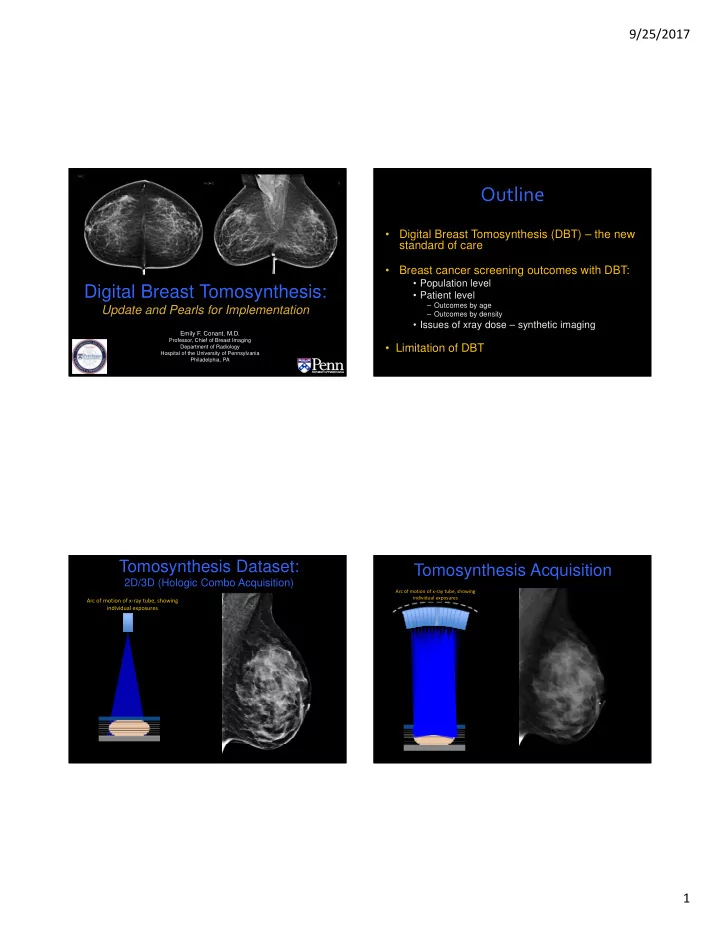
9/25/2017 Outline • Digital Breast Tomosynthesis (DBT) – the new standard of care • Breast cancer screening outcomes with DBT: • Population level Digital Breast Tomosynthesis: • Patient level – Outcomes by age Update and Pearls for Implementation – Outcomes by density • Issues of xray dose – synthetic imaging Emily F. Conant, M.D. Professor, Chief of Breast Imaging • Limitation of DBT Department of Radiology Hospital of the University of Pennsylvania Philadelphia, PA Tomosynthesis Dataset: Tomosynthesis Acquisition 2D/3D (Hologic Combo Acquisition) Arc of motion of x ‐ ray tube, showing individual exposures Arc of motion of x ‐ ray tube, showing individual exposures 1
9/25/2017 Tomosynthesis Dataset: “3D” Dataset 2D/3D (Hologic Combo Acquisition) Projections reconstructed into 1 mm thick slices Projection Images Reconstructed P rojection Images 2D “Dose” Reconstructed Reconstructed 15 images/15 0 arc Mammogram Tomo Slices “Synthetic 2D” 15 images/15 0 arc Tomosynthesis Slices Digital Breast Tomosynthesis DBT Screening Outcomes The new, better mammogram: – Recall reduction (-15-37%) – Increased invasive cancer detection (up to 50%) – No increase in situ detection (? overdiagnosis) 2
9/25/2017 Summary of DBT Screening Studies Summary of DBT Screening Studies Author (Year) Volumes DM versus DBT Author (Year) Volumes DM versus DBT Industry Industry Recall Rate (%) Cancer Rate (per/1000) Recall Rate (%) Cancer Rate (per/1000) Skaane (2013) 12,631 multi reads 6.1 to 5.3% 6.1 to 8.0 Skaane (2013) 12,631 multi reads 6.1 to 5.3% 6.1 to 8.0 Prospective 15% reduction 27% increase Prospective 15% reduction 27% increase Hologic Hologic (p<0.001) (p<0.001) Ciatto (2013) 4.5 to 3.5% 5.3 to 8.1/1000 Ciatto (2013) 4.5 to 3.5% 5.3 to 8.1/1000 7,292 DM then DBT 17.2% “conditional” reduction (cancers overall not by pt) 7,292 DM then DBT 17.2% “conditional” reduction (cancers overall not by pt) Hologic Hologic 52.8% increase 52.8% increase 7,500 2.6 to 3.8% 6.3 to 8.9% 7,500 2.6 to 3.8% 6.3 to 8.9% Lang (2015) Lang (2015) The improvement in outcomes 46% increase (to 3.8%) 43% increase 46% increase (to 3.8%) 43% increase Siemens – single view only Siemens – single view only achieved with DBT directly address the 454,850 10.7 to 9.1 4.2 to 5.4 454,850 10.7 to 9.1 4.2 to 5.4 Friedewald (2014) Friedewald (2014) (DM: 281,187 15% reduction 24% increase (DM: 281,187 major concerns regarding screening for 15% reduction 24% increase Increase in Hologic Hologic DBT: 173,663) (p<0.001) (p<0.001) DBT: 173,663) (p<0.001) (p<0.001) Decrease in Recall of Cancer Detection up breast cancer with mammography: Greenberg (2014) 59,617 16.2 to 13.6% 4.9 to 6.6 Greenberg (2014) 59,617 16.2 to 13.6% 4.9 to 6.6 Retrospective Retrospective up to 31% to 53% (DM: 38,674 16% reduction 35% increase (DM: 38,674 16% reduction 35% increase Hologic Hologic DBT: 20,943) (p<0.0001) (p=0.035) DBT: 20,943) (p<0.0001) (p=0.035) • Too many false positives (low specificity) McCarthy (2014) 26,299 10.4 to 8.8% 4.6 to 5.5 McCarthy (2014) 26,299 • Too few cancers detected (low sensitivity) 10.4 to 8.8% 4.6 to 5.5 (DM: 10,728 15% reduction 19.6% increase (DM: 10,728 15% reduction 19.6% increase Hologic Hologic • Over ‐ diagnosis (esp. DCIS) DBT: 15,571) (p<0.001) (p=0.32) DBT: 15,571) (p<0.001) (p=0.32) Lourenco (2015) 25,299 9.3 to 6.4% 5.4 to 4.6 Lourenco (2015) 25,299 9.3 to 6.4% 5.4 to 4.6 (DM: 12,577 31% reduction 15% decrease (DM: 12,577 31% reduction 15% decrease Hologic Hologic DBT: 12,921) (p<0.00001) (P =0.44) DBT: 12,921) (p<0.00001) (P =0.44) Conant (2016) 198,881 10.4 to 8.7 % 4.4 to 5.9 Conant (2016) 198,881 10.4 to 8.7 % 4.4 to 5.9 (DM: 142,883 16.3% reduction 34% increase (DM: 142,883 16.3% reduction 34% increase Hologic Hologic DBT:55,998) (p <.0001) (p=0.0026) DBT:55,998) (p <.0001) (p=0.0026) Sub ‐ populations reported in Friedewald, et al . Sub ‐ populations reported in Friedewald, et al . DBT reduces false positive call ‐ backs: 47yr ‐ old presents for screening, focal asymmetry, left lateral on CC Recall Reduction Tomosynthesis imaging shows no abnormality. (Tissue superimposition present on 2D) 3
9/25/2017 DBT reduces false positive call ‐ backs: On sequential DBT slices, each component of “lesion” 43yr ‐ old presents for baseline screening. Architectural distortion? is a separate structure (note localizer positions). No recall needed! 46 year old woman presents for screening… Improved Cancer Detection A case 4
9/25/2017 2D DBT US 6 cm Invasive Lobular Carcinoma Teaching point: it’s not all about density… MRI Findings: Architectural distortion, irregular mass in UOQ, Cancer detected on DBT alone: best on DBT. Work up was directly to US. 68 ‐ year ‐ old woman presenting for screening The 2D mammogram was interpreted as negative Pathology: Invasive lobular carcinoma 5
9/25/2017 Limitations of early trials • Most studies “first, prevalent” round screening • Only 3 studies were prospective (Oslo, STORM, Malmo) University of Pennsylvania Data • Majority of retrospective studies had concurrent Method: DM screening • Three consecutive years DBT screening – Population level analysis (each year of screening) – potential for bias in screened cohorts – Patient level analysis (each round of screening) – Comparison with cancer registry data for false negatives • There has been little data on false negatives…. McDonald EM et al. JAMA Oncol. 2016;2(6): 1 ‐ 7 Results from Penn consecutive years Population ‐ level Cancer and Biopsy rates, PPV1 by year of DBT screening 8 7 6.7 6.5 6.2 6.1 Metric Year 0 DM Year 1 DBT Year 2 DBT Year 3 DBT 6 5.8 5.5 Recall rate (%) 10.4 8.8 9.0 9.2 5 Cancer/1000 4.6 4.4 Invasive cancer/1000 Cancer rate/1000 4.6 5.5 5.8 6.1 4.1 4.1 4 3.8 Interval cancer/1000 PPV1 4.4 6.2 6.5 6.7 Biopsy % 3.2 3 PPV1 Interval CA/1000 0.7 0.5 ‐ 2 2 1.9 1.9 1.8 1 0.7 0.5 0 yr 0 (DM) DBT yr 1 DBT yr 2 DBT yr 3 McDonald EM et al. JAMA Oncol. 2016;2(6): 1 ‐ 7 McDonald EM et al. JAMA Oncol. 2016;2(6): 1 ‐ 7 6
9/25/2017 Breast Cancer Research and Treatment – on ‐ line 3/1/16 What about first round, “Prevalence Effect”? Patient ‐ level Outcomes for Consecutive Years of Screening 14 12.4 12 10 9.1 8.6 8 PROSPR consortium (BWH-D, UVt, UPenn) 7.4 7.3 Recall rate % 6.9 Cancer/1000 6.3 • DM and DBT cases 2011-15 (142,883 DM and 55,998 DBT studies) 6.1 6 5.9 PPV1 % 5.1 4.6 – Patient level data 4.2 4 • Reduction in recall (8.7% vs 10.4% p<0.0001) 2 • Increase in cancer detection (5.9 vs 4.4/1000, p= 0.0026), – 34% increase in cancers overall 0 – 27% invasive cancers DM with priors One DBT Screen with Two DBT Screens (n= Three DBT Screens priors (n= 21395) 9316) (n=3023) • Trend in decrease in false negatives (0.46 vs 0.6/1000) McDonald EM et al. JAMA Oncol. 2016;2(6): 1 ‐ 7 Conant EF et al. BCR&T 2016; on ‐ line 3/1/16 Cancer Detection (per 1000) by Age Tomosynthesis Outcomes by Density Category 9 8.2 8 Change in Cancer Change in Recall Author Year Mean Age Number of Dense 7.4 Detection Rate Rate 7 7 Patients (per 1000) (per 1000) Cancer Detection per 1000 6 Prospective Trials 5.7 Ciatto 2013 58 1,215 +2.5 ‐ 26 5 5 5.02 BCSC 4.54 Lang 2016 56 3,150 +3.8 ‐ DM 4 3.8 3.77 DBT Bernardi 2016 58 2,592 +5.4 +10.5 3.6 3 2.9 Tagliafico 2016 51 3,231 +4 ‐ 2.53 2 Retrospective Trials Rose 2013 54 4,006 +1.4 ‐ 36.8 1 McCarthy 2014 55 5,056 +1.8 ‐ 19.4 0 Conant 2016 57 9,265 (21,133) +2.1 ‐ 22.1 40 ‐ 49 50 ‐ 59 60 ‐ 69 >70 Rafferty 2016 ‐ 84,243 +1.4 ‐ 18.4 Adapted from Houssami N, Turner RM. Breast 2016: 141 ‐ 145. Derived from unpublished data: Friedewald, et al. JAMA 2014;311(24):2499 ‐ 2507 7
9/25/2017 Cancer Detection (per 1000) by Density Category 7 6 6.1 5.3 Cancer Detection per 1000 5 What about False Negatives? 4.5 4.4 4.27 4.2 4 3.9 3.88 3.8 BCSC 3.37 DM 3.2 3 DBT 2.52 2 1 0 Fat Scattered Hetero Extreme Derived from unpublished data: Friedewald, et al. JAMA 2014;311(24):2499 ‐ 2507 54 yo with pain, thickening of the right breast False negative DBT: Not all cancers visible with DBT . 42 yo with lump in left breast. 2012 2013 MIP Left (Normal) DBT MLO Views MIP Right Invasive Ductal CA (TNeg) Diagnostic mammogram (2013), ultrasound for rt pain, thickening “negative”. DM DBT MRI extensive asymmetric NMLE enhancement rt breast. Invasive ductal carcinoma. 8
9/25/2017 Comparison of DBT Dose • Hologic DBT has dose boost at > 50mm • Siemens DBT dose higher than DM for all thicknesses • GE DBT dose same as DM (uses grid for both modes) What about Dose?? Hologic Siemens GE Courtesy of Andrew Maidment, PhD Overview of s2D Reconstruction Tomo Stack Synthetic 2D Imaging DBT image data used to create both 1mm slices for s2D Mammo tomo “stack” and s2D images Multiple, low dose images obtained and then reconstruction 9
Recommend
More recommend