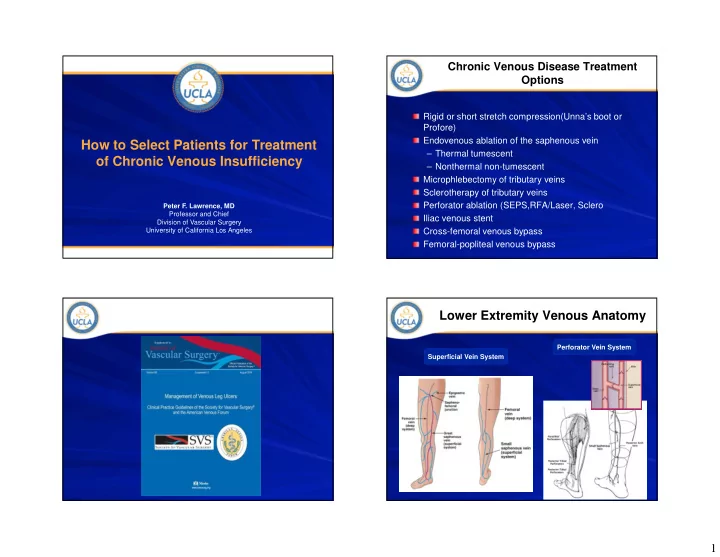
Chronic Venous Disease Treatment Options Rigid or short stretch compression(Unna’s boot or Profore) Endovenous ablation of the saphenous vein How to Select Patients for Treatment – Thermal tumescent of Chronic Venous Insufficiency – Nonthermal non-tumescent Microphlebectomy of tributary veins Sclerotherapy of tributary veins Perforator ablation (SEPS,RFA/Laser, Sclero Peter F. Lawrence, MD Professor and Chief Iliac venous stent Division of Vascular Surgery University of California Los Angeles Cross-femoral venous bypass Femoral-popliteal venous bypass Lower Extremity Venous Anatomy Perforator Vein System Superficial Vein System 1
Proximal Iliac Vein Pathophysiology of CVI Stenosis/Obstruction Vein valves – Bicuspid valves – Blood propelled by calf muscle pump opens the valve in one direction – Blood moving with gravity closes the normal valve – Incompetence of valve at saphenofemoral junction is the source of most varicose veins Chronic Venous Insufficiency Proximal Iliac Vein Stenosis/Obstruction Classification Prospective study of 78 CEAP 5/6 patients to assess incidence of proximal venous disease – Imaging modality: Duplex ultrasound plus combined with either CTV or MRV – M:F = 50%; mean age =60 Clinical Anatomic – Ulcers equally distributed between R and L – (1) Telangiectasias – Deep – 50% had hx of DVT – Superficial – (2) Varicose veins – Perforator 37% had iliocaval stenosis of – (3) Edema >50%; 23% had Pathophysiologic – (4) Skin changes stenosis/occlusion>80% – Reflux – (5) Ulcer-healed Independent risk factors= – Obstruction – (6) Ulcer-active – Women – Reflux + obstruction Etiologic – Hx of DVT – Deep venous reflux – Primary – Secondary – Congenital JVS 2004;40(6):1248-1252 JVS 2011;53:1303-1308 2
Assessing Venous System Classification System Non-invasive vascular lab CEAP is the best classification system The most common chronic disease in the US Duplex scan in reversed Trendelenberg – 40% of Americans have venous disease position to assess for: – 15-25% of the adult population have saphenous or branch incompetence – 40% of adults have telangiectasias (spider veins) – Great/Small saphenous incompetence One of the most common causes of wounds Large vein > 3.5 mm – 6% have a venous ulcer during their lifetime > 0.5 sec reflux – Perforator vein incompetence Large vein > 3.5 mm >0.5 sec reflux Pulsatility – Tributary incompetence – Presence of deep vein obstruction/incompetence Ann Epidemiol 2005;15(3):175-184 Circulation 2005;111:2398-2409 JVS 2014;60:Supplement S Support hose, Circaid, Short Stretch Heat Inducing Devices Compression Bandage and Unna’s Boot That Require Tumescence Superficial Veins Perforator Veins Laser and Radiofrequency RFA approved; Sclero and laser also used 3
Radiofrequency and Laser Ablation Perforator Ablation Mechanism of Action (Difficult!) 2-3 cm RFS catheter placed at a 45 degree angle- transverse and longitudinal transducer Confirm stylet in vein at fascia Inject local anesthetic to eliminate pain Trendelenberg position Vein treated with radiofrequency energy for 1 minute in each quadrant; repeated above the fascia if possible Confirmation of ablation post procedure difficult due to compression from local anesthetic Stab Phlebectomy Single Surgeon Learning Curve Procedure Perforator Closure Success Rate Incisions (Nokor Needle) 80% – Adjacent to the vein to avoid cutting it 70% – Length no greater than the crochet 60% 50% hook width (1 mm) 40% success rate – Penetrate dermis only 30% 20% Loop of vein pulled through incision 10% 0% Mosquitoes used to divide vein 2007 2008 2009 2010 Circular motion used to remove the Learning curve of a Single Vascular Surgeon vein- limits the size of the incision 80% 70% More incisions better than larger 60% incisions 50% success Vein path compressed with finger to 40% rate 30% reduce hematoma 20% 10% 0% Transillumination can be used for 2007 2008 2009 2010 complete vein removal JVS 2010;54(3):737-742 4
CEAP 1 Patients CEAP 2 Patients Telangiectasias or reticular veins Varicose veins Goals for Treatment – Elimination of reflux and any incompetence vein(s) – Reduce pain Elective – Cosmetic – Limited anesthesia – Short recovery – Excellent cosmetic result Treated with injection – Low complication rate (sclerotherapy) or laser – Low recurrence rate SVS-AVF guidelines: compression of 20-30 mmHg recommended, knee or thigh high (Grade 1, Level B) JVS 2014;60:Supplement S JVS 2014;60:Supplement S CEAP 2 Patients CEAP 2 Patients Varicose veins – Treatment Options Varicose veins Sclerotherapy Microphlebectomy 3-month technical success Nonthermal,nontumescent Mechanico-chemical – 96% EVLT Rotational wire/Sclero/Glue – 97% RFA – 95% NT,NT Postop pain was considerably lower for RFA Changes in quality of life between pre and post-operative were not significantly different Endovenous laser ablation of GSV/SSV Radiofrequency ablation of GSV/SSV Ann Surg. 2011;254(6)876:881 5
CEAP 3 Patients Impact of Superficial Vein Ablation for CEAP 2-4 Patients Edema Patients with edema, pain, and/or varicose veins Compression therapy* Presenting Number of patients Symptoms Lifestyle limiting pain n=696 (94.8%) Resolution of No resolution of symptoms symptoms Limb swelling n=485 (66%) Duplex ultrasound of Lipodermatosclerosis n=39 (5.3%) superficial veins Bleeding varicose n=10 (1.4%) Treatment of incompetent veins superficial veins *For post-thrombotic patients the SVS-AVF recommends compression of 30-40, knee or thigh high (Grade 1, Level B) JVS 2014;60:Supplement S Impact of Superficial Vein Ablation for Mid-Advanced CVI CEAP 2-4 Patients CEAP 4-6 Patients Relief of Symptoms Clinical Severity Number of Limbs (Mean=9 months) When to Intervene Patient presents with a leg Symptomatic varicose veins 217 92% that is pigmented and fibrotic (C2) in the “gaiter zone” of the Swelling (C3) 346 91% ankle Patient presents with non- Hyperpigmentation and/or healing ulcer that persists in 230 81% Lipodermatosclerosis (C4) spite of optimal compression Patient presents with a healed ulcer at the location of an 98.6% closure success rate at 24-72 hr incompetent perforator vein Mean follow-up = 9 mo. Late GSV recanalization = 1.8% Late SSV recanalization = 0% 6
What To Do With Patients with Progressive SVS-AFV Practice Guidelines Non Healing Venous Ulcers? Operative/Endovascular - Algorithm Venous Ulcer Correct the ambulatory superficial venous hypertension by: Diagnostics – Great saphenous ablation- agreed – Small saphenous ablation-agreed - + reflux + obstruction - – Tributary eradication-agreed similar + perforator + superficial risk/benefit: + proximal Less risk – Perforator ablation - ???? Rx Endo (open) Rx Endo Linton procedure Too many wound infections *** Failed/ not option SEPS Difficult to get ankle perforators Failed/ not option Reevaluate Reevaluate Laser/RFA ablation + proximal + infrainguinal +/+ + Superficial/perforator Deep reflux +/- -/+ Sclerotherapy Bypass Bypass/ Valvular unilateral endophlebectomy Deep system valvuloplasty/bypass – not routinely used reconstruction Not option/ similar risk/benefit: Reevaluate or Moderate risk Bypass Highest risk *** clarification: bilateral +/+ ulcer treat both, no ulcer treat only superficial Compression for life– and 25% with ulcers have weekly wound care! Simplified Patient Algorithm CEAP 5 Patients CEAP 4- 6 Patients Healed venous ulcer Guiding Information – Did the patient have difficulty healing the ulcer with compression bandages? – Is the patient compliant in wearing appropriate support stockings? – Does the patient have any incompetent superficial or perforator veins? – Does the patients lifestyle increase their risk of recurrence? 7
Recommend
More recommend