Vascular Ultrasound Kim Kargaard Bredahl, MD, Ph.D Background - PowerPoint PPT Presentation
Vascular Ultrasound Kim Kargaard Bredahl, MD, Ph.D Background Resident in vascular surgery Vascular ultrasound on a daily basis Stenosis Flow measurement Aneurysms (size) Ph.d thesis 3D and contrast-enhanced ultrasound in
Doppler angle θ f d = f 0 – f 1 = (2 x V x f 0 x cos ) / C Error in velocity % When calculating the velocity (V) 100 the angle estimation is very important – especially when > 60 . Example: Overestimating the angle by 5 • at 40 leads to an error of 7%. 10 • at 75 leads to an error of 47% ! 30 60 80 0 Conclusion: Keep the angel < 60 ! Degrees kimbredahl79@gmail.com
Volume measurement - Doppler gain Too low gain → flow High gain → overloading of the The ideal gain level may not be detected instrument → poor direction discrimination PSV and TAMV increase PSV and TAMV decrease Ideal image Mirror image kimbredahl79@gmail.com
Cross section Area = π . ¼ . D² The error is 0.084 cm or less than 1 mm. or 11 % The corresponding failure in vol flow is 21 % going from 459 mL to 362 mL kimbredahl79@gmail.com
Diameter assessment and Image resolution L9-3 MHz L17-5 MHz No intima Intima For superficial structures take the transducer with the highest frequency available kimbredahl79@gmail.com
Diameter assessment – when to measure Cardiac cycle kimbredahl79@gmail.com
Cardiac cycle Upper LoA =4.7 mm Average 1, 94 mm kimbredahl79@gmail.com
Challenges in systoly Frame rate = 18 Diameter forskel 1 sekund Tid By Henrik Sillesen kimbredahl79@gmail.com
Cursor position 2-6 mm. Difference! kimbredahl79@gmail.com
Diameter assessment – where to measure The true volume flow The most reproducible From intima to intima measurement Taken the concept of acoustic impedance into account the ideal measurement would be from the most reproducible measurement is from leading edge adventitia ant. wall to leading edge adventitia posterior wall kimbredahl79@gmail.com
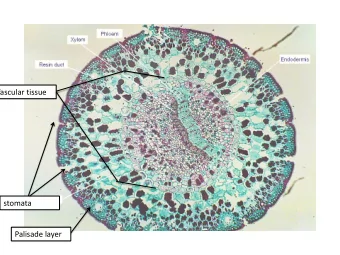
Karvæggen Leading edge of adventitia – anterior wall Tunica media Grænsen mellem tunica media og tunica adventitia Lumen Leading edge of intima kimbredahl79@gmail.com
Cursor position Leading edge of adventitia Leading edge of intima kimbredahl79@gmail.com
Cursor position kimbredahl79@gmail.com
Volume flow and other pitfalls Not all vessels are circular Most scanners assume the mean Medium Speed (C) (m/s) Velocity of sound is 1540 m/s Air 330 Water 1480 → Systematic underestimation of the Blood 1570 Diameter Fat 1450 Muscle 1580 Bone 3500 Soft tissue 1540 (average) kimbredahl79@gmail.com
Ultrasound Contrast media • Microbubbles ≈ Red blood cells. – Small enough to pass through the capillaries – Large enough to retain in the vascular system • Blood pool agent → Indicator dilution principal with a wah Gas SF 6 Amphophilic shell Poor -Stabilizes the gas interaction -Flexible molecule with other molecules – Completely pulmonary eliminated
Contrast specific imaging • Insonation power Low pressure High pressure Oscillation Instability → destruction Backscatter -Harmonic frequency -Specific signals ≠ Tissue signal = Tissue Signal
Contrast specific imaging • In summary – Specific echo signal different from tissue • No tissue signals • No movement artifacts and blooming effects – Independent from blood flow velocity • No angle dependent color display • Better spatial resolution • Detect low flow – Good safety profile • No burden for the liver or kidneys • Allergic reactions are rare
In practice • High end scanner with a contrast specific application • SonoVue – 20 gauge cannula – Forward injection in a cubital vein. – 1-2 ml. – Last 6 hours after mixture. – Anti-histamin and adrenalin.
Contrast-enhanced ultrasound • If microvascular perfusion is important. – Diabetic patients • If luminal morphology is important – Plaque size and neovascularization – Thrombus size estimation – Near occlusion / complete occlusion – Flow detection
Microvasculature C. Greis / Ultrasound contrast agents as markers of vascularity and microcirculation
Healthy volunteer Peripheral arterial disease Lindner JR, Portland, Oregon. JACC: Cardiovascular imaging 2008
Flow detection kimbredahl79@gmail.com
Tasks for practical sessions • Doppler Ultrasound – Control colour box • Size and position • Steering – Pulse repetition frequency • Low and high – find the right level – Spectral analysis • Adjust size of sample volume • Obtain Doppler angle < 60 degrees – Extra option ”Walk the Doppler” from CFA to PFA.
Repetition - If I want to do it right ☺ 1. The right transducer: curved phased or linear array transducer 2. Adjust your B-mode image -Depth -Focal zone Field of -Gain level view 3. Apply colour Doppler image -Tilt the transducer or adjust steering level -Pulse repetition frequency level
Repetition - If I want to do it right ☺ Flow direction 4. Spectral Doppler analysis - Parallel to flow direction Beam path and keep the angle to the Beam path < 60 º
The practical sessions 5. Be correctly seated and your right should work independently. Don’t look down! Keep eye on the road (Keyboard). And your left hand is as important as your right hand.
If you want to know more • Vascular ultrasound How, why and when – Edited by Abigail Thrush and Tim Hartshorne • Quantitative evaluation of microvascular blood flow by contrast-enhanced ultrasound by C. Greis. Clinical Hemorheology and Microcirculation 49 (2011) 137-149 • Pubmed: Eiken FL et al. Diagnostic methods for measurement of peripheral blood flow during exercise in patients with type II diabetes and peripheral artery disease: a systematic review
Practical stuff kimbredahl79@gmail.com
Transducer Low-frequency High-frequency - Marking on the left by your thumb - Towards the heart or cranial (carotid)
Transducer Handheld Fingercontr ol
Transducer
Transducer
Brightness-mode Machinery CD Player – do you Receiver Loudspeake remember it? r Raw Amplificatio data n
Ultrasound equipment in short – two unit model Transducer Displaye d Filtered and amplified Received informatio n Mechanica l energy Tissue
Brightness-mode – 3 buttons!!! Raw data Volume = gain → 2D button Optimal gain level = some echo signal insight the vessel
Brightness-mode 2. and 3. button Adjust the depth of your scanfield Region of interest: at least 1/3 of the scan field If you can get close it is good ☺
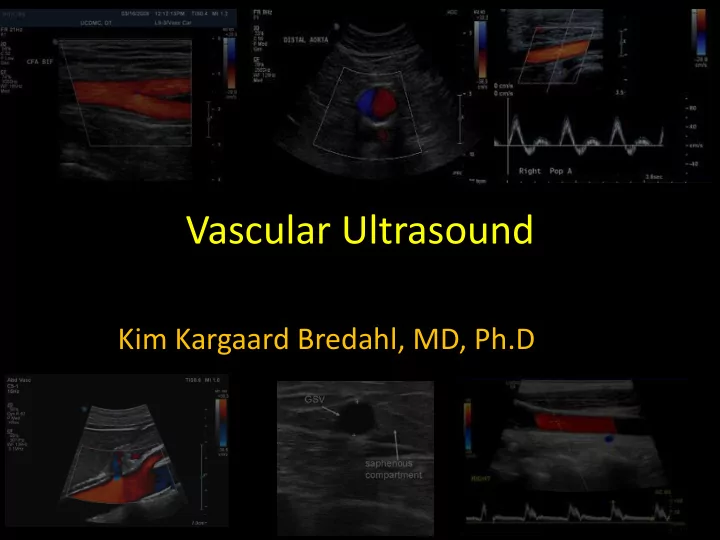
Ultrasound imaging – What can be displayed Brightness mode (B- mode) also called grey- scale imaging -Morphology Doppler Ultrasound - Dynamics Spectral analysis Colour
Linear velocity is Spectral analysis displayed on the vertical – axis (cm/s) Tim e Proportion of blood cells at a particular speed along the third axis – brightness of the display Vessel Flow towards the transducer will displayed as positive Flow away from the transducer will displayed as negative
Colour Doppler • B-mode image with • Colour coded Doppler signals in the steering-box In this example: Blood flow towards the transducer is coded red Heart Foot Blood flow away from the transducer is coded blue
Colour Doppler Tilting or steering θ
Colour Doppler Sin ( θ) Remember! The Doppler shift is based on Doppler equation where cosinus function is included, and 0 1 Cos ( θ ) cosinus to 90 degree is zero SFA External Iliac artery
Colour Doppler Remember! The pulse repetition frequency is important in order to visualize blood-flow. Low PRF too high PRF too low flow If the speed is high – you have to watch every second Growth of a tree cannot be observed by watching every second!
Display of Colour Doppler and spectrum Angle θ Beam path (Steer) Sample Volume Colour Framerat scale e Peak systolic velocity Doppler Angle θ Doppler angle Correction curser Mean Distance velocity Colour Box
If the Doppler waveform doesn’t look right Sup. Fem. Sup. Fem. artery artery
Tasks for practical sessions • Doppler Ultrasound – Control colour box • Size and position • Steering – Pulse repetition frequency • Low and high – find the right level – Spectral analysis • Adjust size of sample volume • Obtain Doppler angle < 60 degrees – Extra option ”Walk the Doppler” from CFA to PFA.
Repetition - If I want to do it right ☺ 1. The right transducer: curved phased or linear array transducer 2. Adjust your B-mode image -Depth -Focal zone Field of -Gain level view 3. Apply colour Doppler image -Tilt the transducer or adjust steering level -Pulse repetition frequency level
Repetition - If I want to do it right ☺ Flow direction 4. Spectral Doppler analysis - Parallel to flow direction Beam path and keep the angle to the Beam path < 60 º
The practical sessions 5. Be correctly seated and your right hand works independently. Don’t look down! Keep eye on the road (Keyboard). And your left hand is as important as your right hand.
Contents • The clinical use of ultrasound in vascular surgery • From sound to image – theory 10 min. • Doppler effect / doppler shift – Displaying the doppler signal – Flow profiles • Colour doppler • Volume measurement – Pitfalls • Hands on session kimbredahl79@gmail.com
Ischemic disease • Patient’s complaint • Objective – Peripheral blood pressure – Dynamic flow visualization • Linear flow velocities • Flow pattern kimbredahl79@gmail.com
Aneurysm size or mophology Accuracy is important Standard protocol is pivotal -Cardiac cycle -Delineation of the vessel wall -Image plan; 3D ultrasound • Ultrasound contrast – Morphology • Thrombus or plaque size – delineates the lumen/thrombus kimbredahl79@gmail.com
Leakage • Flow detection • Ultrasound contrast – Low flow – Microperfusion kimbredahl79@gmail.com
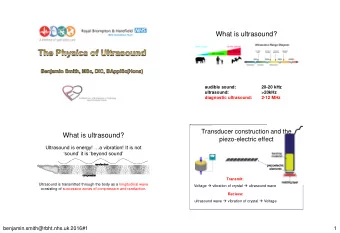
Ultrasound = High frequency sound that induces local periodic displacement of particles in the medium Transducer off Transducer on Displacement Depth λ Frequency ( f ) = 1/ τ, number of cycles of displacements during 1 second (Hz) . Medical ultrasound scanner typically use frequencies between 2 – 15 MHz kimbredahl79@gmail.com
Doppler-effect f d = f r – f t = ( 2 x V x f t x Cos θ) / C : Angle of insonation C: Speed of sound in tissue (1540 m/s) V : Velocity of blood Transducer f r : Receiving frequency f t : Transmitted frequency Transmitting Piezo-electro element elements Receiving element Gel Transducer = stationary source Red cells = moving source, Red cells = Moving observer. Transducer = stationary observer θ kimbredahl79@gmail.com
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.