and hormone production poultry • Iodinized salt • Disparities T4 fetal Iodine Fetal Plasma transfer volume transfer fetal transfer Zimmerman Paediatric and Perinatal Epidemiology.2012; 26: 108-117 Cochrane Database of Systematic Reviews 2017, Issue 3. Art.No:CD011761 8 WHO, IOM, AAP, American Thyroid Association, Endocrine Society, Teratology Society Burrow et al. NEJM. 1994 Oct 20;331(16):1072-8. Soldin et al. Thyroid. 2004 Dec;14(12):1084-90.
Hypothyroidism •Pregnancy loss •Preterm birth •Preeclampsia •Placenta abruption •Low birth weight •IUFD •Lower child IQ Haddlow JE. N Engl J Med . 1999;341(8):549-555. Casey. N Engl J Med. 2017 Mar 2;376(9):815-825. Abalovich M. Thyroid . 2002;12(1):63-68. Lazarus. N Engl J Med. 2012 Feb 9;366(6):493-50 Maraka. BMJ. 2017; 356: i6865. Who should be screened? Hyperthyroidism • Pregnancy loss ATA (2017) Endo ACOG SMFM • Preeclampsia Society (2017) (2014) • Placental abruption (2012) Universal No Yes/No No No • CHF/Thyroid storm screening • Indicated preterm birth Yes Yes Yes Yes “ High risk ” screening • Low birth weight /FGR Screening TSH TSH TSH TSH • Fetal or central hypothyroidism lab • *Fetal thyrotoxicosis TPO Ab Yes (TSH>2.5mU/L) • *Neonatal hyperthyroidism *Specifically with Grave’s Negro. J Clin Endocrinol Metab . 91(7):2587–2591 Obstet Gynecol. 2015 Apr;125(4):996-1005. JCEM. 2012; 97 (8): 2543–2565 (ATA Guidelines) Thyroid. 2017 Mar;27(3):315-389. SMFM. Contemporary OB/GYN 2012; 45-47.
Who is considered “ high risk ” ? Maternal hypothyroidism • Signs/symptoms or history of thyroid dysfunction “Maternal hypothyroidism is defined as a TSH • Goiter or +thyroid antibodies concentration elevated beyond the upper limit of • Type 1 DM or other autoimmune disorders the pregnancy-specific reference range.” • >30 years of age • Morbid obesity (BMI ≥40) Who works with a laboratory that has determined • History of miscarriage, infertility or preterm birth the population-pregnancy-specific reference • ≥2 prior pregnancies range? • History of head/neck radiation or thyroid surgery • Family history of thyroid disease What should the targets be? 2.5mIU/L & • Taking amiodarone or lithium 3.0mIU/L? 4.0mIU/L? • Residing in a moderate/severe iodine insufficient area (ATA Guidelines) Thyroid. 2017 Mar;27(3):315-389. Hypothyroid Management Diagnosis & who should we treat? Diagnosis Treatment Prepregnancy 2 additional tablets per week SC HG/SC Hypo HTX Hypo Hyper hypothyroidism ? ? ? ? ? ? Newly diagnosed TSH <4 1.2mcg/kg/day hypothyroidism TSH 4-10 1.5mcg/kg/day ↔TSH TSH ↑ TSH ↔ TSH ↑ TSH ↑↑ TSH TSH >10 2-2.5mcg/kg/day TT4* ↓TT4* ↓ TT4* ↔ TT4* ↔TT4* ↔TT4* Subclinical Hypo (ART or Goal TSH <2.5mIU/L +TPO Ab) No Yes… Yes No Yes/No Yes +TPO Ab, Euthyroid TSH q4 wks *FT4 can be checked with caution +TPO Ab, Euthyroid, h/o TSH q4 wks vs 25-50mcg/day Loss Stagnaro-Green A et al. Thyroid. 2011 Oct;21(10):1081-125 Casey. N Engl J Med. 2017 Mar 2; 376(9): 815–825. Yassa L. J Clin Endocrinol Metab, July 2010, 95(7):3234–3241 Lazarus. N Engl J Med. 2012 Feb 9;366(6):493-501 Alexander EK. N Engl J Med 2004;351:241-9. (ATA Guidelines) Thyroid. 2017 Mar;27(3):315-389. Hollowell JG. JCEM 2002:2: 489–499 Dhillon-Smith N Engl J Med 2019;380:1316-25.
Competing How is hypothyroidism best FeSO 4 , Drugs sucralfate, treated? cholestyramine Glucocorticoid Al(OH) 3 dopamine somatostatin A. Dessicated thyroid B. Methimazole C.Levothyroxine Iodide, lithium, thioamides D.Liothyronine Phenytoin, Glucocorticoids , rifampin, ipodate sodium, phenobarbital, propranolol , PTU , sertraline , amiodarone carbamazepine Which one does not cross Hyperthyroid management placenta? 1 st Trimester MMI/ 2 nd Trimester 18-22 3 rd Trimester US A.Iodine PTU vs wks findings B.Thionamides off C.TSH Ab check Polyhydramnios goiter, D.Corticosteroids HG = supportive tachycardia, bone E. Dopamine antagonists/agonists SC Hyper = hypodensity none F. Antibodies (TSI, TRAb, TPO, TG) G.T4 Active surveillance FT4/TT4 every 2-4 weeks MMI 10-30 mg daily PTU 50–300 mg daily (ATA Guidelines) Thyroid. 2017 Mar;27(3):315-389.
Take home points • Thyroid hormone has significant implications in pregnancy and the long-term neurologic health in offspring • Too much thyroid is bad • Too little thyroid is bad Thank You • Subclinical (slightly low) thyroid is… • Thyroid replacement is only as good as you take it Amy Valent (empty stomach with large glass of water for 1 hr) • Anti-thyroid medications lowest supportive dose valent@ohsu.edu • Be mindful of who you screen particularly in the first cell: 503-502-7220 TM
Recommend
More recommend