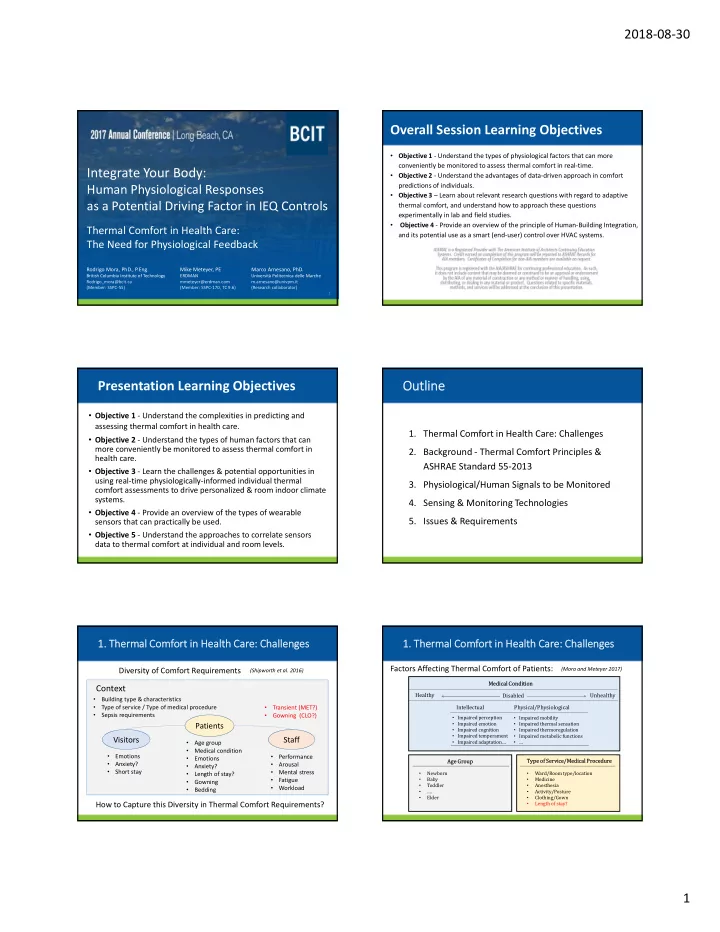
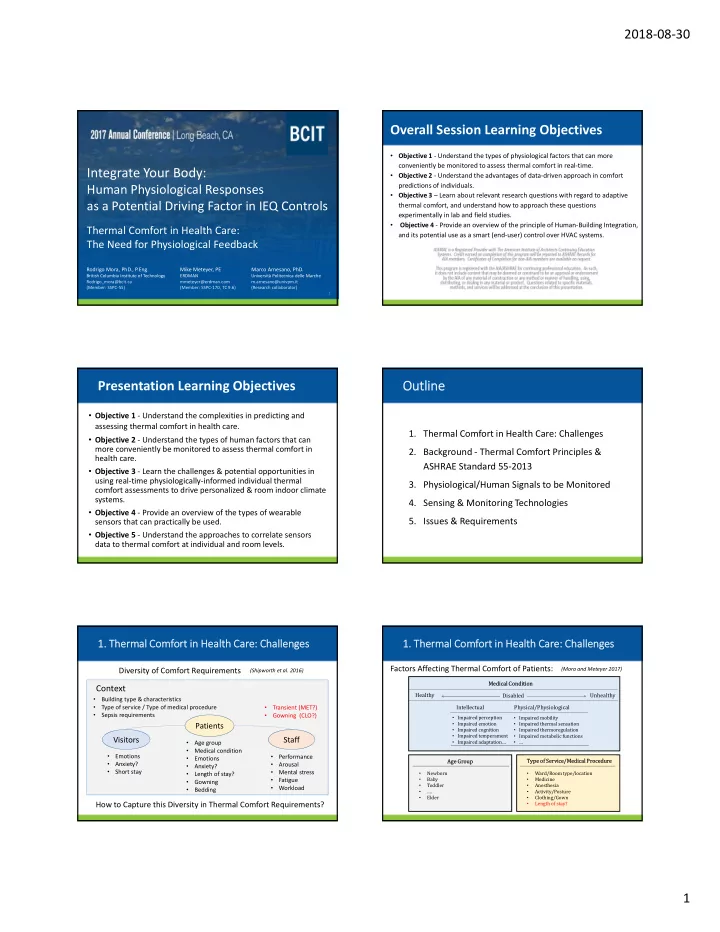
2018‐08‐30 Overall Session Learning Objectives • Objective 1 ‐ Understand the types of physiological factors that can more conveniently be monitored to assess thermal comfort in real‐time. Integrate Your Body: • Objective 2 ‐ Understand the advantages of data‐driven approach in comfort predictions of individuals. Human Physiological Responses • Objective 3 – Learn about relevant research questions with regard to adaptive as a Potential Driving Factor in IEQ Controls thermal comfort, and understand how to approach these questions experimentally in lab and field studies. • Objective 4 ‐ Provide an overview of the principle of Human‐Building Integration, Thermal Comfort in Health Care: and its potential use as a smart (end‐user) control over HVAC systems. The Need for Physiological Feedback Rodrigo Mora, PhD., P.Eng. Mike Meteyer, PE Marco Arnesano, PhD. British Columbia Institute of Technology ERDMAN Università Politecnica delle Marche Rodrigo_mora@bcit.ca mmeteyer@erdman.com m.arnesano@univpm.it (Member: SSPC‐55) (Member: SSPC‐170, TC 9.6) (Research collaborator) 1 Presentation Learning Objectives Outline • Objective 1 ‐ Understand the complexities in predicting and assessing thermal comfort in health care. 1. Thermal Comfort in Health Care: Challenges • Objective 2 ‐ Understand the types of human factors that can more conveniently be monitored to assess thermal comfort in 2. Background ‐ Thermal Comfort Principles & health care. ASHRAE Standard 55‐2013 • Objective 3 ‐ Learn the challenges & potential opportunities in using real‐time physiologically‐informed individual thermal 3. Physiological/Human Signals to be Monitored comfort assessments to drive personalized & room indoor climate systems. 4. Sensing & Monitoring Technologies • Objective 4 ‐ Provide an overview of the types of wearable 5. Issues & Requirements sensors that can practically be used. • Objective 5 ‐ Understand the approaches to correlate sensors data to thermal comfort at individual and room levels. 1. Thermal Comfort in Health Care: Challenges 1. Thermal Comfort in Health Care: Challenges Factors Affecting Thermal Comfort of Patients: Diversity of Comfort Requirements (Mora and Meteyer 2017) (Shipworth et al. 2016) Medical Condition Context Healthy Unhealthy Disabled • Building type & characteristics • Type of service / Type of medical procedure • Transient (MET?) Intellectual Physical/Physiological • • Sepsis requirements Gowning (CLO?) • Impaired perception • Impaired mobility • Impaired emotion • Impaired thermal sensation Patients • Impaired cognition • Impaired thermoregulation • Impaired temperament • Impaired metabolic functions Visitors Staff • Impaired adaptation… • Age group • … • Medical condition • • Emotions Performance • Emotions Type of Service/Medical Procedure Age Group • Anxiety? • Arousal • Anxiety? • Short stay • • Mental stress • Newborn • Ward/Room type/location Length of stay? • • Baby • Medicine Fatigue • Gowning Toddler Anesthesia • • • Workload • Bedding • …. • Activity/Posture • Elder • Clothing/Gown How to Capture this Diversity in Thermal Comfort Requirements? • Length of stay? 1
2018‐08‐30 1. Thermal Comfort in Health Care: Challenges 1. Thermal Comfort in Health Care: Challenges People with Physical Disabilities Environment Effects on People (Assisted Living) “Of particular importance is the use of the adaptive approach for “We feel that enough physiological information on the effects on people with physical disabilities. The present research has led to indoor temperature on health has been gathered to start putting hypotheses that suggest that thermal comfort requirements for this knowledge into practice. Therefore, the question rises: how can people with physical disabilities should take account of the this knowledge be translated into the built environment?” restricted ability of people to adapt to the thermal environment. ” (Lichtenbelt et al. 2016) (Parsons 2002) “Research in the UK and elsewhere has highlighted that older “For babies, children, the sick and the pregnant there is a need for people are particularly vulnerable to negative health effects of systematic research into the interaction of the six basic parameters overheating” and thermal comfort. ” (Gupta et al. 2016) (Parsons 2002) 2. Background ‐ Thermal Comfort & ASHRAE Standard 55‐2013 2. Background ‐ Thermal Comfort & ASHRAE Standard 55‐2013 Mechanically Conditioned Naturally Conditioned Context 10� 50� � ���� ������� ����. � 33.5� �92�� Building Identify space types Objective • Social Identify space types Measurements Environment • Climate ������ ��� ������������ Representative Occupant(s) • ������� ����������� Building type ������� ����������� • Building characteristics Environmental factors Personal factors • Level of control Environmental & Personal factors � � , � � , �̅ � , �� �������� ��� , �������� ����� ���������� ���� ������� ����. Humans ��� ����� � 0.3 �/� �60 ���� ���� �� ����� � 15 ��� 1.0 ��� � � � 2.0 ��� Assumptions: Subjective Physiology Psychology �� ����� ������������: 1.0 � 1.3 ��� � �� � 1.5 ��� Met, Clo Evaluations 0.5 � 1.0 ��� 0.06 � ���� ���������� � 0.25 ��� ����� � 0.2 �/� �40 ���� � � 1.3 ��� Whole‐body Thermal �� Adaptive Comfort Model � �� � 0.7 ��� Balance Model �� ���������� Personal background: Thermoregulation: Subjective Scales: ������� … • Background, motivations • Age • Thermal sensation �� ����. . . �� ����. . . Local • Thermal history Temperature • Gender • Thermal acceptability Discomfort? variations with time? • Expectations on the • Thermal preference • Health condition Direct Solar Indoor Environment on Subject? SET Index: Elevated Air Speed (ERF→MRT) “ Comfort is a construct that exists in our thinking & cannot be measured directly” (Cain 2002) �������� �������? 2. Background ‐ Thermal Comfort & ASHRAE Standard 55‐2013 2. Background ‐ Thermal Comfort & ASHRAE Standard 55‐2013 Rational Model: PMV‐PPD Thermal Comfort Model (Fanger 1970) Local Discomfort: The thermal balance of the human body results in skin temperatures & sweat rates that should be kept within specified ranges, depending on metabolic activity & thermoregulation (physiology), to produce a neutral thermal sensation (sensory Tolerance/Thresholds = f(overall thermal sensation, personal control) psychology) & subsequent conscious thermal satisfaction (cognitive psychology). Temporal thresholds: • Body not far from thermal neutrality • Temperature variations with time: Main Assumptions • Narrow range of environmental conditions • Deviation from neutral (drifts): amplitude • All sweat generated evaporates • Fluctuations: frequency (minutes, hours, days) Calculated Spatial thresholds: Warm thermal imbalance PMV Input (given) Mean Skin • Local discomfort: Temperature Metabolic • Air drafts: ankle, neck Body heat balance Activity • Vertical air temperature difference (stratification): standing, seated Sweat Rate • Radiant thermal asymmetry: cold/warm wall, cold/warm ceiling Cold thermal imbalance • Floor surface temperature Main physiological parameters influencing heat balance 2
Recommend
More recommend