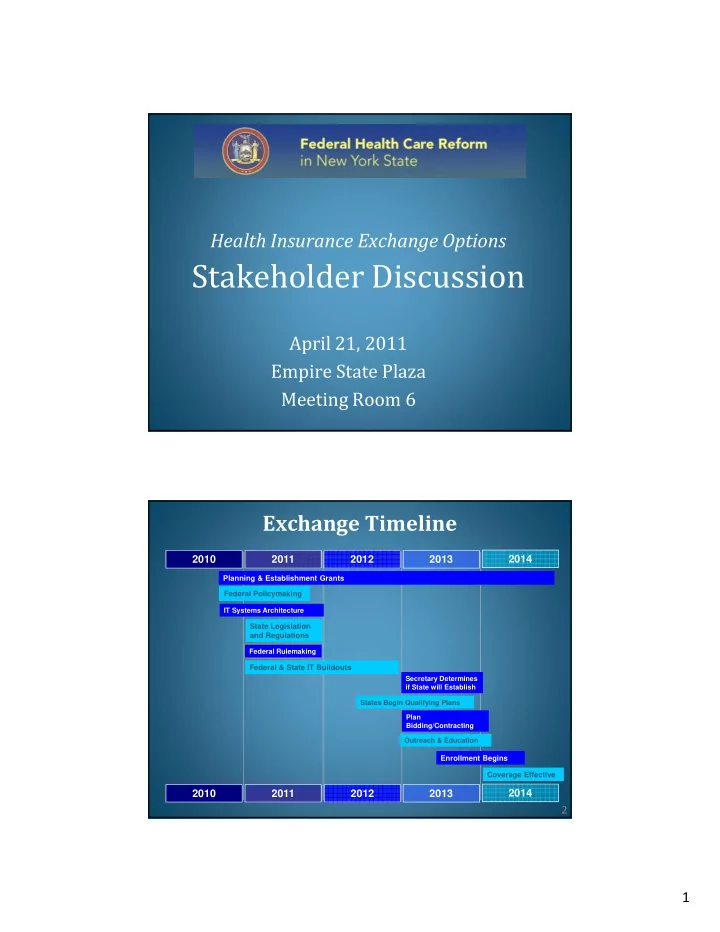
Health Insurance Exchange Options Stakeholder Discussion April 21, 2011 Empire State Plaza Meeting Room 6 Exchange Timeline 2010 2011 2012 2013 2014 Planning & Establishment Grants Federal Policymaking IT Systems Architecture State Legislation and Regulations Federal Rulemaking Federal & State IT Buildouts Secretary Determines if State will Establish States Begin Qualifying Plans Plan Bidding/Contracting Outreach & Education Enrollment Begins Coverage Effective 2010 2011 2012 2013 2014 2 1
New York’s Health Insurance Exchange I. Principles II. Functions III. Exchange Design Questions 3 Principle : It must promote affordable, comprehensive health insurance options • Access to federal subsidies • Plans compete based on price and quality, not risk selection • Opportunity to pool purchasing power 4 2
Principle : It must be consumer-oriented • First class consumer experience • Easy to navigate • Assistance for questions and problems • No wrong door • Attracts small businesses 5 Principle : It must be transparent and accountable • Information publicly accessible • Opportunity for stakeholder input • Subject to reporting, audits and review • Ethics considerations (e.g., conflicts, gifts, post-employment) 6 3
Principle : It must work • Short timeframe: operating by 2014 • Needs to be flexible 7 Exchange Will Operate Within a Larger Environment IRS Public Programs: Commercial Exchange Medicaid Insurance Child Health Plus Market Family Health Plus HHS/CMS NYSDOH NYSID 8 4
Exchange Functions Some are the same or similar to those currently conducted by State regulatory agencies: Function of the Exchange DOH SID Certification, recertification, and decertification of plans √ √ Assignment of price and quality rating to plans √ √ Operate toll free hotline √ √ Maintenance of website for providing plan information √ √ Presentation of enrollee satisfaction survey results √ --- Eligibility determination and enrollment into a wide range √ --- of coverage options Provision for open enrollment period --- √ Consultation with stakeholders √ √ 9 Exchange Functions (cont) Some are new and are not currently conducted by State regulatory agencies: Function of the Exchange DOH SID “Customer-centric” systems approach, including --- --- presentation of plan benefits in a simple, standardized, comparative format Provision of an electronic calculator --- --- Certification of individuals exempt from individual --- --- responsibility Provision of information to the U.S. Treasury Department --- --- Navigator to assist consumers in shopping and enrollment --- --- Publication of data on Exchange’s administrative costs --- --- 10 5
Governance Where should the Exchange Principles: be placed? � Affordable � High Quality • State Agency � Consumer- • Public Authority Oriented � Transparent/ • Not-for-Profit Accountable � It Must Work 11 Exchange Legislation Washington Maine Montana North Dakota Minnesota Oregon New Hampshire Wisconsin Vermont Idaho South Dakota New York Massachusetts Michigan Wyoming Rhode Island Pennsylvania Iowa Connecticut Nebraska Nevada Ohio New Jersey Utah Illinois Indiana West Virginia Delaware Colorado Kansas Missouri Maryland California Virginia Kentucky DC North Carolina Tennessee Oklahoma Arizona Arkansas New Mexico South Carolina Alabama Georgia Mississippi Texas Louisiana Florida ����������������� Quasi-governmental entity ������������������� Two options: existing agency or non-profit Formal draft prepared Within existing agency or office Introduced (Statuses shown are Non-profit accurate as of New state agency Passed and signed into law 4/19/2011) Not specified Passed and not signed into law 12 6
Structure 1. Should there be one statewide Principles: Exchange or multiple � Affordable subsidiary Exchanges? � High Quality � Consumer- 2. Should there be one combined Oriented Exchange for individuals and � Transparent/ small businesses (SHOP) or Accountable separate Exchanges for each � It Must Work group? 13 Purchasing Role Which plan participation model should be used? Principles: � Affordable � High Quality Clearinghouse Model � Consumer- Oriented Selective Contractor � Transparent/ Accountable Active � It Must Work Purchaser 14 7
Benefits Design How to balance plan innovation Principles: with ensuring ease of comparison shopping? � Affordable � High Quality – Platinum: benefits actuarially equivalent to 90% of full actuarial value � Consumer- Oriented – Gold: benefits actuarially equivalent to 80% of full actuarial value � Transparent/ Accountable – Silver: benefits actuarially equivalent to 70% of full actuarial value � It Must Work – Bronze : benefits actuarially equivalent to 60% of full actuarial value 15 Adverse Selection Principles: 1. Should the rules inside and outside the Exchange be the � Affordable same? � High Quality � Consumer- 2. Should insurers outside the Oriented Exchange be required to offer all benefit options (e.g., � Transparent/ Accountable California)? � It Must Work 16 8
Organization of Market Should New York: Principles: 1. Merge individual and small � Affordable group markets? � High Quality � Consumer- 2. Expand small group size Oriented (50 to 100)? � Transparent/ Accountable 3. Include large groups in the � It Must Work Exchange? 17 Additional Information www.HealthCareReform.ny.gov Questions regarding implementation can be sent to: HealthCareReform@exec.ny.gov. 18 9
Recommend
More recommend