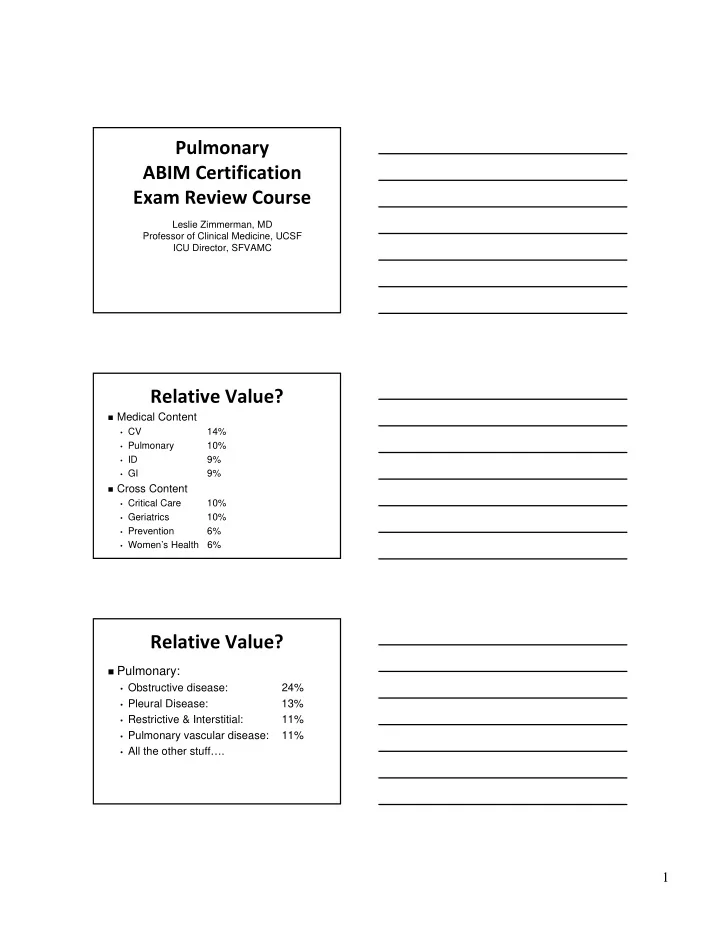
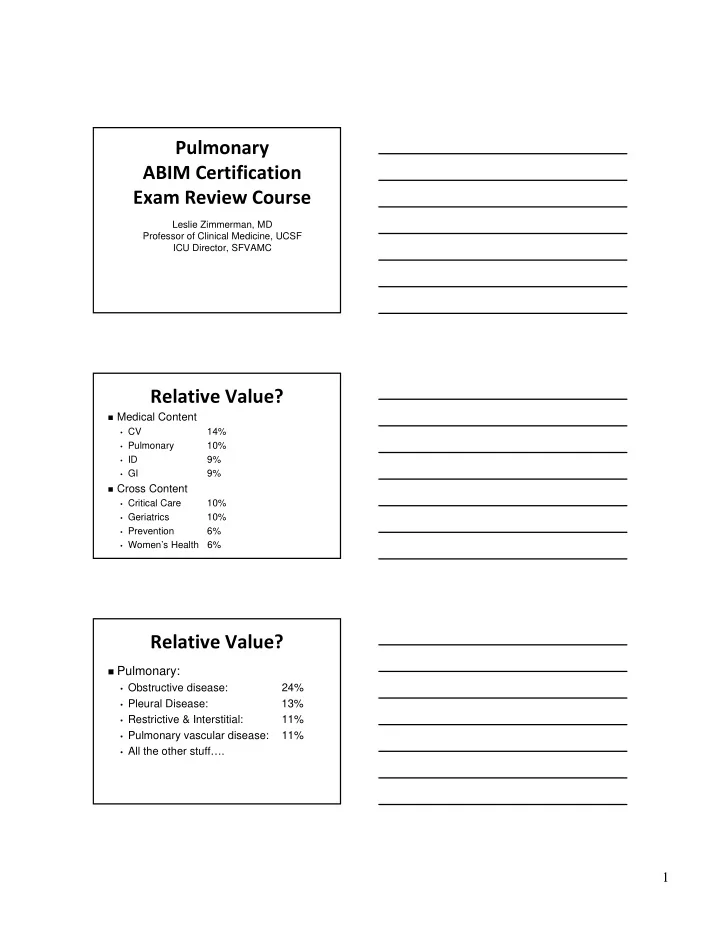
Pulmonary ABIM Certification Exam Review Course Leslie Zimmerman, MD Professor of Clinical Medicine, UCSF ICU Director, SFVAMC Relative Value? Medical Content • CV 14% • Pulmonary 10% • ID 9% • GI 9% Cross Content • Critical Care 10% • Geriatrics 10% • Prevention 6% • Women’s Health 6% Relative Value? Pulmonary: • Obstructive disease: 24% • Pleural Disease: 13% • Restrictive & Interstitial: 11% • Pulmonary vascular disease: 11% • All the other stuff…. 1
Lecture Outline Sleep COPD/Asthma ILDs PVD TB Solitary Pulmonary Nodule Etc. Question 1 A 65 year-old man with daytime sleepiness is evaluated for sleep apnea with polysomnography. His Epworth sleepiness scale is 11/24. The polysomnogram reveals obstructive sleep apnea with an apnea-hyponea index (AHI) of 12 events/hour. Lowest oxygen saturation was 86%. Treatment with continuous positive airway pressure (CPAP): Question 1 65 year-old man with 11/24 Epworth & AHI 12. O2 sat’n nadir 86%. CPAP treatment: A. Will be reimbursed by Medicare B. Will decrease cardiovascular mortality C. Will likely need to be supplemented with oxygen D. Should be offered only if “mission critical job” (airline pilot, bus and truck drivers) 2
Sleep Disorders: Office Visits www.nhlbi.nih.gov/about/factbook-05/chapter4.htm Classic patient with OSA Obesity = #1 risk factor Genetics Upper airway/facial abnormalities Post-menopause Hypothyroidism/ Acromegaly en.wikipedia.org Deeper stages of sleep, neural input to upper airway declines, decreased airway tone, tongue falls back. The vibrations from snoring may actually cause a myopathy! OSA Disruption in sleep causes daytime sleepiness Epworth Scale can estimate “sleepiness” 10 = Sleepy 18 = Very sleepy http//:epworthsleepinessscale.com 3
OSA 10 seconds 10 seconds Air flow “Hyponea” has 4% desaturation Apneas + Hyponeas = AHI OSA So can have AHI of 6-15 Severity and if asymptomatic, low Mild: AHI 5-15 Epworth, no HTN/CAD/CVA, not “mission critical” many Moderate: AHI 15-30 would not treat. Severe: > 30 AHI > 15 in everyone or Medicare reimbursement AHI > 5 if symptoms (sleepiness, fatigue, inattention) or signs of disturbed sleep (snoring, restless sleep, respiratory pauses), or HTN/CAD/CVA OSA and Death Patients with untreated mild OSA may not be at increased risk for mortality compared to individuals without OSA. IN CONTRAST : Untreated severe OSA (AHI > 30/hour) 3-6 fold increased risk of all- cause mortality compared to individuals without OSA. Marin JM et al. Lancet 2005;365(9464):1046. 4
OSA and Mortality Punjabi et al. PLoS Med. 2009 August; 6(8): e1000132 6,441 people with untreated OSA Higher CV mortality in: • Men with severe OSA (AHI > 30) who were < 70 years old • Not enough women enrolled to estimate risk Martinez-Garcia MA et a;. AJRCCM 2012;186:909 Observational, smaller (939 people) mean age 71. Even in older, untreated OSA 2x CV death if severe (AHI > 30) Question 1 65 year-old man with 11/24 Epworth & AHI 12. O2 sat’n nadir 86%. CPAP therapy: A. Will be reimbursed by Medicare B. Will decrease cardiovascular mortality If AHI > 30 C. Likely need to be supplemented with oxygen O2 alone can worsen OSA; with mild–moderate OSA & no sign’t heart/lung disease, CPAP alone typically enough D. Should be offered only if “mission critical job” (airline pilot, bus and truck drivers) AHI > 5 & symptoms treat Sleep Apnea – Cutting Edge Sharma SK et al. “CPAP for the metabolic syndrome in patients with obstructive sleep apnea” NEJM 2011; 365:2277-86. • Cross-over of sham CPAP vs. CPAP in obese patients (80% with Metabolic syndrome) with mod to severe OSA • CPAP decreased: Systolic BP 3 mmHg Diastolic BP 2.8 mmHg LDL 5 mg/dL Hgb A1c .03% 5
Sleep Apnea – Cutting Edge Karkow B,et al. “Prospective Assessment of Nocturnal Awakenings in a Case series of Treatment Seeking Chronic Insomnia patients: A Pilot Study of Subjective and Objective Causes” Sleep 2012; 35:1685-92. • Small study of insomnia patients • Most night awakenings actually caused by sleep disordered breathing What were those OSA numbers? AHI > 5 & symptoms or HTN/CAD/CVA or “mission critical” job CPAP AHI > 15 CPAP AHI > 30 and if < 70 years old, clearly at increased CV mortality if not treated (so we really encourage use!) Question 2 A 60 year-old smoker complains of an insidious onset of dyspnea on exertion. PFTS reveal COPD. The severity of the disease is determined by the: A. Air-trapping B. Diffusion capacity for carbon monoxide C. FEV1 D. FEV1/FVC E. Lack of response to bronchodilators 6
2004: Worldwide Leading Causes of Death Affects 9% of World Population By 2020, will Millions move to 3 rd leading cause of death http://www.who.int/mediacentre/factsheets/fs310_2008.pdf In US, only common disease with RISING mortality Percent Change in Age-Adjusted Death In US, in COPD Rates, US, 1965-1998 (proportion of 1965) deaths is driven by very large 3.0 CAD CVA Other COPD All in CVD Other 2.5 women. In 2000, 2.0 for 1 st time, more 1.5 women died of 1.0 COPD than men 0.5 in US. - 59% - 64% - 35% +163% - 7% 0 http://www.goldcopd.org COPD Pathogenesis: Aging + Genes + Noxious Stimuli Lung function (FEV1; alveoli) Lung Aging Healthy COPD Lung Mature Total dysfunction 18-25 years 130-140 years Chest 2009;135:173. In US, 15-20% of COPD caused in part by occupational exposures (esp. dusts) 7
In non ‐ smokers, environmental exposure is primary risk factor World Health Organization http://www.who.int/heli/risks/indoorair/en/webiapmap.jpg Indoor smoke from biomass solid fuels Contribute up to 35% of COPD in above countries Spirometry FEV1 FVC Obstructive disease TLC Restrictive disease RV Time TLC – elevated reflecting hyperinflation 8
Diffusion Capacity for CO Destroy alveoli or CO capillaries DCO: integrity of the alveolar– Low DCO capillary membrane CO CO Diffusion Capacity for CO Just narrow DCO: integrity of airways CO the alveolar– Normal DCO capillary membrane CO CO Diffusion Capacity for CO Normal Low Asthma Emphysema Fibrosis ELEVATED? Pneumocystis Diffuse alveolar jiroveci pneumonia hemorrhage PE CO Falling Hct Elevated DCO 9
Sample PFTs in emphysema FVC (L) 2.4 (52%) FEV1 (L) 1.02 (38%) Severity FEV1/FVC 41% < 70% diagnoses TLC (L) 6.2 (103%) obstruction RV (L) 3.8 (150%) Suggests DCO 12 (48%) emphysema more likely than asthma or chronic Air trapping bronchitis Question 2 A 60 year-old smoker complains of an insidious onset of dyspnea on exertion. PFTS reveal COPD. The severity of the disease is determined by the: A. Air-trapping B. Diffusion capacity for carbon monoxide C. FEV1 D. FEV1/FVC E. Lack of response to bronchodilators Consistent with emphysema; don’t stop BDs. BIG reversibility Asthma component ? COPD ‐ a different GOLD severity scale? GOLD = Global Initiative for Chronic Obstructive Lung Disease 2013 Search for Spirometry biomarkers Breathlessness Exacerbation number A = Few symptoms, OK numbers Why? B = Lots of symptoms, OK numbers C = Few symptoms, Bad numbers Why? D = Lots of symptoms, Bad numbers 10
Question 3 A 45 year-old ex-smoker with 5 years of progressive DOE has the following CXR And CT scan of Lung Bases Question 3 Testing reveals that he has very low levels of alpha-1-antitrypsin (PiZZ variant). Treatment with replacement therapy has been shown to: A. Prevent liver disease B. Decrease risk of lung cancer C. Slow decline of FEV1 D. Decrease number of exacerbations/year 11
Alpha 1 Anti ‐ trypsin Deficiency Panacinar Neutrophil A1AT Elastase Normal: PiMM Heterozygotes make enough to be protective Homozygous PiZZ, PiZnull, PiNullNull elastase unchecked early emphysema in smokers, though RARE that lifetime non- smokers get emphysema Liver Disease? A1AT made in the liver ZZ variant, it is made but can’t get out of the ER of the hepatocyte liver damage cirrhosis PiNullNull – makes NO A1AT – they do not get the liver disease IV Augmentation doesn’t help liver Augmentation with A1AT Cost is $60,000 to $150,000/ year Approved by the FDA if level below the protective level (PiZZ, PiZnull) & COPD Not in heterozygotes Not if still smoking Not if asymptomatic NIH registry: augmentation decreases rate of decline of lung function & mortality (NOT A RANDOMIZED TRIAL) 12
Question 3 Testing reveals that he has very low levels of alpha-1-antitrypsin (PiZZ variant). Treatment with replacement therapy has been shown to: Adding normal A1AT won’t hurt; but won’t help A. Prevent liver disease B. Decrease risk of lung cancer Increased risk, but no improvement with Rx C. Slow decline of FEV1 D. Decrease number of exacerbations/year “Air sac” disease, not airway disease Other COPD stuff Recurrent exacerbations are bad Lung Function Lung function over lifetime with COPD Question 4 All of the following are risk factors for COPD exacerbations EXCEPT ? A. Prior exacerbations B. Lower FEV1 C. Male sex D. History of asthma 13
Recommend
More recommend