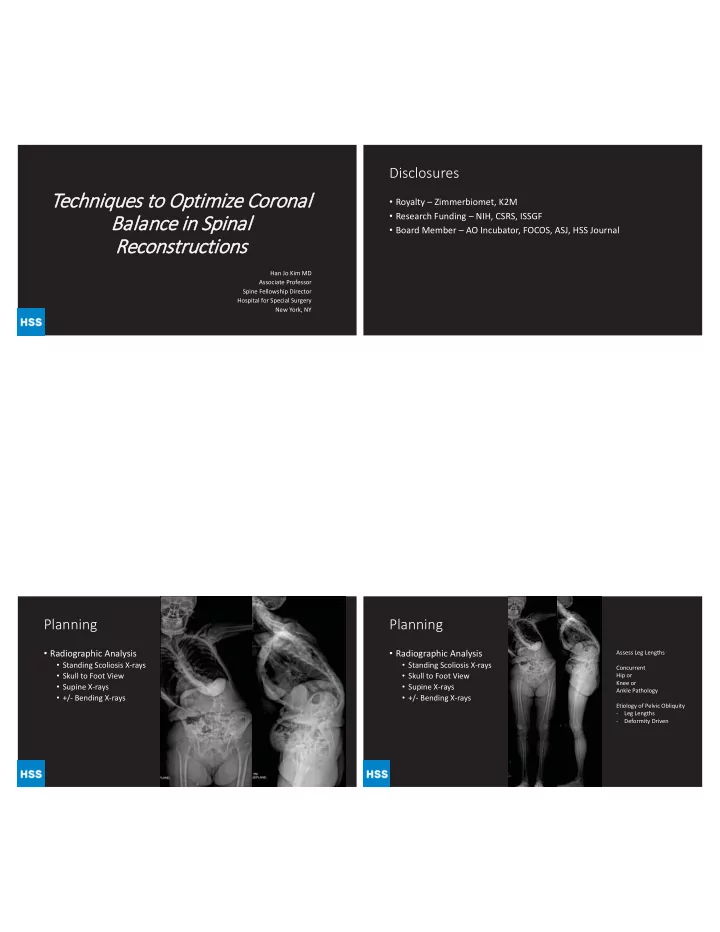
Disclosures Techniques to Optimize Coronal • Royalty – Zimmerbiomet, K2M • Research Funding – NIH, CSRS, ISSGF Balance in Spinal • Board Member – AO Incubator, FOCOS, ASJ, HSS Journal Reconstructions Han Jo Kim MD Associate Professor Spine Fellowship Director Hospital for Special Surgery New York, NY Planning Planning • Radiographic Analysis • Radiographic Analysis Assess Leg Lengths • Standing Scoliosis X-rays • Standing Scoliosis X-rays Concurrent • Skull to Foot View • Skull to Foot View Hip or Knee or • Supine X-rays • Supine X-rays Ankle Pathology • +/- Bending X-rays • +/- Bending X-rays Etiology of Pelvic Obliquity - Leg Lengths - Deformity Driven
Osteotomy Planning Selection • Radiographic Analysis Flexibility • Standing Scoliosis X-rays Assessment • Skull to Foot View • Supine X-rays • +/- Bending X-rays Relationship of PI to Lordosis Osteotomy Selection 45° Low PI • SPO � 11° S1 ~ horizontal • PSO � 33° Large PI Flat Lordosis • Grade 4 Schwab � 40° S1 is tilted 50° • Lumbar • Sagittal Deformities • VCR � 50-70% Correction 45° 83° 20° 45° • Thoracic • Acute/Angular Deformities • >100 Deg 30° 80 80° 8
Relationship of PI to Lordosis Distribution of Lumbar Lordosis versus PI p<0.001 p<0.001 p=0.03 45° Low PI • On average, distal lordosis ~60% S1 ~ horizontal of the total lordosis Large PI Flat Lordosis • Value almost constant across PI S1 is tilted 50° group • Significant association between proximal lordosis and PI 45° 83° 20° 45° • Larger value • More lordotic levels 30° 30 80° 9 10 Goals of the Surgery Case Example • Coronal and Sagittal Balance • 60F with Back Pain • Not Necessarily Cobb Angle! • +/- Decompression • Coronal and Sagittal Decompensation • Fusion • PI: 45 • Minimize EBL and Intra-op • LL: +50 Kyphosis Complications • PT: 35 deg • Avoidance of Neurologic • Coronal Cobb: 66 Complications • SVA +15 cm • Starts with Planning!
Supine X-rays MRI • Element of Rigidity • Element of Rigidity • Will need Osteotomy • Will need Osteotomy • CT – no Fusions • CT – no Fusions • MRI – no Stenosis • MRI – no Stenosis Thinking Process Thinking Process • Lowest Instrumented Vertebrae • Lowest Instrumented Vertebrae • S1 • S1 • S1/Ilium • S1/Ilium • L5 • L5 • Upper Instrumented Vertebrae • Upper Instrumented Vertebrae • UT (T2, T3, T4) • UT (T2, T3, T4) • LT (T9, T10) • LT (T9, T10) • Osteotomy Selection • SPO? • PSO? • VCR? T3
Iliac Screw to “Titrate” Getting the Balance Coronal Balance • SPOs T11-L4 Distraction • Intra-op 36” Cassette until the Pelvis • Still with Significant Left is Leveled Coronal Decompensation Then Place Right Sided Rod and Final Tighten – Locks in Orientation Coronal Plane can be Tricky • 40F Left Leg Pain and Back • Right LLD by 3cm • Correction LL: 32 deg must plan 98 SVA: +5 cm for this PT: 15
94 98 P ATIENT H ISTORY P RE -O PERATIVE I MAGING - 2010 • A Age: 52 yrs • Gender: Female • Functional Status: Fully ambulatory CC: Leftward tilting posture and back pain HPI: 52F who presented after thoracolumbar fusion in 2010 for AIS diagnosed as a teen followed by 2013 revision for bilateral rod After the revision, gradually increasing leftward postural tilt with significant back painbreakage at the distal aspect of her construct. She had no bowel/bladder issues, no radicular pain and no numbness/weakness. PSHx: • 2010 T3-Pelvis fusion Coronal Coronal Benders Sagittal T1 - T5: 26 T1 - T5: 26 -> 9 • 2013 Spinal fusion revision T2-T12: 39 T5 -T10: 59 T5 -T10: 59 -> 49 L1-S1: 56 T10 – L4: 57 T10 – L4: 57 -> 17 with removal of hardware
P RE -O PERATIVE I MAGING P RE P R -O E I MA P RE -O PERATIVE I MAGING RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE RE E E E E PE PE PE PE PE PE PE PE PE PE PE PE PE PE PE P PE PE PE PE PE PE ERA E E E RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA R T RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA RA A A A A A A TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TI TIVE TI TI TI TI TI TI TI TI TI I V MA MA MA MA MA MA MA MA MA MA MA MA MAGI A A A A A A A GI GI GI GI GING GI GI GI GI GI GI GI GI GI GI GI GI GI GI GI GI GI I I NG NG NG NG NG NG NG NG NG NG NG NG NG NG NG NG 71mm SVA 59d PI 31d PT 28d SS 30d LL PI-LL = 29 P OST -O PERATIVE I MAGING P RE -O PERATIVE I MAGING
2yr 2yr 68F f/u f/u /u /u /u u • Back pain • Feels like she is leaning forward • No leg pain • H/O PSF T4-Pelvis (2010) • High Grade Spondy
What would you do? • Surgical Options • 3-Column Osteotomy? Where? • Distal Fixation/Levels? • Proximal Levels?
T2-Pelvis THANK YOU Revision with S1 PSO • hanjokimmd@gmail.com
Recommend
More recommend