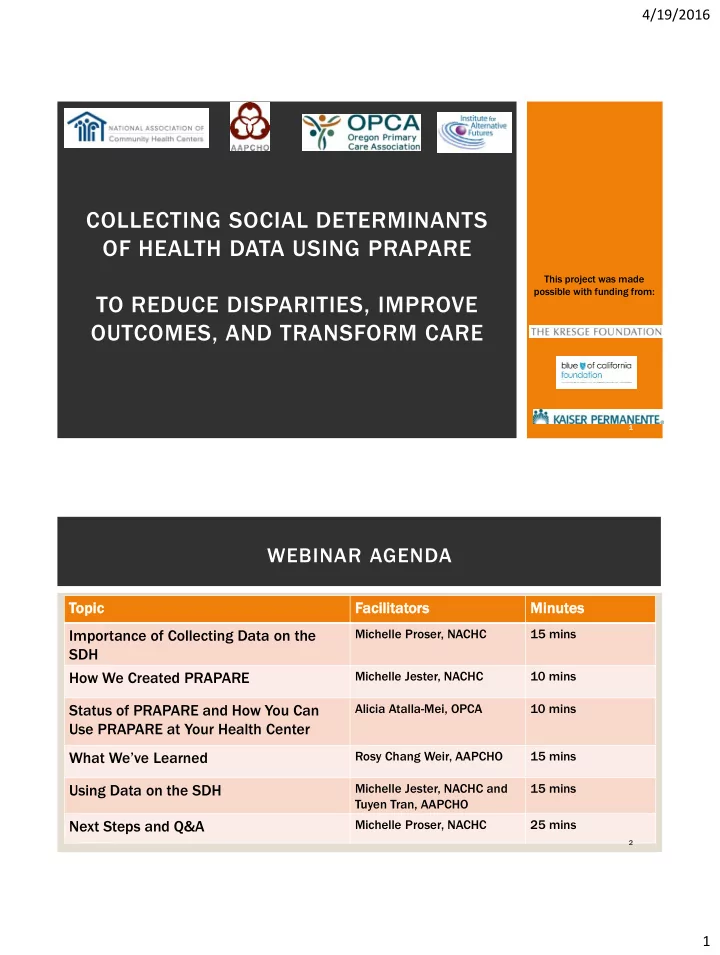
4/19/2016 COLLECTING SOCIAL DETERMINANTS OF HEALTH DATA USING PRAPARE This project was made possible with funding from: TO REDUCE DISPARITIES, IMPROVE OUTCOMES, AND TRANSFORM CARE 1 WEBINAR AGENDA Topic Facilita tator ors Minutes Importance of Collecting Data on the Michelle Proser, NACHC 15 mins SDH How We Created PRAPARE Michelle Jester, NACHC 10 mins Status of PRAPARE and How You Can Alicia Atalla-Mei, OPCA 10 mins Use PRAPARE at Your Health Center Rosy Chang Weir, AAPCHO 15 mins What We’ve Learned Using Data on the SDH Michelle Jester, NACHC and 15 mins Tuyen Tran, AAPCHO Next Steps and Q&A Michelle Proser, NACHC 25 mins 2 1
4/19/2016 WHY IS IT IMPORTANT TO COLLECT STANDARDIZED DATA ON THE SOCIAL DETERMINANTS OF HEALTH? 3 HEALTH, ACCOUNTABILITY & VALUE Under value-based pay environment, providers are held accountable for costs and outcomes Difficult to improve health & wellbeing and deliver value unless we address barriers Current payment systems do not incentivize approaching health holistically and in an integrated fashion Providers serving complex patients often penalized without risk adjustment 4 2
4/19/2016 WHAT IS DRIVING THE NEED TO COLLECT DATA ON THE SOCIAL DETERMINANTS OF HEALTH (SDH)? Figure 1 Are services addressing How well Physical SDH do we Environment (10%) incentivized know our Social and Economic and patients? Factors (40%) sustainable? Are community partnerships adequate Health and Behaviors integrated? (30%) Clinical Care (20%) Bay Area regional Health Inequities Initiative (BARHII). 2008. “Health Inequities in the Bay Area”, accessed November 28, 2012 from 5 http://barhii.org/resources/index.html. PRAPARE: PROTOCOL FOR RESPONDING TO & ASSESSING PATIENT ASSETS, RISKS, & EXPERIENCES Project Goal: To create, implement/pilot test, and promote a national standardized patient risk assessment protocol to assess and address patients’ social determinants of health (SDH). PRAPAR ARE Protoco col to to Assessm ssment t Tool Respond to to Needs To Identi tify Needs • Paper Tool • Implementation and + • EHR Templates Action Toolkit List of Granular • • Examples of Interventions Needs Guidance on how to build • • ICD-10 Z Codes capacity • Workflow Diagrams • Appendix of Resources • Staff Training • Guidance on informing Curriculum policy and payment 6 3
4/19/2016 FROM DATA TO PAYMENT: CONNECTING THE DOTS Local Population State and National Individual Patient Level Level Level Commun unity Understand and Trans nsfor form m Impact Demons nstrat ate Context Patient nts Care Value Impact Upstream Inquiry & New or Negotiate root causes socio- standardized improved for payment of poor ecological data non-clinical change health factors collection interventions, impact enabling Improve Ensure behaviors, Under- services, outcomes, sustainability access, stand extent and patient/staff of outcomes, community of patient & experiences interventions and costs linkages population Lower total complexity cost of care Analyze stand ndar ardized data 7 HOW DID WE CREATE PRAPARE? 8 4
4/19/2016 IDENTIFYING CORE DOMAINS Literature reviews of SDH associations with cost and health outcomes Monitored and/or aligned with national initiatives • HP2020 Used • RWJF County Health Rankings Identified evidence to • ICD-10 15 Core • IOM on SDH in MU Stage 3 apply Domains • NQF on SDH Risk Adjustment domain criteria Collected existing protocols from the field • Collected 50 protocols (many not Critiera: validated) 1) Actionability • Interviewed 20 protocols 2) Alignment with National Initiatives • Identified top 5 protocols 3) Evidence in Research Engaged stakeholders for feedback 4) Burden of Data Collection 5) Sensitivity • Braintrust (advisory board) discussion • Surveyed stakeholders 6) Stakeholder Feedback • Distributed worksheet to potential users for feedback 9 PRAPARE DOMAINS Core PRAPARE asks 15 questions to assess 14 UDS SDH Domains Non-UDS SDH Domains core SDH domains. 1. Race 10. Education 2. Ethnicity 11. Employment 3. Veteran Status 12. Material Security 9 domains already asked for federal 4. Farmworker Status 13. Social Integration health center reporting (Uniform Data 5. English Proficiency 14. Stress System) so can be auto-populated 6. Income 7. Insurance 5 non-UDS domains informed by 8. Neighborhood Meaningful Use Stage 3 9. Housing Optional PRAPARE has 6 optional domains. Non-UDS SDH Domains 1. Incarceration History 5. Safety 2. Transportation 6. Domestic Violence Find the tool at : 3. Refugee Status http://www.nachc.com/research-data.cfm 4. Country of Origin 10 5
4/19/2016 CROSSWALK OF PRAPARE WITH OTHER NATIONAL INITIATIVES PRAPAR ARE Domain UDS ICD-10 10 IOM Meaningf gful HP202 020 RWJF County ty Use (2 and 3) Health th Race/Ethnicity X X X X X Farmworker Status X Veteran Status X Seeking comments English Proficiency X X X X Income X X X X X Insurance Status X X X Neighborhood X X X X X Housing X X X Education X X X X X Employment X X X X X Material Security X X X X X Social Integration X X X X X Stress X X X X VALIDATING THE TOOL Questions Selected questions Pilot Tested Performed Reviewed by to measure SDH Questions Cognitive domains Health Literacy Testing on Expert Questions • Pulled from • Revised as • To ensure existing • Each pilot site necessary after language validated performed pilot testing matched questions when cognitive common possible (few testing with at reading levels validated least 10 questions exist) patients 12 6
4/19/2016 13 14 7
4/19/2016 EXAMPLES OF NEXTGEN TEMPLATES 15 EXAMPLES OF NEXTGEN TEMPLATES 16 8
4/19/2016 WHAT IS THE STATUS OF PRAPARE? 18 9
4/19/2016 TIMELINE OF THE PROJECT • Develop PRAPARE tool Year 1 Dissemination 2014 • Pilot PRAPARE implementation Year 2 in EHR and explore data utility 2015 • PRAPARE Implementation & Year 3 Action Toolkit 2016 19 PRAPARE PILOT TESTING IMPLEMENTATION TEAMS AND ELECTRONIC HEALTH RECORDS 20 10
4/19/2016 IN DEVELOPMENT: IMPLEMENTATION AND ACTION TOOLKIT Cate tego gori ries Exa xamples s of Po Potenti tial Resources rces to to Incl clude Step 1: Understand the Project Project overview, project framework, defining risk, case studies, FAQs Step 2: Engage Key Stakeholders Messaging materials, change management guidance Readiness assessment, PDSA materials, 5 Rights Framework, Implementation Step 3: Strategize the Implementation Plan timeline, progress reports, legal documents Step 4: Technical Implementation PRAPARE paper assessment, data documentation, EHR templates, sample data dictionaries, data specifications, data warehouse and retrieval strategies, guidelines for using design and requirements documents Step 5: Workflow Implementation Workflow diagrams, data collection training curriculum, lessons learned and best practices Step 6: Understand and Report Your Data Reporting requirements, sample database, sample data outputs, sample data analyses and reports, cross-tabulating data, evaluation protocol, population- level planning, guidelines for data integration Step 7: Act on Your Data Strategy for detecting risk, report on best practices and processes for using SDH data, examples of SDH interventions, SDH response codes, linking to enabling services codes Step 8: Use Your Data to Drive Payment and Strategy to engage payers, funding SDH efforts, data visualization templates Policy Transformation 21 PRAPARE IS A NATIONAL MOVEMENT! Use and Interest in PRAPARE • Health centers in 8 states are either already using PRAPARE or are planning to begin using PRAPARE in 2016 • Health centers, state associations, regional networks, and other health care organizations in 20+ other states interested in using PRAPARE 22 11
4/19/2016 HOW CAN PRAPARE BE USED AT YOUR ORGANIZATION? 23 IMPLEMENTING PRAPARE: USING THE FIVE RIGHTS FRAMEWORK • How will tool be administered to the patient to ensure that it Right Information accurately identifies the SDH the patient may have? • Who will collect the data and who will address the social Right Person determinants identified? Right Intervention • How will resource information be organized so that it is readily Format available and standardized for all? • How is the appropriate care team member notified to address the Right Channel SDH identified? Right Time in • When in the patient visit does it make sense to administer the tool Workflow and when is the best time to address identified SDH? 24 12
Recommend
More recommend