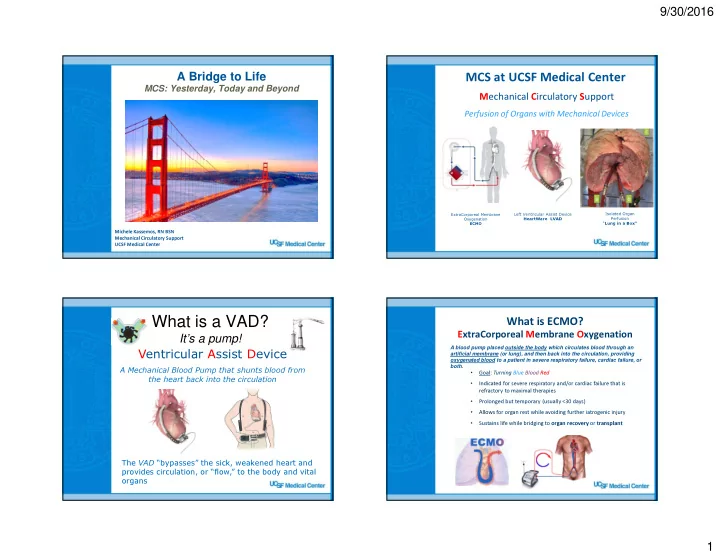
9/30/2016 A Bridge to Life MCS at UCSF Medical Center MCS: Yesterday, Today and Beyond M echanical C irculatory S upport Perfusion of Organs with Mechanical Devices ExtraCorporeal Membrane Left Ventricular Assist Device Isolated Organ Oxygenation HeartWare LVAD Perfusion ECMO “ Lung in a Box” Michele Kassemos, RN BSN Mechanical Circulatory Support UCSF Medical Center What is a VAD? What is ECMO? It’s a pump! ExtraCorporeal Membrane Oxygenation A blood pump placed outside the body which circulates blood through an artificial membrane (or lung), and then back into the circulation, providing Ventricular Assist Device oxygenated blood to a patient in severe respiratory failure, cardiac failure, or both. A Mechanical Blood Pump that shunts blood from • Goal: Turning Blue Blood Red the heart back into the circulation • Indicated for severe respiratory and/or cardiac failure that is refractory to maximal therapies • Prolonged but temporary (usually <30 days) • Allows for organ rest while avoiding further iatrogenic injury • Sustains life while bridging to organ recovery or transplant The VAD “bypasses” the sick, weakened heart and provides circulation, or “flow,” to the body and vital organs 1
9/30/2016 Historical Context The early concepts of Mechanical Life Support � 1813 - Le Gallois - first descriptions of mechanical support in rabbits � 1926 – Soviet physician Brukhonenko developed first primitive heart-lung machine " The solution of the problem of the artificial circulation of the whole animal opens the door to the problem of operations on the heart, for example on the valve." Sergei S. Brukhonenko, 1928 Konstantinov, I MD, Alexi-Meskishvili, V MD, PhDb; Sergei S. Brukhonenko: the development of the first heart-lung machine for total body perfusion. Ann ThoracSurg 2000;69:962-966 History of MCS History of MCS Pioneers of Heart & Lung Assist Pioneers of Heart & Lung Assist 1953 - Dr John Gibbon “Father of CPB” 1954-55 – Dr Lillihei First to successfully use CPB for cardiac surgery “Cross Circulation” as biological oxygenator “…the idea occurred to me that if it were possible to remove continuously some of the blue blood from the patient’s swollen veins, put oxygen into the blood and allow carbon dioxide to escape from it, and then to inject continuously the new red blood back into the patient’s arteries, we might have been able to save her life.” Dr Lillihei with pediatric survivor of cardiac surgery using cross circulation JH Gibbon and wife Mali Cross circulation between parent and child using parent as heart/lung machine Miller BJ, Gibbon JH Jr ; Recent advances in the development of a mechanical heart and lung apparatus. Ann Surg 1951 2
9/30/2016 History of MCS History of MCS Pioneers of Heart & Lung Assist Pioneers of Heart & Lung Assist 1966 – Dr M. DeBakey First Successful VAD 1967 – Dr C. Barnard, South Africa • LVAD for failure to wean from CPB • First successful human heart transplant • Pneumatic, paracorporeal pump 1969 – Dr D. Cooley first Total Artificial Heart • Supported for 10 days, organ recovery, discharged • Lt Ventricular aneurysm repair, failure to wean from home CPB • Supported pt for 64 hrs until heart transplant performed • Concept of “Bridging to Transplant ” with MCS is established Historical Context Historical Context 1 st LVAD-to-Cardiac Transplants 1971 – Dr. Don Hill First adult ECMO survivor (Adult ARDS) � 1984 – 1 st successful LVAD-to-transplant with Novacor LVAD Stanford (Oyer MD) � 1984 –LVAD-to-transplant with Thoratec pneumatic paracorporeal LVAD San Francisco (JD Hill) � 1992 - LVAD-to-transplant with HeartMate IP LVAD Texas Heart Institute (Frazier) Santa Barbara, CA 1971 � NIH-funded study stopped after 90% mortality rate in ECMO group � From 1979-1995 Adult ECMO rarely used outside a number of small, dedicated centers HeartMate Pearce- Novacor HeartMate IP Donachey DDC Driver 3
9/30/2016 Historical Context Historical Context Today: Second Generation Pumps VADs Go Mobile in the 90s • 1991 – 1 st successful implant of “untetherable” New millennium brings “Continuous Flow” HeartMate VE LVAD Texas Heart (Frazier) � Rotary pumps (HM II, Jarvik, MicroDebakey) � Centrifugal pumps (HeartWare, CentriMag, Rotoflow) • 1994 – HeartMate XVE LVAD FDA-approved for implantable pump for bridge-to-transplant � April 2008 – HM II approved for bridge-to-transplant � Jan 2010 – HM II approved for Destination Therapy � Nov 2012 – HeartWare HVAD approved for bridge to transplant A New Era for Adult ECMO Wait….What Happened to ECMO? 2009 Essentially….nothing much Major Game Changers for Adult ECMO � CESAR Trial – Oct 2009 � H1N1 Influenza A epidemic – Fall of 2009 � Avalon Dual Lumen VV Cannula FDA approved – Jan 2009 2005 1972 Up until early 2000s, ECMO still rarely used other than salvage cases, aka “Hail Mary Pass” 4
9/30/2016 CESAR Trial 2009 Flu Pandemic Conventional Ventilation or ECMO for Severe H1N1 Adult Respiratory Failure • Influenza A virus causing ARDS in rare cases • Conducted from 2001 – 2006 in UK • Study from Australia & New Zealand (JAMA 2009) • Randomized controlled trial • observed an 80% ECMO survival rate of adults w/ H1N1 ARDS • Comparing conventional ventilation vs ECMO in patients w/ ARDS (n=68) • ELSO: • Randomized to either VV ECMO (90 pts) or continuing conventional care at referral hospitals (90 pts) • “Review of the H1N1 data shows 72% survival rate when ECMO is • ECMO group: 57 of 90 (63%) met endpoint instituted within 6 days of intubation; 31% when pt intubated for 7 days or longer” • Conventional ventilatory group: 41 of 87 (47%) met end point Why Game Changer? Why a Game Changer? • 70-80 % Survival if ECMO initiated sooner rather than later • 63 % survival rate – demonstrating efficacy in adults • Efficacy in ECMO as tx for Acute Respiratory Distress • Data to support increased survival in transporting to ECMO centers Syndrome in adults Peek et al (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomized controlled trial. Lancet UCSF Develops Mobile ECMO Team Dual lumen VV ECMO Cannula Only Center in Region � During H1N1, and post CESAR Trial, ECMO referrals exploded � Patient’s too unstable for transport • Avalon Elite � “ECMO TO GO” team formed in 2009 under Charles � VV ECMO cannula for respiratory failure Hoopes and Jasleen Kukreja � Cannulation via Rt Internal Jugular � Leaving pt ambulatory � Draining from two points (SVC & IVC) � Flows directly back into Rt Atrium � Very little recirculation rate(2%) Why a Game Changer? � Improving candidacy for transplant � Allows for ambulation � Minimally invasive – no thoracotomy, no major artery cannulation 5
9/30/2016 UCSF at the forefront of bringing ECMO History of Heart & Lung Asist from this…. UCSF makes it’s mark � 2/26/2009 – Dr. Charles Hoopes @ UCSF is the first surgeon in US to place Avalon Cath for Ambulatory Lung Assist � UCSF 1 st ECMO center in the US using ambulatory ECMO as a bridge to lung transplant To THIS!! Central VA ECMO “Ambulatory Bypass” “Ambulatory Oxy RVAD” PA to LA central cannulation w/ VAD cannulae (PHTN, RV Failure, hypoxia, s/p PEA arrest � to Bl lung Tx “Ambulatory Lung Assist” “Ambulatory Oxy RVAD” VV ECMO with DLC. End- PA to Lt Atrium w/ tunneled Stage CF, Bridged to Bilateral VAD cannulae. Lung Transplant. 33 days on (ILD, RV Failure, hypoxia -> support. bridged to bilateral lung tx “Walking Bypass” after 42 days of support). RA to AO central cannulation w/ VAD cannulae (PHTN, RV failure, s/p PEA arrest � to Heart/Lung Tx) 6
9/30/2016 Happy Endings Central “Oxy RVAD” “Oxy RVAD” PA to LA central cannulation w/ VAD cannulae (PHTN, RV failure, Hypoxia, s/p PEA arrest � to Bil Lung Tx) Pipeline Technology Pipeline Technology What’s next? What’s next? HeartWare Pipeline HeartWare mVAD – Continuous Flow Axial Pump � 70% smaller than HVAD � Reduced incision size � Reduced complications (bleeding, RVF) � Preservation of sternum � Full or partial support � Weaning � Intervention in earlier stages of disease � Gimbaled Sewing Ring � Depth adjustment supporting smaller heart chambers � mVAD Advantage Trial in progress � Multi-center single arm trial � 70 patients at 11 sites in Australis/Europe MVAD Video 7
9/30/2016 Pipeline Technology Percutaneous Right-Sided Support Impella RP HeartMate III – Continuous Flow Impella RP Right-sided percutaneous support Centrifugal Pump � Short-term support of RV � Superior Hematological Compatibility � Minimized shear stress � Support RV post LVAD surgery � Minimizes stasis � Minimize interactions between blood and foreign surface � Full support � 2 – 10 lpm flow � Intervention in earlier stages of disease � Modular Driveline � Momentum III Trial in progress � Multi-center trial � Comercialized in Europe w/ over 200 implants � Ongoing studies in 5 sites in US Tandem Lung ECMO Circuits and Components Ambulatory “Oxy-RVAD” they’ve come a long way, Baby � Dual Lumen Cannula � Inflow port: RA � Outflow port: PA � Minimally invasive approach 8
9/30/2016 Thank You for Your Time 9
Recommend
More recommend