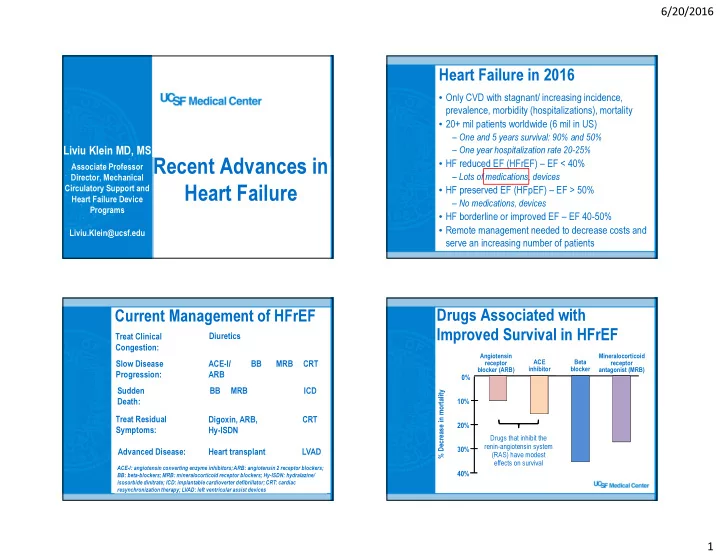
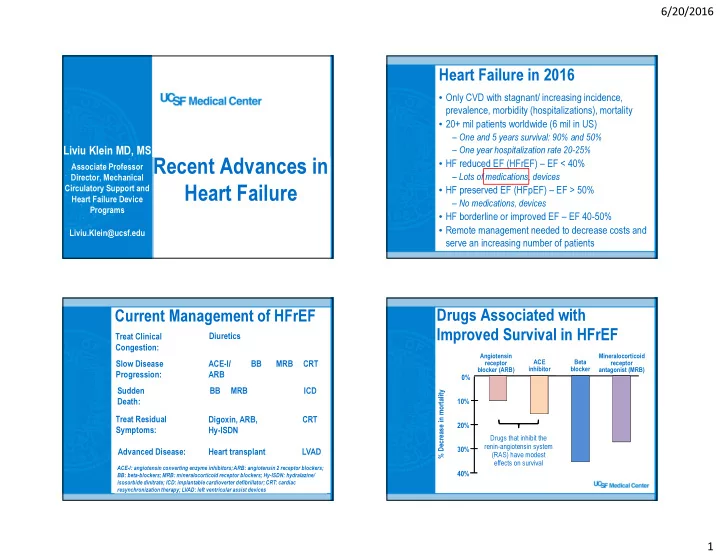
6/20/2016 Heart Failure in 2016 • Only CVD with stagnant/ increasing incidence, prevalence, morbidity (hospitalizations), mortality • 20+ mil patients worldwide (6 mil in US) – One and 5 years survival: 90% and 50% – One year hospitalization rate 20-25% Liviu Klein MD, MS • HF reduced EF (HFrEF) – EF < 40% Recent Advances in Associate Professor Director, Mechanical – Lots of medications, devices Circulatory Support and • HF preserved EF (HFpEF) – EF > 50% Heart Failure Heart Failure Device – No medications, devices Programs • HF borderline or improved EF – EF 40-50% • Remote management needed to decrease costs and Liviu.Klein@ucsf.edu serve an increasing number of patients Drugs Associated with Current Management of HFrEF Improved Survival in HFrEF Diuretics Treat Clinical Congestion: Angiotensin Mineralocorticoid ACE Beta Slow Disease ACE-I/ BB MRB CRT receptor receptor inhibitor blocker blocker (ARB) antagonist (MRB) Progression: ARB 0% % Decrease in mortality Sudden BB MRB ICD Death: 10% Treat Residual Digoxin, ARB, CRT 20% Symptoms: Hy-ISDN Drugs that inhibit the renin-angiotensin system 30% Advanced Disease: Heart transplant LVAD (RAS) have modest effects on survival ACE-I: angiotensin converting enzyme inhibitors; ARB: angiotensin 2 receptor blockers; 40% BB: beta-blockers; MRB: mineralocorticoid receptor blockers; Hy-ISDN: hydralazine/ isosorbide dinitrate; ICD: implantable cardioverter defibrillator; CRT: cardiac resynchronization therapy; LVAD: left ventricular assist devices 1
6/20/2016 Mechanisms of Progression in New Drugs: Mechanisms of Heart Failure Action Myocardial or vascular Neurohormonal activation Vascular tone stress or injury Cardiac fibrosis, hypertrophy Sodium retention Increased activity or Decreased activity or response to maladaptive response to adaptive mechanisms mechanisms Evolution and progression of heart failure Von Lueder TG et al. Nat Rev Cardiol. 2015; 12: 730-740. Von Lueder TG et al. Nat Rev Cardiol. 2015; 12: 730-740. Mechanisms of Progression in PARADIGM-HF Trial Heart Failure Prospective comparison of ARNI with ACEI to Myocardial or vascular Determine Impact on Global Mortality and stress or injury morbidity in Heart Failure trial Increased activity or Decreased activity or LCZ696 Enalapril response to maladaptive response to adaptive 400 mg daily 20 mg daily mechanisms mechanisms Angiotensin Neprilysin SPECIFICALLY DESIGNED TO REPLACE CURRENT USE receptor blocker Inhibitor OF ACE INHIBITORS AND ANGIOTENSIN RECEPTOR BLOCKERS AS THE CORNERSTONE OF THE Evolution and progression TREATMENT OF HEART FAILURE of heart failure Von Lueder TG et al. Nat Rev Cardiol. 2015; 12: 730-740. McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. 2
6/20/2016 PARADIGM-HF Trial Inclusion PARADIGM-HF Trial Design Randomization • NYHA class II-IV heart failure Single-blind run-in period Double-blind period • LV ejection fraction ≤ 40% • BNP ≥ 150 (or NT-proBNP ≥ 600) • Any use of ACE inhibitor or ARB, but able to LCZ696 200 mg BID tolerate stable dose equivalent to at least enalapril 4187 pts. (375 mg daily) Enalapril LCZ696 LCZ696 LCZ696 10 mg daily for at least 4 weeks • Guideline-recommended use of beta-blockers and (1:1 randomization) 10 mg 100 mg 100 mg 200 mg mineralocorticoid receptor antagonists 4212 pts. (18.9 mg daily) BID BID BID BID • SBP ≥ 95 mm Hg, eGFR ≥ 30 ml/min/1.73 m 2 and serum K ≤ 5.4 mEq/L at randomization Enalapril 10 mg BID McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. 2 weeks 1-2 weeks 2-4 weeks PARADIGM-HF Endpoints PARADIGM-HF Baseline Char. • CVD death or first HF hospitalization LCZ696 (n=4187) Enalapril (n=4212) Age (years) 63.8 ± 11.5 63.8 ± 11.3 • Trial powered for 15% CVD mortality reduction Women (%) 21.0% 22.6% • All-cause mortality Ischemic cardiomyopathy (%) 59.9% 60.1% 29.6 ± 6.1 29.4 ± 6.3 LV ejection fraction (%) • Change from baseline to 8 months in the NYHA functional class II / III (%) 71.6%/ 23.1% 69.4%/ 24.9% Systolic blood pressure (mm Hg) 122 ± 15 121 ± 15 Kansas City Cardiomyopathy Questionnaire Heart rate (beats/min) 72 ± 12 73 ± 12 (KCCQ) N-terminal pro-BNP (pg/ml) 1631 (885-3154) 1594 (886-3305) • Time to new onset of atrial fibrillation B-type natriuretic peptide (pg/ml) 255 (155-474) 251 (153-465) History of diabetes 35% 35% • Time to first occurrence of a decline in renal Beta-adrenergic blockers 93.1% 92.9% Mineralocorticoid antagonists 54.2% 57.0% function ICD and/or CRT 21.9% 21.4% McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. 3
6/20/2016 PARADIGM-HF Results: CV PARADIGM-HF Results: CV Death or 1 st HF Hospitalization Death or 1 st HF Hospitalization LCZ696 Enalapril HR P- (n=4187) (n=4212) (95% CI) value CV Death or 0.80 1 st HF 9.7 11.8 < 0.01 (0.73-0.87) Hospitalization 0.80 CV Death 5.9 7.3 < 0.01 (0.71-0.89) 1 st HF 0.79 5.7 6.9 < 0.01 Hospitalization (0.71-0.89) McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. PARADIGM-HF Results: Sudden PARADIGM-HF Results: Heart Cardiac Death Failure Death Desai AS et al. Eur Heart J. 2015; 36: 1990-1997. Desai AS et al. Eur Heart J. 2015; 36: 1990-1997. 4
6/20/2016 PARADIGM-HF Results: PARADIGM-HF Summary: LCZ696 Enalapril Adverse Events p-value (n=4187) (n=4212) In HFrEF, compared to high doses of enalapril: Prospectively identified adverse events LCZ696 was more effective than enalapril in . . . Symptomatic hypotension 588 388 < 0.001 • Reducing the risk of CV death, sudden death and HF death Serum potassium > 6.0 mmol/l 181 236 0.007 by incremental 20% Serum creatinine ≥ 2.5 mg/dl 139 188 0.007 • Reducing the risk of HF hospitalization by incremental 21% Cough 474 601 < 0.001 • Reducing all-cause death by incremental 16% Discontinuation for adverse event 449 516 0.02 • Incrementally improving symptoms and physical limitations Discontinuation for hypotension 36 29 NS LCZ696 was better tolerated than enalapril . . . Discontinuation for hyperkalemia 11 15 NS • Less likely to cause cough, hyper K or renal impairment Discontinuation for renal impairment 29 59 0.001 • Less likely to be discontinued due to an adverse event Angioedema (adjudicated) • Not more likely to cause serious angioedema Medications, no hospitalization 16 9 NS Hospitalized; no airway compromise 3 1 NS • More hypotension, but no increase in drug discontinuation McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. McMurray JJ et al. N Engl J Med. 2014; 371: 993-1004. ARNI Doubles Survival in HFrEF Caveats of Using ARNI Compared to ACE-I/ ARBs • Stop ACE-I for 48 hrs. prior Angiotensin Angiotensin Receptor • Make sure patient is not “dry” (adjust diuretics) Receptor ACE Neprilysin Blockers (ARB) Inhibitors (ACE-I) Inhibitor (ARNI) • Start with low dose (24/26 mg BID) and increase 0% dose slowly (every 7-10 days) as tolerated if patients’ % Decrease in Mortality 15% 18% baseline BP < 120 mmHg 10% • If BP > 120 mmHg, one can start at higher dose (49/ 51 mg BID) and titrate up faster 20% • For patients that cannot achieve target dose (98/102 20% 30% mg BID), check NT-pro BNP and echocardiogram (LV size, LVEF) after 3 months on therapy to assess benefit 40% 5
6/20/2016 ARNI in HFpEF: PARAMOUNT Future Management of HFrEF and PARAGON Diuretics Treat Congestion: Slow Disease ARNI BB MRB CRT Progression: Sudden ARNI BB MRB ICD Death: Stay tuned: fall 2019 Treat Residual Digoxin, ARB, CRT Symptoms: Hy-ISDN Advanced Disease: Heart transplant LVAD ACE-I: angiotensin converting enzyme inhibitors; ARB: angiotensin 2 receptor blockers; ARNI: angiotensin receptor blocker and neprilysin inhibitor; BB: beta-blockers; MRB: mineralocorticoid receptor blockers; Hy-ISDN: hydralazine/ isosorbide dinitrate; ICD: implantable cardioverter defibrillator; CRT: cardiac resynchronization therapy; LVAD: Solomon SD et al. Lancet. 2012; 380: 1387-1395. left ventricular assist devices Heart Failure Hospitalizations: Heart Failure in 2016 1 Million and Counting…. • Only CVD with stagnant/ increasing incidence, prevalence, morbidity (hospitalizations), mortality • 20+ mil patients worldwide (6 mil in US) – One and 5 years survival: 90% and 50% – One year hospitalization rate 20-25% • HF reduced EF (HFrEF) – EF < 40% – Lots of medications, devices • HF preserved EF (HFpEF) – EF > 50% – No medications, devices • HF borderline or improved EF – EF 40-50% • Remote management needed to decrease costs and serve an increasing number of patients Go AS et al. Circulation. 2014; 129: e28-e292. 6
6/20/2016 Heart Failure Hospitalizations: Timing of Heart Failure Re- All Roads Lead to Rome Hospitalizations: Dharmarajan K et al. JAMA. 2013; 309: 355-363. Dharmarajan K et al. JAMA. 2013; 309: 355-363. Heart Failure Signs/ Symptoms High Mortality Post Discharge for Heart Failure Hospitalization in Hospitalized Patients Admission Discharge Symptoms (%) Dyspnea on exertion 79 58 Dyspnea at rest 42 5 Orthopnea 50 12 PND 33 4 Fatigue 53 57 Signs (%) JVP > 8 cm 33 6 Rales 57 13 S3 gallop 20 6 Edema > 2+ 50 13 Solomon SD et al. Circulation. 2007; 116: 1482-1487. Gattis WA et al. J Am Coll Cardiol. 2004; 43: 1534-1540. 7
Recommend
More recommend