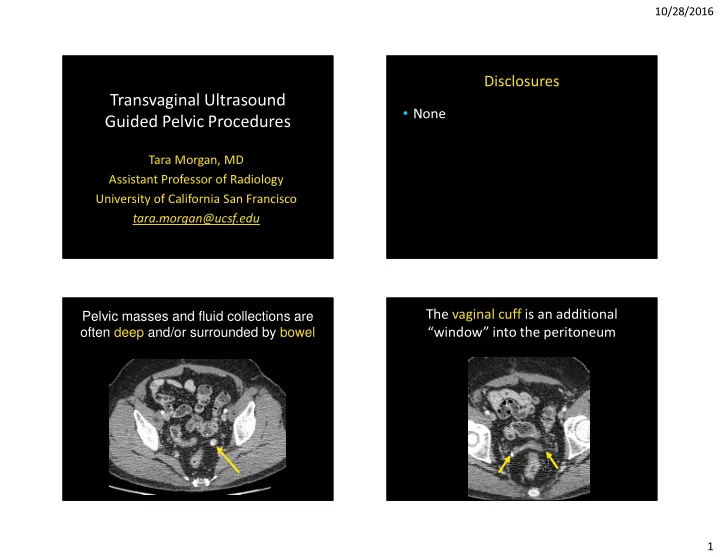
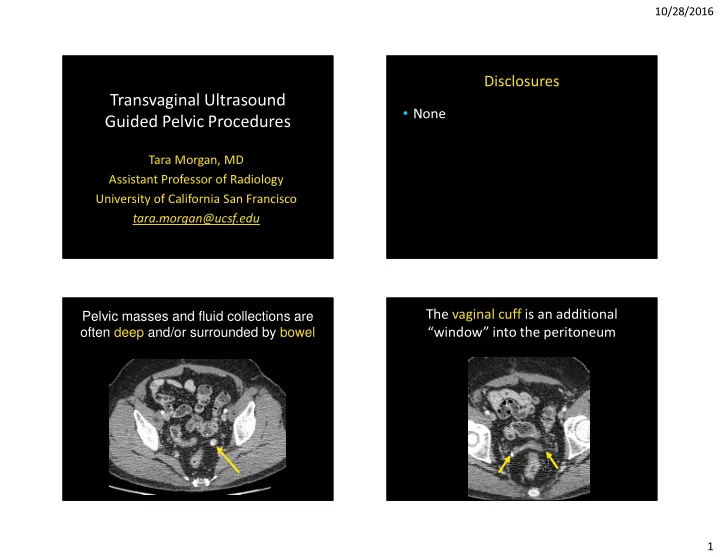
10/28/2016 Disclosures Transvaginal Ultrasound • None Guided Pelvic Procedures Tara Morgan, MD Assistant Professor of Radiology University of California San Francisco tara.morgan@ucsf.edu Pelvic masses and fluid collections are The vaginal cuff is an additional often deep and/or surrounded by bowel “window” into the peritoneum 1
10/28/2016 Transabdominal vs. Transvaginal Procedures Types • Biopsy • Aspiration Bladder • Therapeutic Injection Technique Patient Selection • Disposable • Planning is imperative endocavity • Diagnostic pelvic ultrasound prior to needle guide • Accepts up to procedure 16-18G needle • Complication rate is very low • Predictable location of the • Usually given conscious sedation needle on the image programonline.civco.com 2
10/28/2016 Biopsy Case 1 Biopsies 63 year old history mullerian adenosarcoma • Access to the cervix, uterus, vagina, posterior bladder, adnexa, parametrial/cul-de-sac • Indeterminate masses • Suspected cancer recurrence • Fine needle aspiration vs. core biopsy Biopsy Biopsy Case 1 Case 1 VC 3
10/28/2016 Biopsy Biopsy Case 1 Case 1 Recurrent Mullerian Adenosarcoma Biopsy Case 2 Biopsy 36 year old, ovarian cancer Case 2 4
10/28/2016 Biopsy Case 3 Biopsy 56 yo history of serous ovarian cancer Case 3 High grade carcinoma Biopsy Biopsy Case 4 Case 4 22 year old female with pelvic pain, referred for T2 fat sat mass T2 T1 post contrast fat sat T1 post contrast fat sat T1 5
10/28/2016 Biopsy Biopsy Case 4 Case 4 Case 4 Biopsy Case 5 Bladder Paraganglioma 64 yo pancreatic ca 7 years prior 6
10/28/2016 Biopsy Case 5 Drainage/Aspiration Metastatic pancreatic cancer • Abscess (gyn vs. non-gyn) • Hemorrhage • Ovarian/Peritoneal inclusion cyst • Serous/Mucinous Neoplasm • Diagnostic versus symptomatic • Adjunct or alternative to surgery Aspiration Case 1 Aspiration 44 yo fever and pelvic pain Case 1 7
10/28/2016 Aspiration Case 1 Aspiration Case 2 Post 24 year old, prior TOA and endometriosis T2 T1 fat sat post contrast Aspiration Aspiration Case 2 Case 2 8
10/28/2016 Aspiration Case 2 Aspiration Case 3 Recurrence required drain placement 55 yo history of vaginal cancer PET/CT Aspiration Aspiration Case 3 Case 3 9
10/28/2016 Aspiration Case 3 Therapeutic Injection Post • Intra-amniotic injection for ectopic pregnancy • Treatment of AVM, fistula R squamous cell, L benign Therapeutic Injection Case 1 Transvaginal Methotrexate Injection C-Section Ectopic 10
10/28/2016 Therapeutic Injection Case 2 Therapeutic Injection 23 yo old, s/p D&C and uterine septum Case 2 removal, AVF ++bleeding T1 post contrast fat sat Therapeutic Injection Therapeutic Injection Case 2 Case 2 11
10/28/2016 Therapeutic Injection Therapeutic Injection Case 2 Case 2 Arteriogram of the uterus T1 post contrast fat sat Pitfall Case 1 Pitfalls 23 year old RLQ pain • Poor screening tool BL • Prior radiation/scar tissue • Pelvic ascites • Technical factors – Soft masses/collections – Bladder prolapse – Introduction of air T2 T1 post contrast fat sat 12
10/28/2016 Pitfall Case 1 Pitfall Case 1 Soft Mass Pitfall Case 3 Pitfall Case 2 40 year old with hx cervical cancer, Pelvic Ascites/Fine Cystic Mass ?infection vs recurrence 13
10/28/2016 Pitfall Case 3 Pitfall 2 months later Case 3 Pitfall Case 3 Conclusion Missed Recurrence • Transvaginal ultrasound is a great method to access deep pelvic lesions • Procedures include biopsy, aspiration, and therapeutic injection • Some technical limitations can occur 14
10/28/2016 1) Transvaginal ultrasound has which advantage over CT? Ultrasound A. Better screening/surveillance for metastatic disease 97% B. Larger field of view C. Superior resolution of pelvic structures D. Better visualization of bone 3% 0% 0% 0% Pyosalpinx w . e E. Better visualization through gas e . n . . . o . . v i e . . l l p b o i f e o f f r v o o h t r d n n u l n s e o o / i i i o f t t i g u a t n e r z a filled structures i o l i z n g l i r s a l e a e a e u u r L r s c r i s o v v i s r i r r e e r e t e t p t t t u e t e e B S B B 2) What finding may compromise 3) How could this lesion best be safety of a transvaginal ultrasound sampled for diagnosis? • A) Transvaginally guided biopsy? with ultrasound • B) Ultrasound 59% A. Prior hysterectomy guided percutaneous B. Empty bladder • C) CT guided 34% C. Pelvic Infection percutaneous • D) No safe access D. Pelvic Ascites with CT or 3% 3% E. EPrior radiation 1% ultrasound • E) Cystic and can not s y r n e n m e o o d t t i i i o d c t t a c s a c e A i e b l f d 33 yo with hx of ovarian n c a r e y I v i r t t c s p i e l r y v o m l P i h e r be sampled E P r P o E r i P cancer 15
10/28/2016 Percutaneous Approach Transvaginal Vaginal Cuff Transabdominal US Recurrent low serous carcinoma Tara.morgan@ucsf.edu 16
Recommend
More recommend