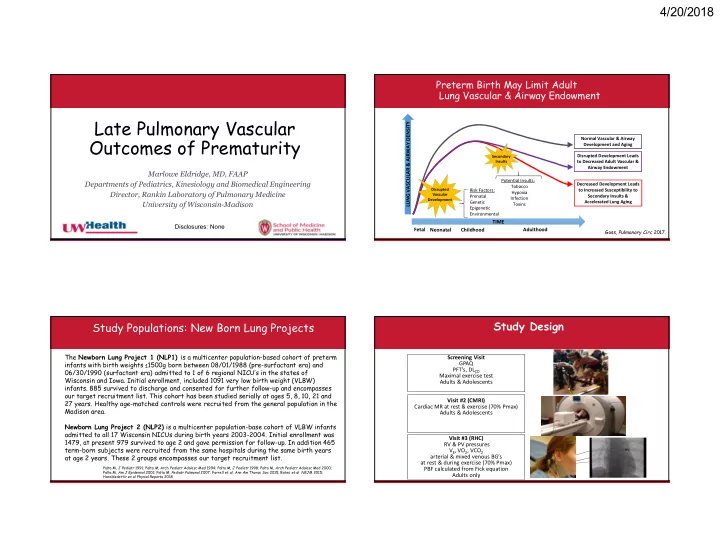
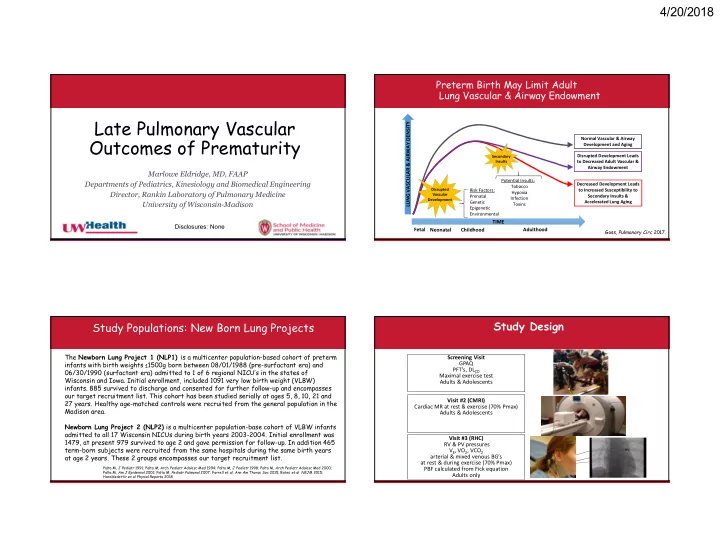
4/20/2018 Preterm Birth May Limit Adult Lung Vascular & Airway Endowment Late Pulmonary Vascular LUNG VASCULAR & AIRWAY DENSITY Outcomes of Prematurity Normal Vascular & Airway Development and Aging Disrupted Development Leads Secondary Insults to Decreased Adult Vascular & Airway Endowment Marlowe Eldridge, MD, FAAP Potential Insults: Departments of Pediatrics, Kinesiology and Biomedical Engineering Decreased Development Leads Tobacco Disrupted Risk Factors: to Increased Susceptibility to Director, Rankin Laboratory of Pulmonary Medicine Hypoxia Vascular Prenatal Secondary Insults & Infection Development Genetic Accelerated Lung Aging University of Wisconsin-Madison Toxins Epigenetic Environmental TIME Disclosures: None Fetal Neonatal Childhood Adulthood Goss, Pulmonary Circ 2017. Study Design Study Populations: New Born Lung Projects The Newborn Lung Project 1 (NLP1) is a multicenter population-based cohort of preterm Screening Visit infants with birth weights ≤1500g born between 08/01/1988 (pre-surfactant era) and GPAQ PFT’s, DL CO 06/30/1990 (surfactant era) admitted to 1 of 6 regional NICU’s in the states of Maximal exercise test Wisconsin and Iowa. Initial enrollment, included 1091 very low birth weight (VLBW) Adults & Adolescents infants. 885 survived to discharge and consented for further follow-up and encompasses our target recruitment list. This cohort has been studied serially at ages 5, 8, 10, 21 and Visit #2 (CMRI) 27 years. Healthy age-matched controls were recruited from the general population in the Cardiac MR at rest & exercise (70% Pmax) Madison area. Adults & Adolescents Newborn Lung Project 2 (NLP2) is a multicenter population-base cohort of VLBW infants admitted to all 17 Wisconsin NICUs during birth years 2003-2004. Initial enrollment was Visit #3 (RHC) 1479, at present 979 survived to age 2 and gave permission for follow-up. In addition 465 PA RV & PV pressures term-born subjects were recruited from the same hospitals during the same birth years V E , VO 2 , VCO 2 RV at age 2 years. These 2 groups encompasses our target recruitment list. arterial & mixed venous BG’s Sheeth at rest & during exercise (70% Pmax) Palta M, J Pediatr 1991; Palta M, Arch Pediatr Adolesc Med 1994; Palta M, J Pediatr 1998; Palta M, Arch Pediatr Adolesc Med 2000; PBF calculated from Fick equation Palta M, Am J Epidemiol 2001; Palta M, Pediatr Pulmonol 2007; Farrell et al, Ann Am Thorac Soc 2015; Bates et al NEJM 2015; Adults only Haraldsdottir et al Physiol Reports 2018 1
4/20/2018 Anthropometric & Pulmonary Function Data Exercise Capacity Term Preterm Term Preterm P value P value N=10 N=11 N=10 N=11 Exercise Testing Anthropometric Data Age (years) 26.3 ± 0.9 27.3 ± 0.8 0.02 VO 2max (L/min) 3.5 ± 0.7 2.6 ± 0.6 0.005 Arij Beshish, Arij Beshish, Sex (M/F) 7/3 5/6 0.26 – % predicted 135.5 ± 31.7 112.4 ±3 7.0 0.17 MBBCh, PhD MBBCh, PhD Weight (kg) 72.8 ± 9.8 69.3 ± 13.3 0.45 VO 2max (ml/kg/min) 50.0 ± 10.4 38.1 ± 8.6 0.01 Height (cm) 176.6 ± 7.8 170.0 ± 11.3 0.23 P max (watts) 236.5 ± 48.9 187.7 ± 36.0 0.02 BMI (kg/m 2 ) 23.3 ± 1.7 23.9 ± 3.0 0.66 P max at 70% VO 2max (watts) 172.8 ± 31.5 130.5 ± 24.6 0.005 Pulmonary Function Testing GPAQ (MET/week) 3368 ± 2550 3420 ± 2006 0.79 FVC (L) 5.4 ± 1.1 4.7 ± 0.7 0.16 – % predicted 103.8 ± 13.2 103.8 ± 16.6 0.73 FEV 1 (L) 4.5 ± 1.0 3.8 ± 0.7 0.11 – % predicted 101.9 ± 15.1 99.1 ± 20.1 0.37 FEF 25-75 (L/s) 4.5 ± 1.6 3.6 ± 1.2 0.24 – % predicted 98.3 ± 30.3 87.6 ± 32.6 0.45 FEV 1 /FVC 0.82 ± 0.06 0.80 ± 0.06 0.73 DL CO (ml/min/Torr) 32.4 ± 6.5 24.4 ± 4.3 0.004 – % predicted 97.8 ± 9.1 81.5 ± 6.4 <0.001 DL CO /V A (ml/min/Torr/L) 5.6 ± 0.8 4.7 ± 0.4 0.002 Goss et al AJRCCM , in review, 2018 Females Males Females – % predicted 113.3 ± 18.0 96.3 ± 8.9 0.01 Males Farrell et al AATS , 2015 Adults Born Premature Have Elevated Neonatal Characteristics Resting Pulmonary Vascular Pressures Neonatal Characteristics N (males) 11(5) Arij Beshish, Gestational age (weeks) 28.6 ± 2.7 (24 – 31) MBBCh, PhD Birth weight (grams) 1087 ± 297 (675 – 1497) Arij Beshish, MBBCh, PhD Apgar score at 1 minute 3 ± 2 Apgar score at 6 minutes 6 ± 2 Singleton/multiple birth 5/6 Received antenatal steroids 0 sPAP (mmHg) mPAP (mmHg) dPAP (mmHg) Intubated at 24 hours of age 9/2 (yes/no) Received surfactant (yes/no) 2/9 Days of invasive ventilation 15.5 ± 17.7 (0 – 50) Days of noninvasive ventilation 3.9 ± 6.5 (0 – 22) Days on oxygen 93 ± 150 (1 – 514) Days in the NICU 64 ± 30 (33 – 107) BPD diagnosis at discharge (yes/no) 5/6 Persistent PDA (yes/no) 7/4 Goss et al AJRCCM , Diagnosis of PH by echo in NICU 0 In review, 2018 Goss et al AJRCCM , in review, 2018 2
4/20/2018 Adults Born Premature have a Preterm subjects continue to have higher afterload Stiffer Pulmonary Vascular Bed and stiffer PA in response to exercise Arij Beshish, (mPAP/PBF) (mPAP/SV) Arij Beshish, MBBCh, PhD MBBCh, PhD Goss et al AJRCCM , in review, 2018 Adults Born Premature Unable to Adolescents Born Preterm have similar Augment Stroke Volume During Exercise Cardiac Dysfunction Kristin Haraldsdottir,MS Arij Beshish, MBBCh, PhD Goss et al AJRCCM , in review, 2018 Haraldsdottir et al Pediatrics in review 2018 3
4/20/2018 Neonatal Days on Ventilatory Support is Pressure / Flow Relationships during Exercise Strongest Predictor of Adult PAP Arij Beshish, Arij Beshish, MBBCh, PhD MBBCh, PhD Left: Cardiac output (CO) versus mean pulmonary artery pressure (mPAP) demonstrates a greater pulmonary vascular resistance (slope) for a given volume of pulmonary flow among preterm subjects. Right: Systolic right ventricular pressure (sRVP) versus stroke volume (SV) demonstrates a lower Goss et al AJRCCM , volume ejected for any RV pressure among preterm subjects. in review, 2018 Goss et al AJRCCM , in review, 2018 Shorter Mean Transit Time in Adults Born Preterm PC VIPR or 4D Flow further supports stiffer pulmonary vascular bed ( phase contrast vastly-undersampled isotropic projection) Kevin Johnson PhD UW Med Physics Luis Torres * PA PA SVC SVC RA RA RV RV Pulmonary Blood Flow (PBF) and Mean Transit Time (MTT) in term and preterm populations IVC IVC indicate significantly shorter MTT (* p<0.02). Suggest stiff pulmonary vascular bed in preterm’s. May also suggest vascular simplification. PC VIPR is a UW-developed 4D phase contrast technique that extends flow encoding from 1 dimension to 3 dimensions. 4
4/20/2018 Cardiac Flow Is Less Laminar Further evidence for a stiffer pulmonary vascular beds in adults born preterm in Adults Born Preterm Term Preterm Jacob Macdonald Term Preterm Pulmonary Artery Relative Area Change 0.45 * Relative area (%) 0.40 0.35 Male, 0.30 Male, GA 25 wks PA 23/10 (mPAP 15) Male, GA 40 wks Male, GA 25 wks PA 30/19 (mPAP 23) 0.25 PA 23/10 (mPAP 15 ) PA 30/19 (mPAP 23) 0.20 Term Preterm RV Filling Vortex Is Less Structured RV Filling Vortex Is Less Structured in Adults Born Preterm in Adults Born Preterm Term Preterm Term Preterm Jacob Macdonald Jacob Macdonald 5
4/20/2018 RV Energetically Less Efficient Representative image of the determination of in Adults Born Preterm right ventricular circumferential strain Jacob Macdonald Total kinetic energy in the RV was normalized by each subject’s stroke volume Greg Barton, PhD to evaluate energetic efficiency Macdonald et al J Cardiovascular MR 2018, in review Strain based analysis further supports Adults Born Preterm have greater RV strain decreased RV efficiency suggesting a hyperdynamic RV Greg Barton, PhD Greg Barton, PhD Preterms require a greater proportion of the cardiac cycle to reach peak systolic strain (45% vs 35%). During diastole, preterm demonstrate greater diastolic strain suggestive of altered relaxation kinetics or increased myocardial stiffness . 6
4/20/2018 Summary: Cardiopulmonary Impairment in Acknowledgements Adults Born Premature Enthusiastic human subjects Heart & Lung Imaging Core • Adults born premature have: Oliver Wieban, PhD (Medical Physics) Key Collaborators Sean Fain, PhD (Medical Physics) Kara Goss MD (Medicine & Pediatrics) Chris François, MD (Radiology) • Mild elevations in pulmonary arterial pressure Mari Palta PhD (NLP, Biostatistics) Scott Nagle, MD, PhD (Radiology) Luke Lamars MD (Pediatrics) Kevin Johnson, PhD (Medical Physics) • Stiffer pulmonary vascular bed Research Scientist Naomi Chesler PhD, Biomedical Engineering Emily Farrell, PhD (Pediatrics) • Impaired cardiac response to exercise (SV limitation) Ruedi Braun PhD (pediatrics) Funding: Jens Eickhoff, PhD (Biostatistics) NIH-NHLBI, RO1 HL086897 (Eldridge) • Evidence of diastolic dysfunction Pre & Post-Doctoral Trainees NIH-NHLBI RO1 HL115061 (Eldridge) Arij Beshish, MBBCh, PhD (Pediatrics & Physiology) NIH-NHLBI RO1 HL115061-03:Suppl (Eldridge/Goss) • Reduced RV efficiency Kristin Haraldsdottir, MS (Pediatrics & Kinesiology) Laura Tetri, PhD (MD/PhD Program) CTSA grant UL1TR000427 (Goss:KL2) Jacob McDonald, BS (Medical Physics) PHA Barst Award (Goss) Luis Torres, BS (Medical Physics) Parker B. Francis Fellowship (Goss) Ashley Mulchrone, BS (Biomedical Engineering) Greg Barton, PhD (Pediatrics & Medical Physics) Technical Support David Pegelow, BS (Pediatrics) Army of Graduate Students Questions / Comments Hybrid cardiac PET/MR 7
Recommend
More recommend