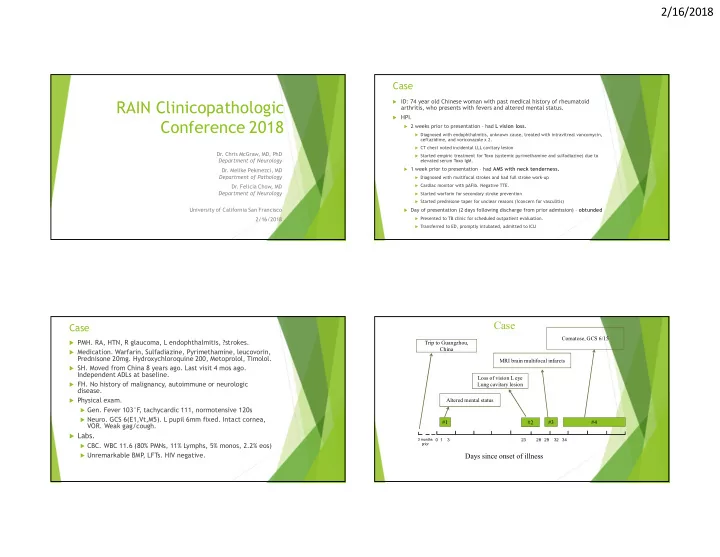
2/16/2018 Case RAIN Clinicopathologic ID: 74 year old Chinese woman with past medical history of rheumatoid arthritis, who presents with fevers and altered mental status. HPI. Conference 2018 2 weeks prior to presentation – had L vision loss. Diagnosed with endophthalmitis, unknown cause, treated with intravitreal vancomycin, ceftazidime, and voriconazole x 2. CT chest noted incidental LLL cavitary lesion Dr. Chris McGraw, MD, PhD Started empiric treatment for Toxo (systemic pyrimethamine and sulfadiazine) due to Department of Neurology elevated serum Toxo IgM. 1 week prior to presentation – had AMS with neck tenderness. Dr. Melike Pekmezci, MD Department of Pathology Diagnosed with multifocal strokes and had full stroke work-up Dr. Felicia Chow, MD Cardiac monitor with pAFib. Negative TTE. Department of Neurology Started warfarin for secondary stroke prevention Started prednisone taper for unclear reasons (?concern for vasculitis) University of California San Francisco Day of presentation (2 days following discharge from prior admission) – obtunded 2/16/2018 Presented to TB clinic for scheduled outpatient evaluation. Transferred to ED, promptly intubated, admitted to ICU Case Case Comatose, GCS 6/15 PMH. RA, HTN, R glaucoma, L endophthalmitis, ?strokes. Trip to Guangzhou, China Medication. Warfarin, Sulfadiazine, Pyrimethamine, leucovorin, Prednisone 20mg. Hydroxychloroquine 200, Metoprolol, Timolol. MRI brain multifocal infarcts SH. Moved from China 8 years ago. Last visit 4 mos ago. Independent ADLs at baseline. Loss of vision L eye FH. No history of malignancy, autoimmune or neurologic Lung cavitary lesion disease. Physical exam. Altered mental status Gen. Fever 103°F , tachycardic 111, normotensive 120s Neuro. GCS 6(E1,Vt,M5). L pupil 6mm fixed. Intact cornea, #1 #3 #4 #2 VOR. Weak gag/cough. Labs. 3 months 0 1 3 23 28 29 32 34 CBC. WBC 11.6 (80% PMNs, 11% Lymphs, 5% monos, 2.2% eos) prior Unremarkable BMP , LFTs. HIV negative. Days since onset of illness 1
2/16/2018 Initial thoughts? MRI Brain on admission Dr. Felicia Chow T2 FLAIR 16/28 28/28 27/28 26/28 25/28 24/28 23/28 22/28 21/28 20/28 19/28 18/28 17/28 15/28 1/28 13/28 12/28 11/28 10/28 9/28 8/28 7/28 6/28 5/28 4/28 3/28 2/28 14/28 MRI Brain on admission MRI Brain on admission T2 TRACE T1 PRE + POST 2/69 48/69 53/69 52/69 51/69 3/69 49/69 46/69 47/69 55/69 45/69 44/69 43/69 42/69 41/69 54/69 57/69 56/69 39/69 58/69 59/69 60/69 61/69 62/69 63/69 64/69 65/69 66/69 67/69 68/69 69/69 1/69 40/69 50/69 38/69 11/69 17/69 16/69 15/69 14/69 13/69 12/69 10/69 19/69 9/69 37/69 7/69 6/69 5/69 4/69 18/69 8/69 20/69 30/69 36/69 21/69 35/69 34/69 32/69 31/69 33/69 29/69 23/69 27/69 26/69 22/69 25/69 24/69 28/69 17/25 18/25 19/25 20/25 23/25 21/25 22/25 15/25 24/25 25/25 16/25 11/25 14/25 13/25 12/25 10/25 9/25 8/25 7/25 5/25 4/25 3/25 2/25 1/25 6/25 2
2/16/2018 Routine Labs Microbiology Hospital course – initial treatment Basic metabolic panel Na 146, K 4.8, CL 118, CO2 22, BUN 40, Creat Cerebrospinal fluid (CSF) 0.99, EGFR 55 #1 Appearance, cell Clear, WBC 347H (57% PMN, Complete blood count WBC 17.0 (90% neut, 5% lymph, 2.5% monos, count, diff, glucose, 11%Mono, 31% Lympho, 3% eos), Initial work-up concerning for toxoplasmosis vs 0.3% eos). Hb 9.2, MCV 89.5, Plts 165. protein RBC 13, glc 30L, protein 71H. 72 H Ammonia nocardia abscesses > TB meningoencephalitis Gram stain. Many PMNs, no organisms. TSH 0.08 (uU/mL) L Bacterial/fungal/AFB Negative Free T4 0.30 (ng/dL) L Empiric antibiotics covering toxo + nocardia: Cryptococcal Ag Negative (CrAg) Rheumatological Toxo PCR Negative Ampicillin 2g q6 ANA 1:640 H CSF VDRL Non reactive Rheumatoid Factor 429 H Cefepime 2g Q12 Negative CSF VZV PCR/IgG/IgM 151.2 H CRP Metronidazole 500 q8 #2 Appearance, cell Clear, WBC 123H (50% PMN, 17% Microbiology (HD#9) count, diff, glucose, mono, 30% lympho, 3% eos). RBC Vancomycin Serum Blood cultures (multiple) No growth protein 2. Glc 36L, protein 210H Sulfadiazine/Pyrimethamine HIV Ab Negative Mixed inflammatory infiltrate, no Cytology malignant cells Toxo PCR/IgM/IgG Negative Steroids tapered off #3 Appearance, cell Xanthochromic, WBC 123 (50% Negative Coccidioides IgM/IgG (HD#13) count, diff, glucose, PMN, 17% mono, 30% lympho, 3% AFB smear protein eos). RBC 2, glc 36L, prot 210H. Negative x 3 RPR Non reactive Diagnostic imaging Trach No organisms, no Chest CT (OSH) Gram stain/Culture LLL cavitary lesion aspirate growth. Transthoracic No e/o valvular disease MTB PCR Negative Echocardiogram Urine Histoplasma Ag Negative CT Angio No flow limiting stenoses Repeat MRI Brain on Day 10 of hospitalization T2 FLAIR Hospital course – response to treatment Patient continued to decline rapidly over the 1 st 10 days of hospitalization HD#1 Intermittently febrile despite antibiotics GCS declining. Initially 6 4 (E1, VT , M3) 2 (E1, VT , M1). Unreactive pupils. Breathing spontaneously. Brain biopsy #1 was obtained on HD#4 – unimpressive. Repeat MRI brain on HD#10. HD#10 3
2/16/2018 Additional thoughts? Repeat MRI Brain on Day 10 of hospitalization Dr. Felicia Chow T1 POST 16/27 27/27 26/27 24/27 23/27 22/27 21/27 20/27 19/27 18/27 17/27 25/27 15/27 6/27 1/27 2/27 3/27 4/27 5/27 14/27 7/27 8/27 9/27 10/27 11/27 12/27 13/27 Hospital course – treatment change Hospital course – response to treatment change Given clinical and radiographic deterioration, Worsening hemodynamic stability empiric treatment for toxo was discontinued, and Worsening mass effect of lesions causing empiric treatment for TB / cocci was started on communicating hydrocephalus HD#10-11. Extraventricular drain (EVD) is placed for CSF diversion Rifampin, Isoniazid, Pyrazinamide, Ethambutol HD#13, with elevated ICPs noted Moxifloxacin Methylprednisone to reduce swelling Amphotericin Worsening exam. Repeat brain biopsy was obtained on HD#11 No cough/gag. Patient transitioned to comfort care and expires HD#17. 4
2/16/2018 Additional thoughts? Additional diagnostic studies Dr. Felicia Chow Two brain biopsies were obtained CSF was sent for next generation sequencing Pathology Biopsy #1 (day 4) Dr. Melike Pekmezci • Clinical • Klebsiella (urine) • Toxoplasmosis IgM+ • Cavitary lung lesion (TB?) • Embolism per initial imaging (? Bacterial source) • Imaging (multiple lesions with reduced diffusion and central enhancement) • Toxoplasmosis • Nocardia • Cryptococcus • PML • Lymphoma/metastasis 5
2/16/2018 Diagnosis: Mild white matter gliosis • No inflammatory component or other features to suggest an infectious process • The findings are mild and nonspecific • Unclear whether the biopsy material is representative of the radiographic abnormality 6
2/16/2018 Biopsy #2 (day 11) • Clinical • Klebsiella (urine) • Toxoplasmosis IgM+ • Cavitary lung lesion (TB?) • Embolism per initial imaging (? Bacterial source) • Imaging (multiple lesions with reduced diffusion and central enhancement) • Toxoplasmosis • Nocardia • Cryptococcus • PML • Lymphoma/metastasis 7
2/16/2018 CD20 CD3 Prebiopsy differential diagnosis • Clinical • Klebsiella (urine) • Toxoplasmosis IgM+ • Cavitary lung lesion (TB?) • Embolism per initial imaging (? Bacterial source) • Imaging (multiple lesions with reduced diffusion and central enhancement) • Toxoplasmosis • Nocardia • Cryptococcus • PML • Lymphoma/metastasis 8
2/16/2018 Vasculitis – Fibrinoid necrosis Vasculitis – Fibrinoid necrosis Lymphocytes, eosinophils, neutrophils Lymphocytes, eosinophils, neutrophils • Primary CNS vasculitis • Primary CNS vasculitis • Primary angiitis of CNS • Systemic diseases • Aβ-related angiitis • PAN, eosinophilic granulomatous polyangiitis • Systemic Lupus Erythematosis • Rheumatoid arthritis Vasculitis – Fibrinoid necrosis Necrotizing vasculitis- SLE Lymphocytes, eosinophils, neutrophils • Primary CNS vasculitis • Systemic diseases • Infectious • Bacterial: Treponema (syphilis), Borrelia (lyme) • Viral: VZV, HCV, HIV • Fungal: Aspergillus, Mucor, Candida, Coccidioides 9
2/16/2018 Vasculitis – Fibrinoid necrosis Aspergillus Lymphocytes, eosinophils, neutrophils • Primary CNS vasculitis • Systemic diseases • Infectious • Bacterial: Treponema (syphilis), Borrelia (lyme) • Viral: VZV, HCV, HIV • Fungal: Aspergillus, Mucor, Candida, Coccidioides • Protozoal: Toxoplasmosis, Trypanosomiasis, Amebiasis Vasculitis – Fibrinoid necrosis Toxoplasmosis Lymphocytes, eosinophils, neutrophils • Primary CNS vasculitis • Systemic diseases • Infectious • Bacterial: Treponema (syphilis), Borrelia (lyme) • Viral: VZV, HCV, HIV • Fungal: Aspergillus, Mucor, Candida, Coccidioides • Protozoal: Toxoplasmosis, Trypanosomiasis, Amebiasis • Nematodes: Toxocariasis • Trematodes: Schistosomiasis • Cestodes: Neurocysticercosis- cerebrovascular form 10
Recommend
More recommend