1/13/16 Pharmacist objectives: Summarize key updates to the DHHS treatment 1. guidelines. Identify recommended antiretroviral regimens for 2. Bernadette Jakeman, PharmD, PhC, BCPS, AAHIVP treatment-naive patients. Assistant Professor Describe common side effects and drug interactions 3. UNM College of Pharmacy associated with the recommended antiretroviral regimens. bjakeman@salud.unm.edu Technician objectives: Define HAART. 1. Define CD4 cell count and HIV viral load. 2. Explain why combination therapy is required in the 3. management of HIV. ¡ Approximately 1.2 million people are living ¡ www.aidsinfo.nih.gov with HIV in the US 1 ¡ Updated April 2015 ¡ 14% of infected patients remain undiagnosed 2 § Undiagnosed responsible for 30-50% of new cases 3,4 ¡ CDC recommends testing for all patients ages 13-64 years 5 1. CDC. MMWR June 26, 2015/64(24);657-662. 2. http://www.cdc.gov/hiv/pdf/surveillance_report_vol_19_no_3.pdf 3. Skarbinski J et al. JAMA Intern Med 2015;175:588–96. 4. Marks G et al. AIDS 2006;20:1447-50. 5. CDC MMWR Sept 22, 2006/55(RR14);1-17 A. <100 cells/mm 3 B. 100-200 cells/mm 3 C. 200-350 cells/mm 3 D. 350-500 cells/mm 3 E. >500 cells/mm 3 1
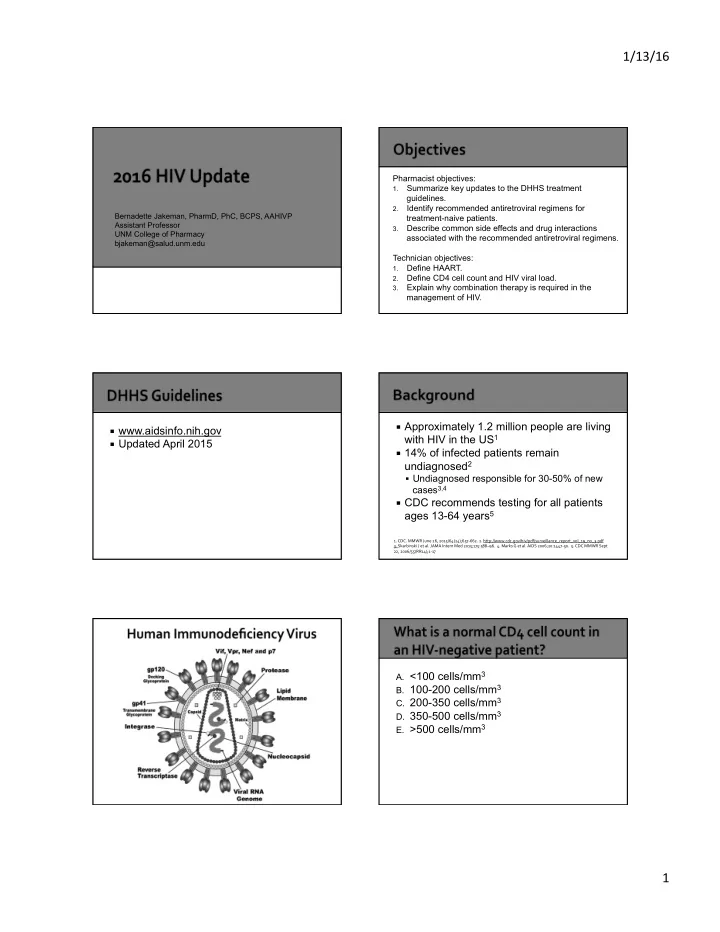
1/13/16 ¡ Reverse Transcriptase ¡ Integrase § Nucleoside/tide Reverse Transcriptase § Integrase Strand Transfer Inhibitors Inhibitors (NRTIs): Non-functional DNA (INSTIs): Bind viral integrase preventing building blocks which interrupts transcriptions integration of viral DNA into host genome ¡ Protease § Non-nucleoside Reverse Transcriptase § Protease Inhibitors (INSTIs): Bind viral Inhibitors (NNRTIs) : Binds reverse protease preventing conversion of viral transcriptase enzyme preventing transcription polypeptide into functional viral proteins ¡ NRTIs ¡ INSTIs A. One § Tenofovir § Dolutegravir B. Two § Emtricitabine § Raltegravir C. Three § Abacavir § Elvitegravir (with D. Four § Lamivudine cobicistat booster) § Zidovudine E. Five ¡ PIs (boosted with ¡ NNRTIs ritonavir or cobicistat) § Efavirenz § Darunavir § Rilpivirine § Atazanavir § Etravirine 2
1/13/16 ¡ HAART: Combination HIV therapy that suppresses HIV replication and prevents emergence of drug resistance when taken appropriately § Composed of 3 active medications from at least 2 classes § Commonly includes: ▪ 2 NRTIs (backbone) + another medication class (NNRTI, INSTI, PI) ¡ >95% adherence required for virologic suppression ¡ Early HAART improves outcomes 1-5 1. Kitahata MM et al. N Engl J Med. 2009;360(18):1815-26. 2. Lundgren JD et al 2015;373;795-807 . 3. Estrella M et al. CID 2006;43:337-380. 4. Bhaskaran K, et al. Ann Neurol. 2008;63:213-221. 5. Lichtenstein K, et al. CID 2010;51:435-447. Quinn TC et al. N Engl J Med 2000;342:921-929. ¡ Therapy recommended for ALL HIV- ¡ Proven clinical efficacy infected patients, regardless of pre- ¡ Ease of administration (frequency, pill treatment CD4 count burden) § CD4 count <350 cells/mm3 (AI) ¡ Low drug-drug interaction potential § CD4 cell count 350-500 cells/mm3 (AII) ¡ Low side effect profile § CD4 cell count >500 cells/mm3 (BIII) ¡ Baseline resistance testing recommended (GART) 1. Guidelines for the use of an- tiretroviral agents in HIV-1-infected adults and adolescents. DHHS. Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdoles- centGL.pdf. Accessed 1/6/2016. 2. INSIGHT START Study Group. N Engl J Med 2015;373:795-807. Dolutegravir + Abacavir/Lamivudine Superior to Efavirenz/Tenofovir/Emtricitabine ¡ INSTI-Based Regimens § Dolutegravir/abacavir/lamivudine § Dolutegravir + tenofovir/emtricitabine § Elvitegravir/cobicistat/tenofovir/emtricitabine § Raltegravir + tenofovir/emtricitabine § NEW!: Elvitegravir/cobicistat/tenofovir alafenamide /emtricitabine ¡ PI-Based Regimen § Darunavir + ritonavir + tenofovir/emtricitabine 1. Guidelines available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdoles- centGL.pdf. Accessed 1/6/2016. 2. HHS Panel on Antiretroviral Guidelines for Adults and Adolescents Update Nov 18, 2015. Walmsley S et al. J Acquir Immune Defic Syndr 2015;70:515-519. Walmsley SL et al. N Engl J Med 2013;369:1807-1818. https://aidsinfo.nih.gov/news/1621/evg-c-ftc-taf--statement-from-adult-arv-guideline-panel Accessed 1/6/2015. 3
1/13/16 Elvitegravir/Cobicistat/Tenofovir/Emtricitabine Noninferior to Efavirenz/Tenofovir/Emtricitabine ¡ One tablet once-a-day regimen for treatment- naïve patients ¡ No pre-treatment viral load restrictions Difference 3.6% (95% CI = -1.6 to 8.8) ¡ HLA-B*5701 screening required (abacavir) ¡ Possible increased cardiovascular risk (abacavir) ¡ Reduced tubular secretion of creatinine (dolutegravir, mean SCr increase = 0.15mg/dL)* ¡ Avoid coadministration with polyvalent cations ¡ Other ADEs: GI disturbances, headache, insomnia, transaminitis *Triumeq Package Insert. 2014. https://www.viivhealthcare.com/media/80846/Triumeq-PI-MG.pdf Sax PE et al. Lancet 2012;379:2439-2448. Accessed 1/6/2016. COBI Reduces tubular Secretion of Creatinine ¡ One tablet once-a-day regimen ¡ Cobicistat booster § CYP3A4 inhibitor = drug-drug interactions § Increases tenofovir concentrations, avoid use in patients with ClCr <70 mL/min ¡ Food increases absorption ¡ Avoid coadministration with polyvalent cations ¡ Other ADEs: diarrhea, nephrotoxicity, decreases in bone mineral density Sax PE et al. Lancet 2012;379:2439-2448. ¡ HMG-CoA reductase inhibitors (statins) ¡ Tenofovir disoproxil fumarate (TDF) ¡ Hep C protease inhibitors (boceprevir, § Readily converted in plasma to tenofovir diphosphate telaprevir) § Potential ADEs: ¡ Macrolides (clarithromycin, erythromycin) ▪ Proximal tubular uptake and dysfunction of kidney ¡ Corticosteroids ▪ Tenofovir-associated bone loss (alteration of gene ¡ Methadone expression) ¡ Tenofovir alafenamide (TAF) ¡ Rifampin § Stable in plasma, resulting in lower plasma ¡ Benzodiazepines tenofovir concentrations ¡ PDE5 inhibitors (e.g., tadalafil) § Converted intracellularly to tenofovir ¡ Oral contraceptives diphosphate § Advantages: may cause less nephrotoxicity and www.hiv-druginteractions.org bone effects, smaller pill size 4
1/13/16 Δ +2.0% § TAF group had smaller ¡ One tablet once-a-day regimen (95% CI: -0.7% to +4.7) 100 decline in eGFR (0 · 08 vs 92 90 § Approved by FDA November 2015 % Patients with HIV RNA <50 c/mm 3 0 · 12 mg/dL; p<0 · 0001) 90 § DHHS Recommend Agent November 2015 TAF group had less § ¡ Cobicistat booster 80 E/C/F/TAF (n=866) proteinuria (median % § CYP3A4 inhibitor = drug-drug interactions 70 change − 3 vs 20; E/C/F/TDF (n=867) § Avoid use in patients with ClCr <30 mL/ 60 p<0 · 0001) min 50 ¡ Food increases absorption § TAF group had smaller 40 reductions in bone mineral ¡ Avoid coadministration with polyvalent density at the spine (mean 30 cations % change − 1 · 30 vs –2 · 86; 20 p<0 · 0001) and hip ( − 0 · 66 6 ¡ Other ADEs: diarrhea, nephrotoxicity, 10 4 4 4 vs –2 · 95; p<0 · 0001) decreases in bone mineral density 0 Success Failure No Data E = elvitegravir; C = cobicistat, F = emtricitabine; TAF = tenofovir alafenamide; TDF = tenofovir disoproxil fumarate Sax PE, et al. Lancet 2015;385;2606-2615. INSTI Advantages Disadvantages Dolutegravir • Once-daily dosing • No coformulation with • Single tablet with abacavir/ tenofovir/emtricitabine § TAF/emtricitabine – under review lamivudine • High resistance barrier • Activity against resistant virus § Rilpivirine/TAF/emtricitabine – under • Few drug interactions review • No food requirement Elvitegravir • Once-daily dosing • Requires boosting • Single tablet • Drug-drug interactions § Darunavir/cobicistat/TAF/emtricitabine • Food requirement • Avoid if ClCr <70 ml/min if given § GS-9883/emtricitabine/TAF with TDF • New TAF formulation may require PA Raltegravir • First INSTI • BID dosing • Fewest drug interactions • No single-tablet regimen • Best ADE profile • Lower barrier to resistance • No food requirement Atazanavir/ Raltegravir Darunavir/ ritonavir ritonavir ¡ NNRTI-based regimen ADE Resulting in 95 (15.7%) 8 (1.3%) 32 (5.3%) § Efavirenz/tenofovir/emtricitabine Discontinuation ▪ Baseline resistance 1 GI toxicity 25 2 14 ▪ Failures due to ADEs requiring switch 2,3 ▪ CNS toxicity and suicidality 4 Hyperbilirubinemia 47 0 0 Other hepatic toxicity 4 1 5 ¡ PI-based regimen Rash 7 2 4 § Atazanavir + ritonavir + tenofovir/emtricitabine Metabolic toxicity 6 0 2 ▪ Failures due to ADEs requiring switch 5 Renal toxicity 4 0 0 ¡ Regimens with HIV RNA or CD4 cell count Abnormal chem/hem 0 0 2 restrictions Other 2 3 4 Results of study: Cumulative incidence of virologic and tolerability favored 1. Snedecor SJ et al. PLoS One 2013;8:e72784. 2. Walmsley SL et al. N Engl J Med 2013;369:1807-1818. 3. raltegravir and darunavir/ritonavir over atazanavir/ritonavir. Rockstroh JK et al J Acquir Immune Defic Syndr 2013;63:77-85 4. Mollan KR et al. Ann Intern Med 2014;161:1-10. 5. Lennox JL, et al. Ann Intern Med 2014;161:461-71. Lennox JL, et al. Ann Intern Med 2014;161:461-71 & supplemental material. 5
Recommend
More recommend