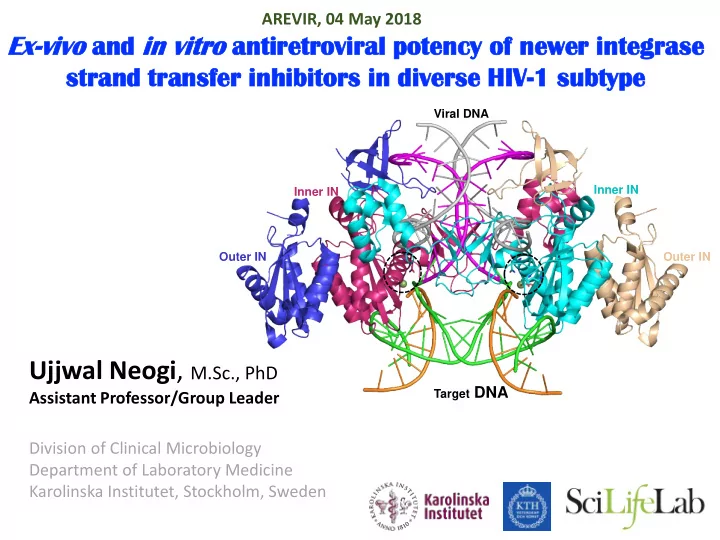
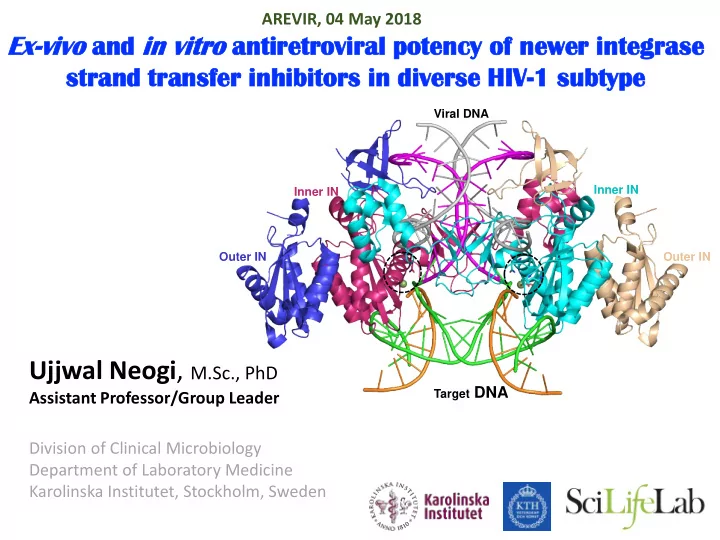
AREVIR, 04 May 2018 Ex-vivo vivo and in vi vitr tro antire retroviral ral p potency o y of newer integras rase stra rand tran ansfer i r inhibi bitors i in diverse H HIV-1 s 1 sub ubtype Viral DNA Inner IN Inner IN Outer IN Outer IN Ujjwal Neogi , M.Sc., PhD Target DNA Assistant Professor/Group Leader Division of Clinical Microbiology Department of Laboratory Medicine Karolinska Institutet, Stockholm, Sweden
Ashokkumar M Maike Sperk PhD Students Visiting Researcher Emmanuel Obasa Duncan T Njenda Hemalatha Babu Anoop Ambikan Robert van Domsealer Associated Members Wang Zhang Sara Svensson Naveen Muppani PostDoc Shambhu Aralaguppe
Study Designing: Drugs: RAL, EVG, DTG, CAB and BIC Biochemical Assays: The integrase genes (HXB2: 4230-5096) of four randomly selected INSTI-naïve patients infected by HIV-1B, C, CRF01_AE, and CRF02_AG, respectively, were cloned into the pRSFDuet-integrase vector with N-terminal H 6 -tag, purified and used for inhibition of 3'-end processing (IC 50-3P ) and strand transfer (IC 50-ST ) Virological assay: Drug sensitivity (DSA) for five INSTIs were done using patient-derived integrase or gag-pol genes from subtypes (HIV-1B: n=6; HIV-1C: n=14; HIV-1A1: n=1; HIV- 1CRF_01AE: n=2; HIV-1CRF_AG: n=1) . Clinical Data: Integrase from INSTI-naïve (n=270) and experienced (n=96) patients were sequenced.
In In vi vitro tro inhib ibit ition ion of of stra trand tra ransfer (IC IC 50 ST ) and nd 3’- end nd 50-ST proc ocessin ing activ ivit itie ies (IC IC 50-3P ) • No potential subtype specific difference • DTG, CAB and BIC has slightly better IC 50-ST in non-B subtypes
Ex Ex vi vivo vo drug rug sensitiv ivit ity assa ssay in in TZM ZM-bl bl cell ll li lines F. CAB DTG BIC EVG RAL
Genot otyp ypic Re Resi sist stance Testing ng: Inf InfCare-Coh ohor ort Acquired Drug Resistance Mutations Primary integrase DRM 270 INSTI-naïve individuals, infected with HIV-1B (n=92), C (n=82), 01_AE (n=25), 02_AG (n=15), A1/A2 (n=22), other pure subtypes (n=13), and recombinant forms (CRFs or URFs) (n=21). • One HIV-1B patient had a major primary INSTI-DRM, T66I . • 6.3% (17 of 270) patients had one major accessory DRM: T97A (n=3), E157Q (n=12), or A128T (n=2).
• Absence of major RAMs in the cohort collected before the broad availability of combination antiretroviral therapy (cART) and INSTI in South Africa. • One of 87 samples carried the accessory mutation G140E.
Naturally ally Occur urri ring Pol olymor ymorphis isms ms A1/A2 (n=483) B (n=4379) C (n=1155) 01_AE (n=1581) 02_AG (n=522) 100 90 80 Frequency (%) 70 60 50 40 30 20 10 0 K14R D25E V31I M50I I72V L74M/I F100Y L101I T124A K136Q D167E V201I T218I L234I A265V R269K S283G L74M/I K136Q R269K S283G D167E A265V F100Y T124A V201I T218I L101I L234I K14R D25E V31I I72V M50I C-terminal domain (CTD) D64 D116 E152 N-terminal domain the catalytic core domain (NTD) (CCD) Rogers et al Manuscript under communication
Muta tati tion t to watch ch: M M50I Tsiang et al Antimicrob Agents Chemother. 2016 vDNA M50/I50 Rogers et al Manuscript under communication
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG,
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG, • No significant difference between the newer INSTIs was seen with regard to efficacy on various subtypes.
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG, • No significant difference between the newer INSTIs was seen with regard to efficacy on various subtypes. • Patient derived sequences from INSTI-naïve individuals both in Swedish cohort and South African cohort have very low prevalence of primary INSTI DRM by Sanger Sequencing.
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG, • No significant difference between the newer INSTIs was seen with regard to efficacy on various subtypes. • Patient derived sequences from INSTI-naïve individuals both in Swedish cohort and South African cohort have very low prevalence of primary INSTI DRM by Sanger Sequencing. • There are five patients in Sweden who has high level of resistance to all INSTIs.
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG, • No significant difference between the newer INSTIs was seen with regard to efficacy on various subtypes. • Patient derived sequences from INSTI-naïve individuals both in Swedish cohort and South African cohort have very low prevalence of primary INSTI DRM by Sanger Sequencing. • There are five patients in Sweden who has high level of resistance to all INSTIs. • The relatively high rate of accessory INSTI mutation (6.3% in Swedish Cohort) but not in South African cohort. Accessory mutations: 15.1% 23.1% in HIV-1A, 8.7% HIV-1C, 11.6% HIV-1D, 25% HIV-1G and 23.8% in recombinants.
Con onclusion ons • DTG, CAB, and BIC had higher antiretroviral potency not only in HIV-1B but also in non-B subtypes compared to RAL and EVG, • No significant difference between the newer INSTIs was seen with regard to efficacy on various subtypes. • Patient derived sequences from INSTI-naïve individuals both in Swedish cohort and South African cohort have very low prevalence of primary INSTI DRM. • There are five patients in Sweden who has high level of resistance to all INSTIs. • The relatively high rate of major accessory INSTI mutation (6.3% in Swedish Cohort) but not in South African cohort. • Naturally occurring polymorphisms in the catalytic core domains mainly near the active sites (D64, D116 and E152) and M50I may affect the stability of the enzyme subsequently the DNA binding affinity followed by drug binding.
Understanding minor pol mutation in HICs and LMICs Study sites and sample collection Treatment First line Failure Second line failure Third Line Country Status Naive (NRTIs+NNRTI) (NRTIs+ PI/r) (NRTI+RAL) South Africa 30 30 30 15* PCR Completed Sample Kenya 30 30 30 ? collection going on Samples are Tanzania 30 30 30 ? already stored Sample Cameroon 30 30 30 ? collection going on Samples are India 30 ? ? ? already stored Ethiopia 30 30 30 ? To be started Sample Sweden 200 ? ? ? collection started *All the samples will have clinical information, mostly from private clinics
Methods and sensitivity Success: A1 (/A1 like) B C D AE G AG Other-CRF Swedish Cohort : 91% (49/54) 10% South African Cohort: 80% (84/106) 19% 6% 8% 16% 16% 4% 21%
High t h thro hroug ughp hput ut s sequenci cing MiDRM pol
Anders Sönnerborg Piotr Nowak Establishment Grant Sweden-China Asso. Prof. Kamlendra Singh, University of Missouri, US Dr. Luke Elisabeth Hanna, NIRT, Chennai Prof. Thomas Klimkait, University of Basel, Switzerland Dr. Graeme Jacobs, Stellenbosch University Dr Christa Kasang, Mwanza, Tanzania Dr. George Mondinde Ikomey, University of Yaoundé, Cameron Dr. Marc Noguera Julian, Institut de Recerca de la SIDA - IrsiCaixa Prof. Stefan Sarafianos, Emory University, US Jonas Söderquist’s Stipendium for Experimental Virology and Immunology Research-2016
Recommend
More recommend