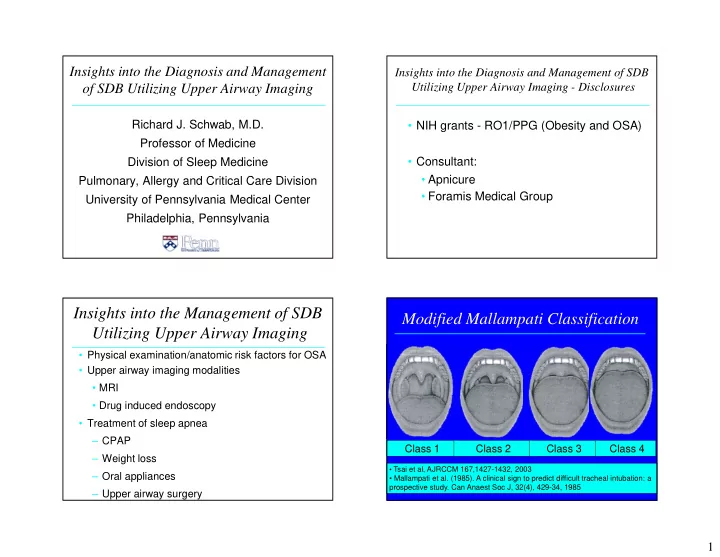
Insights into the Diagnosis and Management Insights into the Diagnosis and Management of SDB Utilizing Upper Airway Imaging - Disclosures of SDB Utilizing Upper Airway Imaging Richard J. Schwab, M.D. • NIH grants - RO1/PPG (Obesity and OSA) Professor of Medicine Division of Sleep Medicine • Consultant: • Apnicure Pulmonary, Allergy and Critical Care Division • Foramis Medical Group University of Pennsylvania Medical Center Philadelphia, Pennsylvania Insights into the Management of SDB Modified Mallampati Classification Utilizing Upper Airway Imaging • Physical examination/anatomic risk factors for OSA • Upper airway imaging modalities • MRI • Drug induced endoscopy • Treatment of sleep apnea – CPAP Class 1 Class 2 Class 3 Class 4 – Weight loss • Tsai et al, AJRCCM 167,1427-1432, 2003 – Oral appliances • Mallampati et al. (1985). A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaest Soc J, 32(4), 429-34, 1985 – Upper airway surgery 1
Modified Mallampati Classification Anatomic Risk Factors for Sleep Apnea • Obesity and its effects on the upper airway tissues • Increased neck circumference • Nasal airway restriction: septal deviation, allergic rhinitis, nasal polyps • Macroglossia/tongue ridging • Adeno-tonsillar hypertrophy (palatine/lingual tonsils) • Lateral peritonsillar narrowing • Enlargement/elongation of the soft palate • Recessed mandible (retrognathia)/maxilla • Narrowed hard palate - overbite/overjet What is this patient’s Modified Mallampati • A combination of soft tissue and/or craniofacial risk score? factors is likely most important Normal Upper Airway Morphometric Measurements (Schellenberg et al, AJRCCM 162;740-748, 2000) (Schellenberg AJRCCM 162;740-748, 2000) • Macroglossia: tongue being above level of mandibular occlusal plane • Uvula enlargement: > 1.5 cm in length or > 1.0 cm in width • Enlargement of lateral walls: > 25% impingement pharyngeal space by peritonsillar tissues • Tonsillar enlargement: > 50% lateral impingement of posterior pharyngeal airspace 2
Physical Examination and Sleep Apnea Physical Examination and Sleep Apnea (Schellenberg et al, AJRCCM 162;740-748, 2000) (Schellenberg et al, AJRCCM 162;740-748, 2000) Normal Upper Airway Physical Examination and Sleep Apnea (Schellenberg et al, AJRCCM 162;740-748, 2000) (Schellenberg et al, AJRCCM 162;740-748, 2000) 3
Lateral Pharyngeal Grading System Physical Examination and Sleep Apnea (Schellenberg et al, AJRCCM 162;740-748, 2000) • Class I = palatopharyngeal arch intersects at the edge of the tongue • Class II = palatopharyngeal arch intersects at 25% or more of the tongue diameter • Class III = palatopharyngeal arch intersects at 50% or more of the tongue diameter • Class IV = palatopharyngeal arch intersects at 75% or more of the tongue diameter Tsai, et al. A Decision Rule for Diagnostic Testing in Obstructive Sleep Apnea. American Journal of Respiratory and Critical Care Medicine, Vol. 167, No. 10 (2003), pp. 1427-1432 Physical Examination and Sleep Apnea Physical Examination and Sleep Apnea (Schellenberg et al, AJRCCM 162;740-748, 2000) (Schellenberg AJRCCM 162;740-748, 2000) Adjusted Odds Ratio (OR) for Sleep Apnea Physical Finding OR 95% CI • Lateral Narrowing 2.6* 1.7 - 4.1 • Tonsillar hypertrophy 2.1* 1.1 - 4.2 • Macroglossia 2.0 1.1 - 3.6 • Enlarged soft palate 1.9 1.2 - 2.9 • Retrognathia 1.3 0.8 - 2.1 *Maintained significance after adjusting for BMI/neck size 4
Quantify Anatomic Risk Factors for OSA Digital Morhphometrics with Laser Ruler with Digital Morhphometrics/Laser Ruler Upper Airway Soft Tissue and Different Imaging Modalities to Craniofacial Measurements Phenotype the Upper Airway • Morphometric examination/digital photography • Cephalometrics - craniofacial skeleton • Nasopharygnoscopy - awake and sleep induced (Propofol) • Acoustic Reflectance - airway • Optical Coherence Tomography - airway lumen • Computed Tomography • Magnetic Resonance Imaging 5
Müller Maneuver - Retropalatal Region Traditional Cephalometry (Ritter et al, Laryngoscope 109:954-963, 1999) Normal Examination of craniofacial skeleton - but a two Sitting - Baseline Sitting - Maximum Effort dimensional analysis of a three dimensional structure Studied 18 normal subjects with Müller maneuver during NPL; quantification of airway caliber; changes in airway dimensions Utility of CBCT in OSA Müller Maneuver - Retropalatal Region • The literature lacks strong evidence for using CBCT to assess (Ritter et al, Laryngoscope 109:954-963, 1999) treatment outcomes in the OSA population • However the available studies provide some evidence of Normal utilizing CBCT to measure anatomic airway changes with surgical and dental appliance treatment for OSA • Three studies using oral appliances and CBCT: – Haskell JA et al, (2009) Semin Orthod 15:132-58 – Abi-Ramia LBP, et al (2010) Dental Press J Orthod 15:166-71 Baseline (Quiet Respiration) – Singh GD, Wendling S, Chandrashekhar R (2011) Dent Today 30:124-7 • CBCT may emerge as an objective tool to anatomically and functionally assess OSA treatment outcomes • High-quality evidence studies, with statistically appropriate sample sizes and clinical cross validation are needed to determine the role of CBCT to assess treatment outcome in OSA patients - 10 cm H 2 O - 20 cm H 2 O - 30 cm H 2 O - 40 cm H 2 O Alsufyani NA et al (2013) Sleep Breath. “CBCT assessment of upper Consider NPL sleep induced endoscopy with propofol airway changes and treatment outcomes of OSA: a systematic review” 6
M Raffaini, C Pisani (2012) J Cranio-Maxillo-Facial Surg M Raffaini, C Pisani (2012) J Cranio-Maxillo-Facial Surg Drug Induced Sleep Endoscopy Borek et al (2012) Laryngoscope; 122:2592-9 Borek et al (2012) Laryngoscope; 122:2592-9 7
Normal Subject (Axial View) Normal Subject (Mid-Sagittal View) (Schwab, Am J Resp Crit Care Med 152:1673-1689, 1995) (Schwab, Am J Resp Crit Care Med 152:1673-1689, 1995) Airway Tongue Pharyngeal Wall Soft Mandible Mandible Palate Parapharyngeal Parotid Tongue Retropalatal Fat Pad Pharyngeal Wall Retroglossal Airway Subcutaneous Subcutaneous Fat Fat Mandible Spinal Cord Subcutaneous Fat MR Cephalometry Novel MR Cephalometry: Mandible Landmarks: S: sella N: nasion A: subspinale B: supramentale Gn: gnathion H: hyoid Angles: SNA (maxilla) SNB (mandible) NSH (hyoid) Linear distances computed mathematically from Cartesian Mid-Sagittal MRI coordinates (z-axis determined by slice number and thickness) 8
Craniofacial Changes in Normals and Apneics Craniofacial Changes in Normals and Apneics (Chi et al, European Respiratory Journal 38: 348-58, 2011) (Chi et al, European Respiratory Journal 38: 348-58, 2011) • We found that a 1-SD increase in mandibular length and depth were associated with decreased risk of sleep apnea in men but not in the women • The hyoid was more inferior and posteriorly positioned in apneics • The difference between apneics and controls for hyoid position was lost after controlling for tongue volume. Thus, increased tongue size mediates the inferior position of the hyoid Sagittal Upper Airway MR Images Axial Upper Airway MR Images (Schwab, Am J Resp Crit Care Med 152:1673-1689, 1995) (Schwab, Am J Resp Crit Care Med 152:1673-1689, 1995) Normal Subject Apneic Patient Normal Subject Apneic Patient 9
Schwab et al, AJRCCM 168; 522-530, 2003 Volumetric Anatomic Risk Factors for Sleep Apnea (Cases/Controls: N = 96) Tongue Mandible Parapharyngeal Airway Fat Pads Adjusted § Odds Ratio (OR) for Sleep Apnea: (Schwab et al, AJRCCM 168; 522-530, 2003) Soft Tissue Volume OR 95% CI Pharyngeal • Fat pads 1.64 1.00 - 2.81 Soft Palate Normal Subject Walls • Lateral Walls 6.01* 2.62 - 17.14 Mandible Parapharyngeal Airway Tongue • Soft Palate 1.66 0.99 - 3.18 Fat Pads • Tongue 6.55* 2.81 - 19.42 • Total Soft Tissue 6.95* 3.08 - 19.11 § Adjusted for gender, ethnicity, age, craniofacial size and Pharyngeal Soft Palate Patient with Sleep Apnea visceral neck fat * = Significant Walls Does Exercising the Upper Airway Why are Upper Airway Soft Tissue Muscles Improve Sleep Apnea? Structures Enlarged in Apneics? • Playing the didgeridoo improves sleep apnea • Edema from negative pressure – Puhan et al, BMJ 332; 266 - 270, 2006 • Changes in blood flow • Muscle disorder/function/exercise • Vibration/snoring/surface tension • Performing oropharyngeal exercises improves sleep • Weight gain/obesity apnea – Guimaraes et al, AJRCCM 179; 962 - 966, 2009 • Gender – What does exercise do to the upper airway - tongue • Genetic factors fat? 10
Recommend
More recommend