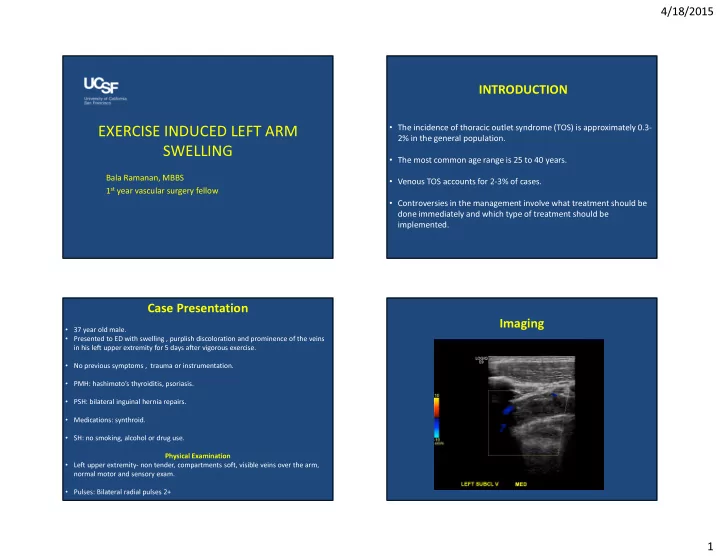
4/18/2015 INTRODUCTION • The incidence of thoracic outlet syndrome (TOS) is approximately 0.3- EXERCISE INDUCED LEFT ARM 2% in the general population. SWELLING • The most common age range is 25 to 40 years. Bala Ramanan, MBBS • Venous TOS accounts for 2-3% of cases. 1 st year vascular surgery fellow • Controversies in the management involve what treatment should be done immediately and which type of treatment should be implemented. Case Presentation Imaging • 37 year old male. • Presented to ED with swelling , purplish discoloration and prominence of the veins in his left upper extremity for 5 days after vigorous exercise. • No previous symptoms , trauma or instrumentation. • PMH: hashimoto’s thyroiditis, psoriasis. • PSH: bilateral inguinal hernia repairs. • Medications: synthroid. • SH: no smoking, alcohol or drug use. Physical Examination • Left upper extremity- non tender, compartments soft, visible veins over the arm, normal motor and sensory exam. • Pulses: Bilateral radial pulses 2+ 1
4/18/2015 What are the initial management options? Case Management A. Discharge home from ED on lovenox bridge to warfarin. • 87% Started on a heparin drip. B. Anticoagulation with heparin drip, • Underwent catheter directed thrombolysis and mechanical hypercoagulable workup and thrombectomy. discharge home on warfarin for 3-6 months. • Repeat Venogram on POD #1 showed patent subclavian vein with 10% stenosis. He underwent venoplasty of the subclavian vein using 6 C. Heparin drip, venogram and 3% 0% mm and 8 mm balloons with no significant change in the stenosis. catheter directed thrombolysis and . . . . . . . D e . . . c . E h m mechanical thrombectomy. e m h a b t r m o i g w r o o f n e n r e h m o t v i l o t , a a p h l i c D. Open surgical thrombectomy. u r i e g g d r g a r n u a o s r i h c n i a c t p e s n i e p D A O H PRETREATMENT VENOGRAM POST-THROMBOLYSIS VENOGRAM 2
4/18/2015 POST-VENOPLASTY VENOGRAM How would you further manage this patient? A. Discharge home on low molecular 57% weight heparin bridge to warfarin for 3-6 months. 39% B. Thoracic outlet decompression surgery in the same hospital stay. C. Discharge home on anticoagulation 4% followed by thoracic outlet decompression surgery at a later . . . . e . . . . . r c w p t i o m n l a o n c n o time. e o d e e m t m e o l t o h u h e o e g c r g a i r c a h a r h c o s c i h s D i T D What intervention would you perform to Case Management restore vein patency? 1. Ultrasound-guided retrograde left basilic vein access. 2. Left subclavian nonselective venogram. 70% 3. Left 1st rib resection. A. Intraoperative balloon venoplasty. B. Delayed balloon venoplasty +/- 4. Subclavian venolysis. stent. 5. Percutaneous balloon angioplasty of subclavian vein to 12 mm. C. Intraoperative venolysis/ vein 17% 13% patch. Postoperative course Discharged home on warfarin on POD 5 for 3 months then switched to aspirin. . . t . . s . . a / . v l s p i n s o y o n l o e o l v n a l e b n v o e o e v l v i l i t a t a a b r r e d e p e p o y o a a a r e l r t t n D n I I 3
4/18/2015 POST BALLOON VENOPLASTY IN OR STEP 1: IMMEDIATE THROMBOLYSIS • Immediate thrombolysis of venous TOS is favored as the syndrome can evolve very rapidly into a chronic stage with irreversible fibrotic changes of the vein. • This can lead to total obliteration with chronic edema and disability. Timing of TOS decompressive surgery STEP 2: PREVENTION OF RECURRENCE • Kunkel and Machleder* in 1989 described and algorithm of initial thrombolysis therapy followed by 3 months of anticoagulation to allow the inflammation to Role of venous stents alone without TOS decompressive surgery subside and then delayed transaxillary first rib resection and scalenectomy in 17 • Urschel et al.*studied 22 patients who had venous stents inserted without TOS patients. decompressive surgery. All 22 stents occluded within 6 weeks after insertion. The • Angie and colleagues# reviewed 18 consecutive patients and for the first time authors concluded that venous stents alone are contraindicated in venous TOS. compared outcomes of 9 patients undergoing immediate surgery and 9 patients undergoing staged therapy with excellent results in the early surgery group. • Meier and colleagues# studied outcome of venous stents after initial thrombolysis • Early decompressive surgery has now been widely adapted for treatment of venous for venous TOS. They observed stent fractures in patients who had venous stents TOS. alone. • In patients unable to receive early decompression- anticoagulation is followed by decompression at a convenient time. *J.M. Kunkel, H.I. Machleder. Arch Surg, 124 (1989), pp. *Urschel HC, Patel AN. Ann Thorac Surg 2003;75:1693-6. 13. 1153–1158 #Meier GH, et al.J Vasc Surg 1996;24:974-83. #Angie et al. Ann Vasc Surg, 15 (2001), pp. 37–42. 4
4/18/2015 Conclusions Direct interventions on the vein to re-establish normal caliber • Venous TOS occurs in young patients after vigorous • Schneider et al. *described balloon angioplasty alone during the exercise. surgery for TOS decompression in 25 patients. • Immediate thrombolysis is the first line of therapy. • Balloon angioplasty with stent implant as a delayed second • Venous stents alone are contraindicated. intervention has been reported by Hall et al.# and Kreienberg et al.! • Timing of TOS decompression surgery is • Direct surgical intervention- simple venotomy or patch enlargement controversial. of the vein during surgery for TOS decompression has been described • Vein stenosis can be treated with percutaneous by Molina and colleagues$ with 100% success rate in a cohort of 97 patients. angioplasty, venolysis or patch venoplasty. *Schneider DB, et al. J Vasc Surg 2004;40:599-603. #Hall LD,et al. J Vasc Interven Radiol 1995;6:565-70. 16. !Kreienberg PB, et al. J Vasc Surg 2001;33:S100-5. $ Molina et al. J Vasc Surg 2007; 45(2):328-34. 5
Recommend
More recommend