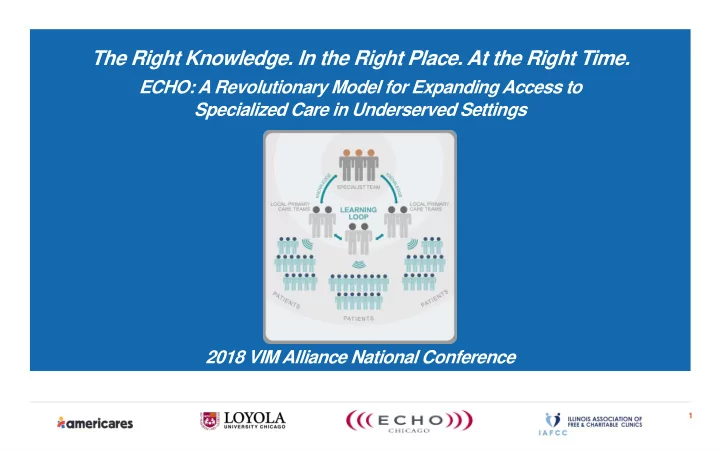
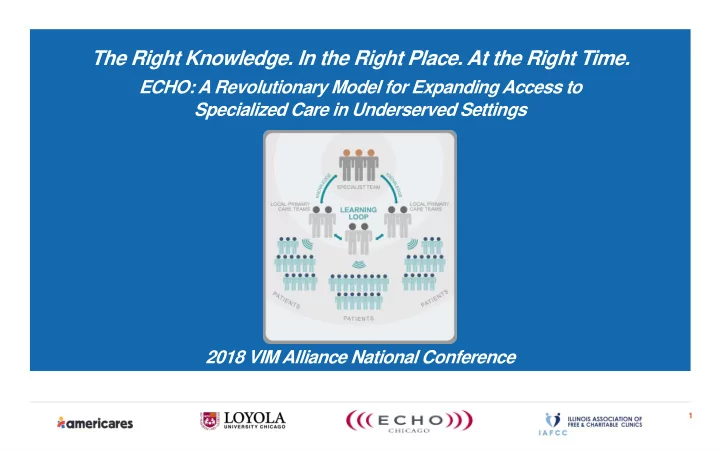
The Right Knowledge. In the Right Place. At the Right Time. ECHO: A Revolutionary Model for Expanding Access to Specialized Care in Underserved Settings 2018 VIM Alliance National Conference 1
Objectives 1. Describe the ECHO model and its implementation in free and charitable clinics. 2. Recognize the resources the ECHO model offers to clinics in underserved settings. 3. Discuss the impact of the model on education, provider knowledge, patient health outcomes and clinic-wide changes in a pilot study involving 5 free and charitable clinics. 4. Identify, locate and consider opportunities to participate in ECHO by collaborating with local ECHO hubs across the country. 2
Americares, Loyola University Chicago, ECHO-Chicago, and IAFCC Free and Charitable Clinics (FCC) Initiative • Collaboration among four strategic partners • Implemented in five FCCs in Illinois • Designed exclusively for FCC providers • Goal: Assess feasibility and effectiveness of ECHO model in FCC setting for hypertension Funding provided by the GE Foundation 3
ECHO-Chicago Mission The mission of ECHO-Chicago is to establish a robust community-based knowledge network that reduces the serious health disparities affecting children and adults in underserved communities. 4
ECHO: How it Works Extension for Community Health Outcomes (ECHO) uses case-based, iterative, telehealth delivered via high-grade videoconference technology to bring advanced training and support to community-based primary care providers leveraging university-based specialists. Image courtesy of ECHO Institute 5
6
7
Example Disease Areas from ECHO-Chicago Resistant hypertension Oct 2010 Pediatric ADHD Dec 2011 Risk based approach to women’s health Jan 2012 Pediatric obesity & comorbidities Mar 2013 Apr 2014 Hepatitis C Feb 2015 Child & youth epilepsy (not active) Feb 2016 Geriatrics Jun 2016 Behavioral health integration (system change) Sep 2016 Complex pediatric asthma Jan 2017 Hepatitis C case management Behavioral health (clinic management) Feb 2017 8
Characteristics of Participating Clinics SITE A SITE C SITE D SITE B SITE E URBAN SURBURBAN SURBURBAN URBAN SURBURBAN $3.0 million Budget $1.2 million Budget $380,000 Budget $580,000 Budget $571,000 Budget 10,5000 patients 2,054 patients 510 patients 1,500 patients ~1,000 patients 23,000 annual 7,500 annual visits 1,825 annual visits 10,000 annual ~6,000 annual visits visits visits 2 NPs, 4 RNs 1 NP, 1 RN 1 NP, 2 RNs 2 NPs 5 RNs Paid FTEs Paid FTEs Paid FTEs Paid FTEs Paid FTEs 36 Vol. Providers 47 Vol. Providers 292 Vol. Providers 146 Vol. Providers 83 Vol. Providers 205 HTN patients 81 HTN patients 294 HTN patients 260 HTN patients 91 HTN patients ECHO Participants: ECHO Participants: ECHO Participants: ECHO Participants: ECHO Participants: 1 NP (paid P/T) 1 NP (paid ~F/T) 1 NP (paid F/T) 2 NPs (F/T) 1 NP (vol) 2 RN (paid P/T) 2 MD (vol) 1 RN (paid F/T) 1 RN (paid P/T) 1 MD (vol) 9
FCCs and ECHO 10
Focus: Resistant Hypertension • Disease area selected through collaborative discussion with FCC partners; common diagnosis in FCCs • Leverage existing ECHO-Chicago infrastructure, experience and disease specific resources • Mixed-method approach • Quantitative analysis of patient and provider outcomes • BP control • Medication management • Qualitative/descriptive analysis of provider practices and clinic processes 11
ECHO-Chicago FCC Project • Aim 1: Determine the feasibility of implementing the ECHO-Chicago intervention in free and charitable clinics • Aim 2: Compare the effectiveness of the ECHO-Chicago intervention with conventional care in free and charitable clinics 12
13
Preliminary Findings
Study Timeline Study period 10/1/2015 and 5/10/2017 (586 day/ 1.6 year period) Total visits occurring in this time period: 4,849 15
Is ECHO Feasible in FCCs? 16
ECHO-Chicago HTN FCC Participants Total number of participating clinicians = 12 *1 RN participated informally All ECHO (2016-17) FCC 100% 90% 80% 70% 60% 50% 50% 47% 38% 40% 33% 30% 20% 17% 10% 6% 6% 3% 0% Nurse Practitioner Physician Nurse Physician Assistant Clinical Pharmacist n=6 n=2 n=4* n=0 n=0 17
ECHO-Chicago HTN FCC Rates of Participation Total # of participants Mean Attendance (# of sessions) All ECHO HTN Participants (2016-17) 276 9 FCC ECHO HTN Participants 12 11 (of 12) ALL Participants(2016-17) FCC Participants 50% 45% Percent of total participants 40% 35% 30% 25% 20% 15% 10% 5% 0% 8% 17% 25% 33% 42% 50% 58% 67% 75% 83% 92% 100% Percent of sessions attended (Total 12) 18
Is ECHO Effective in FCCs? • Provider-Level: • Self-Efficacy • Knowledge • Number of blood pressure readings taken • Adherence to guideline-concordant care • Patient-Level: • Reduction in systolic blood pressure • Improvement in blood pressure control • Clinic-Level: • Changes in policies and procedures affecting management of hypertensive patients • Dissemination of knowledge 19
PROVIDER-LEVEL 20
Self-Efficacy ALL ECHO Participants (2016-17) 7.0 6.0 7-point rating scale 5.0 4.0 3.0 1. Identify patients with resistant HTN 2.0 1.0 2. Assess the importance of kidney disease in HTN 0.0 3. Measure blood pressure accurately 1 2 3 4 5 6 7 8 9 4. Manage side effects of HTN medications 5. Work collaboratively with patients to manage HTN FCC Participants 6. Assess and manage comorbidities 7.0 6.0 7. Overall ability to treat patients with resistant HTN 5.0 4.0 8. Select the most appropriate medication(s) 3.0 2.0 9. Educate clinic staff about patients with resistant HTN 1.0 0.0 1 2 3 4 5 6 7 8 9 Avg. Pre Avg. Post 21
Improving Provider Self-Efficacy ECHO-trained providers emerged as HTN experts at 80% of participating clinics “Our provider has become the expert and a champion for the program in our medical advisory committee and at our board meetings.” “My "new" NP grew so quickly because of the ECHO program. Her learning curve was greatly accelerated. Also, for myself and pharm tech we are much more knowledgeable in the full range of HTN meds and dosing and what are reasonable doses.“ 22
PATIENT-LEVEL 23
Number of Hypertensive Patients by Clinic (n=931 patients) 350 294 300 260 250 Number of Patients 205 200 150 100 91 81 50 0 Clinic A Clinic B Clinic C Clinic D Clinic E 24
Patient Characteristics by Clinic Characteristic Overall Clinic A Clinic B Clinic C Clinic D Clinic E Age (mean) 55 56 53 54 53 54 % Female 55 63 48 58 36 54 Race/Ethnicity % White 35 29 36 37 73 10 % Hispanic 56 67 40 54 21 84 % Black 4 7 16 0 1 4 % Other 5 2 8 9 5 2 % Non-English 64 86 37 51 24 73 Note: Differences across clinics are statistically significant at p<.0001 25
Patient Characteristics by Clinic # of Overall Clinic A Clinic B Clinic C Clinic D Clinic E comorbidities % % % % % % 0 49 35 53 63 57 45 1 40 52 34 32 33 35 2 9 11 9 4 7 14 3 2 1 6 1 2 6 Notes: Maximum # of comorbidities = 19 Differences across clinics are statistically significant at p<.0001 26
Top Comorbidities by Clinic Overall Clinic A Clinic B Clinic C Clinic D Clinic E Comorbidities % % % % % % Diabetes 34 45 19 27 27 50 Diabetes w/ 8 10 8 5 11 6 complications Renal disease 5 7 0 4 9 5 Notes: Maximum # of comorbidities = 19 Differences across clinics are statistically significant at p<.0001 27
Changes in Systolic Blood Pressure by Clinic 200 PreECHO PostECHO 190 180 170 160 150 3.5 7.9 3.8 1.8 140 4.4 4.3 130 120 110 100 90 Overall Clinic A Clinic B Clinic C Clinic D Clinic E “PreECHO” value is the first visit during the pre period and “PostECHO” is the last visit 28
Adjusted Differences in Systolic Blood Pressure Variable Coef SE p-value Change in systolic blood pressure -3.99 2.17 .033 Notes: n=523 having both pre- & post-ECHO visits. Adjusted differences are derived from a regression-based difference-in-difference model that includes clinic sites, age, race, language spoken, and number of comorbidities. Standard errors are robust. We detected a 4 mm/Hg reduction in SBP in patients seen by ECHO-trained providers 29
% of Patients with Controlled Blood Pressure 100 PreECHO PostECHO 90 80 70 62 60 52 50 40 30 20 10 0 Overall Clinic A Clinic B Clinic C Clinic D Clinic E 30
% of Patients with Controlled Blood Pressure by Provider Type 100 100% PreECHO 90 90% PostECHO 80 80% % change 70 70% % of 60 60% % change patients 50 50% 40 40% 30 30% 20 20% 10 10% 0 0% Provider Type Overall Clinic A Clinic B Clinic C Clinic D Clinic E Overall, we observed a 21% increase in patients with controlled blood pressure, but no differences by provider. 31
CLINIC-LEVEL 32
Changing Clinic Processes Clinic Implemented Changed Identified Increased Improved ECHO Trained Patient How BP was new sources Frequency Patient Providers Seen Registry Taken HTN Meds of Visits Education as Experts (100%) (60%) (40%) (80%) Resources (80%) (80%) SITE A SITE B SITE C SITE D SITE E 33
Recommend
More recommend