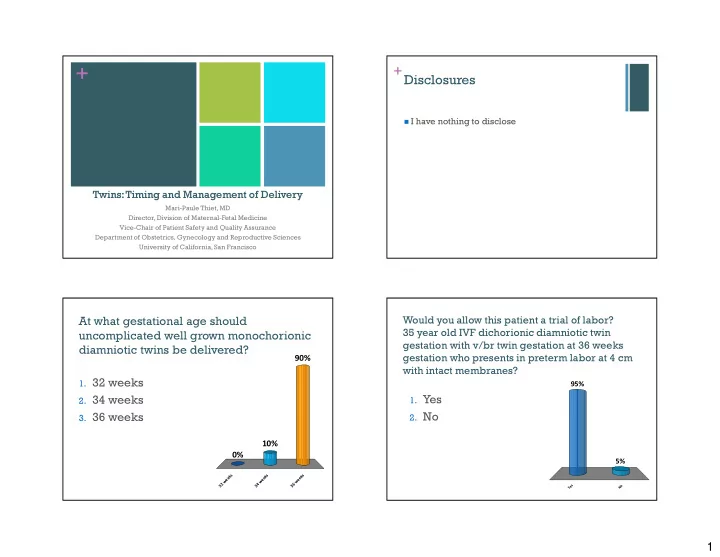
+ + Disclosures � I have nothing to disclose Twins: Timing and Management of Delivery Mari-Paule Thiet, MD Director, Division of Maternal-Fetal Medicine Vice-Chair of Patient Safety and Quality Assurance Department of Obstetrics, Gynecology and Reproductive Sciences University of California, San Francisco Would you allow this patient a trial of labor? At what gestational age should 35 year old IVF dichorionic diamniotic twin uncomplicated well grown monochorionic gestation with v/br twin gestation at 36 weeks diamniotic twins be delivered? 90% gestation who presents in preterm labor at 4 cm with intact membranes? 1. 32 weeks 95% 2. 34 weeks 1. Yes 3. 36 weeks 2. No 10% 0% 5% s s s k k k e e e e e e w w w 2 4 6 3 3 3 s o e Y N 1
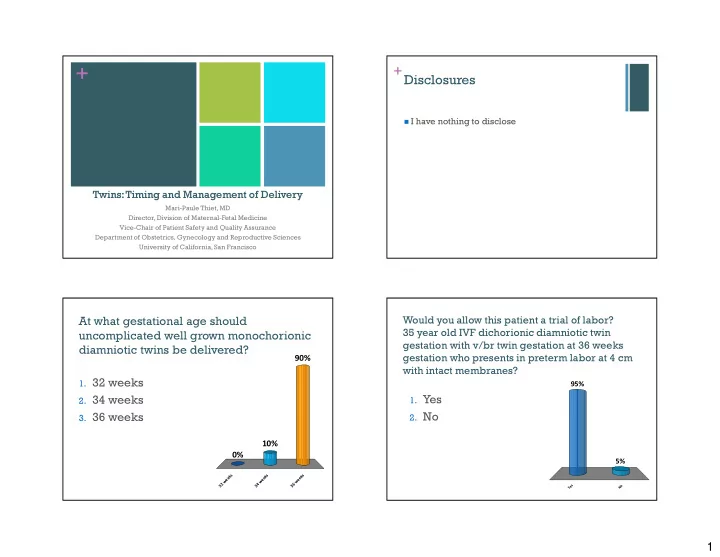
Would you allow her to labor if her first What if the previous patient had a twin has an estimated fetal weight of 5 hx of a previous low transverse c/s? lbs and the 2nd one has an EFW of 6# and is a footling breech? 74% 1. Yes, labor 54% 2. No, c/s 1. Yes 2. No 26% 46% r o s / b c a , l o N , s e s o Y e N Y + + Incidence/Scope of the problem Objectives � Define Incidence/scope of problem � Incidence of multiples increasing � ART vs spontaneous � Determine optimal gestational age for delivery � Older gravidas � Monochorionic vs dichorionic � Risks � Plan optimal route of delivery � Fetal/neonatal complications � Delivery considerations � Maternal complications � Management of 2 nd twin 2
+ Twins/Multiples + Assisted Reproduction � In 2002: 130,000 multiples born � Responsible for 17% of twins in US � Since 1980, � Risk of multiples increased 20-40% � 65% increase in twins � Clomiphene – 5-10% � 500% increase in triplets or > � IVF: # of embryos � risk of multiples � 3% of all births � 1 � 1.4% � 77% of preterm births � 2 � 17.9% � 4 � 24.1% � Disproportionate share of perinatal M&M � Higher than expected incidence of MC twins – 3.2% (background - 0.4%) ACOG Practice Bulletin, No 56, 2004, US Vital Stats, 2007 + Twins: Disproportionate Use of + Timing of Delivery Healthcare Dollars � Costs of twins associated with 2nd trimester � 25% spontaneous PTD, 25% Indicated PTD through 1 st month of life 5x compared to singleton (preeclampsia, IUGR) � $21K singleton � Sairam (2002): IUFD >39wks twins = 42 wks singleton � $104.8K twins � But mature at same rate � $407K triplets 3
+ Recommended timing of delivery: + Neonatal Mortality Near-term twins(≥34 weeks) � Twin Clinic at Med. Univ. S. Carolina � MFM, U/S, NST, del 37-38 wks � 1987-2010: 1779 twin gestations � 1011 excluded: PTD <34 wks, unsure chorionicity, monoamniotic, anomalies � 768 twin gestations analyzed � 601 di/di: 1 IUFD after 34 wks � 167 mo/di: no IUFDs after 34 wks (only 94 went past 36 wks) Burgess, American Journal of Obstetrics and Gynecology, 2014 Burgess, American Journal of Obstetrics and Gynecology, 2014 + Recommended timing of delivery: + Recommended timing of delivery: Complicated near-term twins Uncomplicated near-term twins (≥34 weeks) (≥34 weeks) Burgess, American Journal of Obstetrics and Gynecology, 2014 Burgess, American Journal of Obstetrics and Gynecology, 2014 Spong, NICHD consensus, 2011 4
+ + Twin Presentation Delivery Planning � Timing Vtx/Vtx 42.5% � Planned mode of delivery � L&D preparation Non-Vtx/Other Vtx/Non-Vtx 19.1% 38.4% Ramsey et al., Seminars in Perinatology 2003;27 (1) + Delivery: Twins + Mode of Delivery: Vtx/Vtx � Skilled/experienced � U/S in OR � Successful VD – 70-80% RNs, anesthesia, OB, � 8% operative vaginal delivery � Epidural anesthesia peds � 5% cesarean delivery recommended � 2% internal podalic version � Continuous EFM � Delivery in OR � No increase in M&M regardless of gestational age � Blood products � 27% anesth need or birth weight available � 6% emergent C/S Ramsey & Repke, Seminars on Perinatology, 2003 Carvalho, Int J Anesth 2008 5
+ + Mode of Delivery: Mode of Delivery: Non-Vertex Twin A Non-Vertex Second Twin � Cesarean Delivery generally recommended � Retrospective cohort, 1542 twin pairs in Nova Scotia, 1988-2002 � Level II-C evidence � 2 nd twin greater risk adverse outcome independent of presentation, chorionicity, sex Armson, B et al. Obstet Gynecol 2006 + + RCT: Mode of Delivery Mode of Delivery: Non-Vertex Second Twin First Twin Cephalic � Retrospective cohort, 858 twin pairs in France, � RCT: planned C/S vs planned VD >35 wks, 1 st twin cephalic, VD if B <125% A � Toronto/multi-center � “Active management of 2 nd twin” � Twins 32+0-38+6 wks � Twin A cephalic � Mean intertwin interval (VD) 4.9 minutes � Both alive, with EFWs 1500-4000g � 657 planned VD: 78% V/V , 21% C/C, 0.5% V/C � Excluded MA twins, lethal anomalies, previous classical or >1 LTCS � Neonatal composite morbidity unchanged � OBs “qualified” per their dept head � (5 vs 4.7%) � Level II evidence Barrett, Twin Birth Study Collab. Group NEJM 2013 Schmitz. Obstet Gynecol 2008 6
+ RCT: Mode of Delivery + RCT: Mode of Delivery First Twin Cephalic First Twin Cephalic � RCT: planned C/S vs planned VD � RCT: planned C/S n=1393 � If delivery elective: planned 37+5 to 38+6 wks � 90% delivered both by C/S � Continuous EFM � 0.8% Vag+C/S � Oxytocin, epidural per OB � 9% both Vag � Sono encouraged for delivery � Planned VD n=1393 � If Twin B cephalic, AROM delayed until head � 40% both C/S engaged � 4% Vag+C/S � If B not cephalic, OB chose breech delivery vs � 56% both Vag ECV vs C/S Barrett, Twin Birth Study Collab. Group Barrett, Twin Birth Study Collab. Group NEJM 2013 NEJM 2013 + RCT: Mode of Delivery + RCT: Mode of Delivery Outcomes Outcomes � Primary outcome (perinatal death or serious � Neonatal Morbidity 1.3% in both groups neonatal morbidity) � Birth trauma: n=4 vs n=7 (both <0.1%) � 2.2% planned C/S � 5 min Apgar <4: 0.1 vs 0.3% � 1.9% planned VD ( p 0.49) � Vent with ETT >24 hrs: n=27 (1%) vs n=17 (0.6%) � Perinatal death � 0.9% planned C/S � 0.6% planned VD Barrett, Twin Birth Study Collab. Group Barrett, Twin Birth Study Collab. Group NEJM 2013 NEJM 2013 7
+ RCT: Mode of Delivery + RCT: Mode of Delivery Outcomes � Maternal M&M: 7% vs 8.5% p 0.29 � Conclusion: � Maternal Mortality: n=1 in each group No benefits of planned cesarean section over planned vaginal delivery for twins between 32-38 � Maternal Morbidity: weeks if first twin is cephalic � Hemorrhage: 6% C/S vs 7.8% VD � 3 rd or 4 th degree: 0% C/S vs 0.3% VD � Infection (wound + non-wound): 3.7% C/S vs 2.6% VD Barrett, Twin Birth Study Collab. Group NEJM 2013 + Trial of Labor in Twins: + Trial of Labor in Twins: Previous Cesarean A few studies � Small studies � 38 TOL � 28 VD � no ruptures; 2 C/S for 2 nd twin � No increased risk uterine rupture, maternal � repeat C/S had higher SSI morbidity morbidity � 26 TOL � 85% del A vag, 73% del both vag; 71 � Perinatal mortality not increased after adjusting for elective RC/S confounders � No difference in outcomes except LOS � NIS data: 4705 elective repeat, 1805 TOL Aaronson, JMFNM 2009 � 45% both twins vag Delaney, JOG Can 2003 � 0.9% uterine rupture rate (= singleton rate) Sansregret, JOG Can 2003 Delaney, JOG Can 2003 Ford, AJOG 2006 Sansregret, JOG Can 2003 Barrett, 2013 Ford, AJOG 2006 8
+ Twins: A Reasonable Approach + Thank you for your attention. � Deliver at 36-37 wks mo/di, 38 wks di/di � Route of delivery based on presentation & OB experience (no benefit to C/S if you are trained to deliver twins) Questions? � Epidural anesthesia, OR delivery w/ U/S, peds, anesthesia, & extra MD/RN help 9
Recommend
More recommend