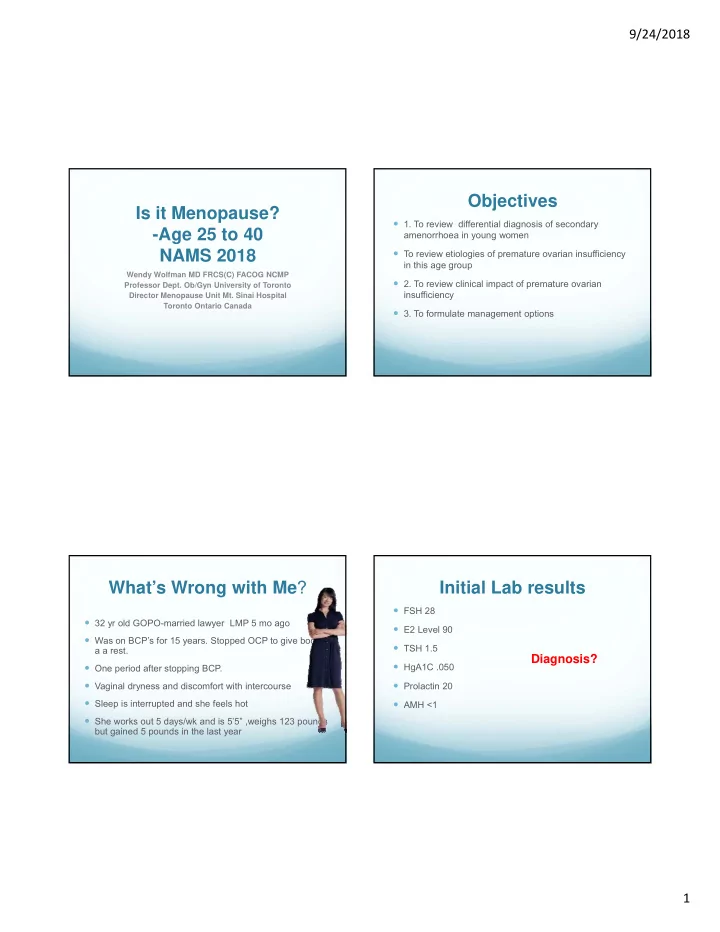
9/24/2018 Objectives Is it Menopause? 1. To review differential diagnosis of secondary -Age 25 to 40 amenorrhoea in young women NAMS 2018 To review etiologies of premature ovarian insufficiency in this age group Wendy Wolfman MD FRCS(C) FACOG NCMP 2. To review clinical impact of premature ovarian Professor Dept. Ob/Gyn University of Toronto insufficiency Director Menopause Unit Mt. Sinai Hospital Toronto Ontario Canada 3. To formulate management options What’s Wrong with Me ? Initial Lab results FSH 28 32 yr old GOPO-married lawyer LMP 5 mo ago E2 Level 90 Was on BCP’s for 15 years. Stopped OCP to give body a TSH 1.5 a a rest. Diagnosis? HgA1C .050 One period after stopping BCP. Vaginal dryness and discomfort with intercourse Prolactin 20 Sleep is interrupted and she feels hot AMH <1 She works out 5 days/wk and is 5’5” ,weighs 123 pounds but gained 5 pounds in the last year 1
9/24/2018 Definition-ESHRE Most common causes of secondary Guidelines 2016 amenorrhea in women Clinical syndrome defined by loss of ovarian activity 1. Pregnancy before 40 2. PCO- FSH-Normal-E2-Normal Characterized by amenorrhea or oligomenorrhea for at 3. Hypothalamic amenorrhoea- FSH E2 least 4 months with raised gonadotropins and low estradiol 4. POI- FSH E2 Due to decreased ovarian function primary ovarian insufficiency or premature ovarian insufficiency FSH>25 IU/ml on 2 occasions>4 wks apart Diagnosis of POI Pathogenesis 90% present with secondary amenorrhoea 20 weeks gestation-6-7 million Primordial germ cells (PGC), 1-2 million at birth, 400,000 at puberty, 500 Also known as hypergonadotropic hypogonadism ovulations in reproductive life 1% of population <40, 0.1%<30 Fertile lifespan depends on Results in hypoestrogenism and infertiility size of oocyte pool at birth 5-10% conceive rate of depletion over reproductive life Most common cause 90% unknown active destruction As cancer cure rates improve incidence will rise possibly inadequate renewal of stem cells Modifiable factors-smoking, surgical practice and modifying medical treatments for malignant and chronic diseases Nelson L, NEJM 2009 ESHRE Guidelines Hum Reprod 2016 2
9/24/2018 Why is the Correct Early Menopause Diagnosis Important Ages 40-45 Huge and serious diagnosis for a young woman 3-5% of population Prospective Fertility Clinically same risk factors for bone and CVR Long term ramifications of estrogen lack HT recommended until average age of menopause or To Improve symptoms and Quality of Life 51-52 Etiology of POI Informing Patient Idiopathic most common –up to 90% Devastating diagnosis, impairs self-esteem Iatrogenic -increasing 71% dissatisfied with how they were told Chemotherapy and radiation 50% saw > 3 clinicians surgical Genetic -10-13%-most Turner’s, in this age group mosaics then Need time and information-consider increased risk in relatives Fragile X (FMR1)- 0.8-7.5% of cases 5-10% pregnancy rate Autoimmune -5% of cases Information re long term health risks Metabolic - galactossemia Emotional support Infectious -HIV, Cytomegalovirus, Zoster, Mumps HT does not have same conjectural risks in younger women Toxins/Environmental- smoking ,organic substances Yasui JCO 2009 Qin Hum Reprod Update 2015 Hamoda Post Reproductive Health 2017 3
9/24/2018 Ramifications of POI Treatment Counselling- untreated reduced life expectancy due to CVR Symptoms Other Issues disease Vasomotor Symptoms relatives may be at increased risk-no predictive tests Cardiovascular CHF IHD Sleep disturbances Stop smoking Osteoporosis Mood changes and Hormone replacement until average age of menopause- Earlier neurological problems depression does not increase breast cancer-need P to protect uterus Dementia Joint aches Strokes Exercise and weight management Vaginal Dryness Parkinson’s Adequate calcium and vitamin D Sexual Issues-Dyspareunia, Decreased Libido Earlier death Referral to discuss fertility and egg donation if patient is Dry eyes ready What is the Best Replacement ? Conclusions Depends on patient and compliance-Individualize Suspect POI in young women with secondary amenorrhoea who are not pregnant younger patients tend to prefer OCP’s, older HT Replicate average estrogen level during menstrual cycle 382 Prevent POI by preserving ovaries at hysterectomy if pmol/L possible Prefer transdermal therapies with 100 μ gm estradiol patches Hormone therapy in young women does not have the or 2 mg estrace-Higher doses than menopausal same risks as therapy in older women 12 days sequential (300 mg P or 10 mg provera)- versus daily P- optimal daily dose for unknown with higher doses of Treat patients with hormone therapy until the average E- age of menopause Long cycle low dose OCP for contraception or LNG-IUD with estrogen Kaunitz Obste Gynecol 2015 N Am Men Society 2017 Stute P Climacteric 2016 Sassarini Cl Endo and Metab 2015 4
Recommend
More recommend