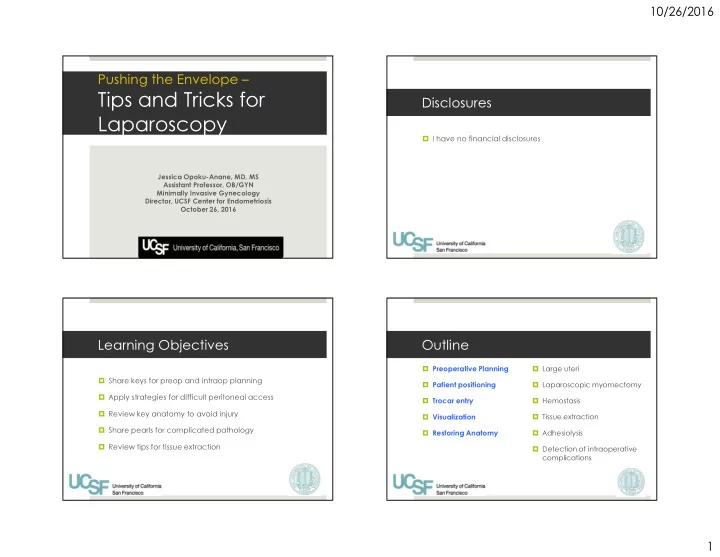
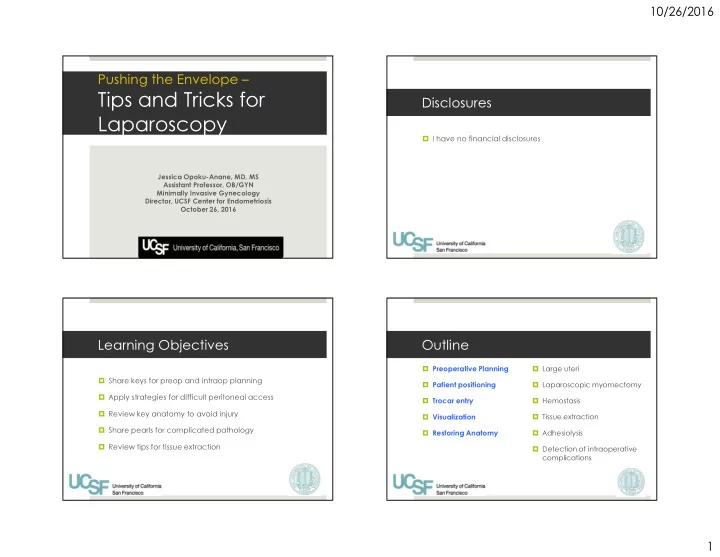
10/26/2016 Pushing the Envelope – Tips and Tricks for Disclosures Laparoscopy � I have no financial disclosures Jessica Opoku-Anane, MD, MS Assistant Professor, OB/GYN Minimally Invasive Gynecology Director, UCSF Center for Endometriosis October 26, 2016 Learning Objectives Outline � Preoperative Planning � Large uteri � Share keys for preop and intraop planning � Laparoscopic myomectomy � Patient positioning � Apply strategies for difficult peritoneal access � Trocar entry � Hemostasis � Review key anatomy to avoid injury � Visualization � Tissue extraction � Share pearls for complicated pathology � Restoring Anatomy � Adhesiolysis � Review tips for tissue extraction � Detection of intraoperative complications 1
10/26/2016 Outline Preoperative Planning – High Risk Patients � Preoperative Planning � Large uteri � Patient positioning � Laparoscopic myomectomy � Prior laparotomy or known adhesive disease � Trocar entry � Hemostasis � Advanced endometriosis � Visualization � Tissue extraction � Large pelvic/abdominal pathology � Restoring Anatomy � Adhesiolysis � Infections (PID/TOA, diverticulitis) � Detection of Intraoperative � Obesity complications � Very thin patients � Pregnancy Patient positioning Trocar Entry • Lateral to avoid inferior � Arms tucked at side epigastrics � Dorsal lithotomy • 20-25 mmHg � Gel/foam pad • LUQ entry • Direct visualization of ancillary trocars 2
10/26/2016 Preoperative Assessment of Risk of Adhesive Disease Adhesions Omental and/or Bowel � H&P including rectal Prior surgical scar � Prior operative notes Pfannensteil–27% � Ultrasound � Visceral slide test Low vertical–55% High vertical–67% Brill. Obstet Gynecol. 1995;85:299. Palmer’s Point Palmer’s Point Technique � Closed Veress technique � Relative CI � 5 mm incision 3 cm below left costal � Prior gastric bypass or splenectomy margin in the mid clavicular line � LUQ mass � Heaptosplenomegaly � OG tube Tulikangas. Fertil Steril. 2003;79:411-2 3
10/26/2016 Visualization Know your anatomy! � Retroperitoneal dissection � Identification of the ureters � Uterine manipulator � 0, 30, 45 degree scopes � Ovarian, bowel, or uterine pexy � Keith needle, curved needle, T-lift � Restoring anatomy Courtesy of Astrid Von Walter Large Uteri Large Uteri Hysterectomy � Pre-operative Lupron � Uterine manipulator and colpotomy cup � Suprapubic port � Hand assist � Peritoneal window in the broad ligament � Stay close to the ovary � Desiccate both sides before transection of UA 4
10/26/2016 Laparoscopic myomectomy - Hemostasis Avoiding hemorrhage � Vasopressin (0.05-0.3 U/ml) � Hemostatic agents � 20 U in 200 ml � Laparoscopic pericervical tourniquets � Coagulation � Misoprostol � Bupivacaine plus epinephrine � Vascular Clips � Gelatin-thrombin matrix � Tranexamic acid � Thermal energy � Cell saver � Laparoscopic bulldog clamps � Suture � IP ligament � Pressure – clamping, gauze, etc. � UO ligament Cochrane - Kongnyuy 2014 On Op-Ed in the Philadelphia Inquirer 3/16/14 by Hooman Noorchashm Petition Organizer As a surgeon, I have seen an overt emphasis on marketing and enhancement of the volume of practice and, thus, revenue flow. But the cost of this emphasis on the business of medicine seems to be an inability to empathetically, carefully, and self- critically look at the devastating complications we cause. When empathy is gone, the self-criticism that comes along with it is also history. Given that reality, it is easy to see how purely utilitarian arguments can take hold of an establishment's ethical reasoning. Specimen Removal 5
10/26/2016 Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication POLL A) Power morcellation � April 17, 2014 B) Mechanical morcellation � Risk of Sarcoma 1/352, Risk of LMS 1/498 � No way to predict sarcoma pre-operatively C) Morcellation in a bag only � “FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy D) No morcellation for uterine fibroids.” E) Enjoy tissue extraction Slide adapted from Ashkins, Power Morcellation in Gyn Surgery; Established Trend & New Controversy Presentation, Holy Cross 5/2014 Specimen Removal Manuel morcellation in a bag - Extraction Sites � 2.5 cm abdominal � Umbilicus � Suprapubic � Lower lateral port � Alexis wound retractor � Paper roll/”C” technique 6
10/26/2016 Power morcellation in a bag Vaginal morcellation in a bag Specimen Removal – tips for bagging Adhesiolysis � Types of bags � Steps: � Deployable bags if possible! - � Specimen in upper abdomen � Uterine manipulator and/or up to 15 cm rectal probe � Introduce bag � Dissect � FDA approved tissue extraction � Accordion � Apply traction bag by Applied Medical � Parallel to the ureter � Ties at two ends � introduce � Cook Lap Sac bag � Medial to uterosacral bag � cut strings to “deploy � Create planes and windows ligament � Isolation bag � Open bag � Fat stays with the bowel or � Do not tear � Fluid in the bag bladder � Reverse trendelenburg � Cold scissors close to viscera � Backfill bladder 7
10/26/2016 Assess for injury Conclusions � Backfill the bladder � Use the right incision for the right surgery � Rectal integrity test � Know your anatomy � Cystoscopy � Right placement of trocars is essential � fluorescein � Blood is the enemy � indigo carmine � methylene blue � Identify complications early � preop pyridium Resources Thank you! � AAGL SurgeryU � https://www.aagl.org/service/surgeryu/ � International Academy of Pelvic Surgery � https://www.academyofpelvicsurgery.com/ � Websurg � http://www.ircad.fr/e-learning/websurg/ 8
Recommend
More recommend