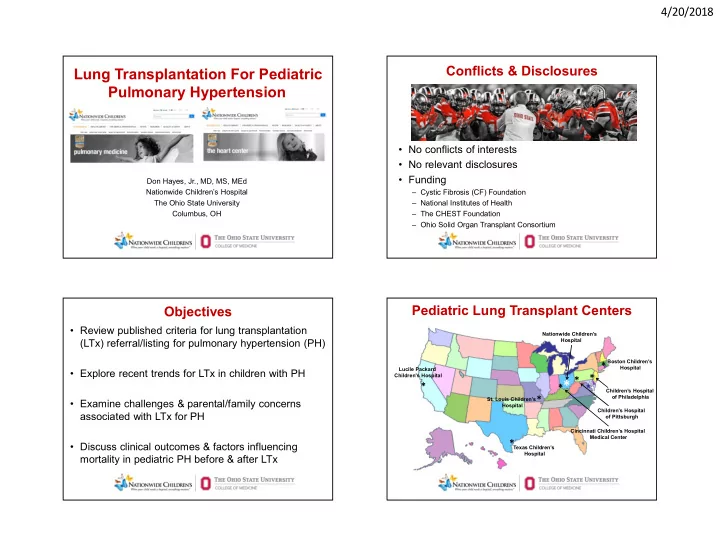
4/20/2018 Conflicts & Disclosures Lung Transplantation For Pediatric Pulmonary Hypertension • No conflicts of interests • No relevant disclosures • Funding Don Hayes, Jr., MD, MS, MEd Nationwide Children’s Hospital – Cystic Fibrosis (CF) Foundation The Ohio State University – National Institutes of Health Columbus, OH – The CHEST Foundation – Ohio Solid Organ Transplant Consortium Pediatric Lung Transplant Centers Objectives • Review published criteria for lung transplantation Nationwide Children’s (LTx) referral/listing for pulmonary hypertension (PH) Hospital Boston Children’s * Hospital Lucile Packard • Explore recent trends for LTx in children with PH Children's Hospital * * * * * Children’s Hospital of Philadelphia * St. Louis Children’s • Examine challenges & parental/family concerns Hospital Children’s Hospital associated with LTx for PH of Pittsburgh Cincinnati Children’s Hospital Medical Center * • Discuss clinical outcomes & factors influencing Texas Children’s Hospital mortality in pediatric PH before & after LTx 1
4/20/2018 Pediatric Lung Transplants Indications by Age Group (1/00- 6/16) Diagnosis < 1 1-5 6-10 11-17 Cystic Fibrosis 0 4 3.7% 116 50.0% 814 66.7% Non CF-bronchiectasis 0 0 2 0.9% 23 1.9% ILD 5 8.3% 9 8.3% 6 2.6% 37 3.0% ILD Other Specify Cause 6 10.0% 10 9.3% 21 9.1% 46 3.8% Pulmonary Hypertension/Pulmonary Arterial 7 11.7% 28 25.9% 24 10.3% 100 8.2% Hypertension PH Eisenmenger’s Syndrome 0 1 0.9% 2 0.9% 6 0.5% PHT Other 15 25.0% 21 19.4% 8 3.4% 20 1.6% Obliterative Bronchiolitis (non-Retransplant) 0 10 9.3% 26 11.2% 58 4.8% Bronchopulmonary Dysplasia 4 6.7% 4 3.7% 3 1.3% 3 0.2% ABCA3 Transporter Mutation 5 8.3% 4 3.7% 1 0.4% 1 0.1% Surfactant Protein B Deficiency 13 21.7% 4 3.7% 1 0.4% 0 Surfactant Protein C Deficiency 0 1 0.9% 0 1 0.1% Retransplant (Obliterative Bronchiolitis) 0 4 3.7% 8 3.4% 41 3.4% Retransplant (not Obliterative Bronchiolitis) 0 4 3.7% 6 2.6% 41 3.4% COPD, with or without A1ATD 2 3.3% 1 0.9% 3 1.3% 10 0.8% Other 3 5.0% 3 2.8% 5 2.2% 20 1.6% JHLT 2017; 36(10): 1037-1079 Pediatric Lung Transplants Age Distribution by Pediatric Lung Transplants Indications by Year (Number) Diagnosis (1/08-6/16) 160 CF ILD ILD Other OB (non-Retx) PHT Other PH/PAH Other <1 1-5 6-10 11-17 140 100% Number of Transplants 120 80% 100 % of Transplants 80 60% 60 40% 40 20 20% 0 0% CF ILD ILD Other OB (non-Retx) PHT Other PH/PAH Other Transplant Year JHLT 2017; 36(10): 1037-1079 JHLT 2017; 36(10): 1037-1079 2
4/20/2018 Published Criteria for LTx Referral Pediatric Lung Transplants Diagnosis Distribution by Era (1/88-6/16) • WHO Class III or IV symptoms CF ILD ILD Other OB (non-Retx) PH/PAH PHT Other Other 100% – During escalating therapy • Rapidly progressive disease 80% % of Transplants – Assuming no weight & rehabilitation concerns 60% • Use of parenteral targeted PH therapy – Regardless of symptoms or WHO Class 40% • Known or suspected 20% – Pulmonary veno-occlusive disease (PVOD) – Pulmonary capillary hemangiomatosis 0% 1988-1999 (N=634) 2000-2007 (N=679) 2008-6/2016 (N=942) Weill D et al. JHLT 2015;34:1-15 JHLT 2017; 36(10): 1037-1079 Published Criteria for LTx Listing Challenges of Pediatric PH for LTx • WHO Class III or IV • Heterogeneous population – 3 mo trial of combo therapy, including prostanoids • Effect of therapeutic options • Cardiac index < 2 L/min/m 2 – Prostanoids • Mean right atrial pressure > 15 mmHg – Endothelin receptor antagonists • 6-min walk test < 350 m • Clinical deterioration – Phosphodiesterase inhibitors – Significant hemoptysis • Wide referral/listing patterns – Pericardial effusion – Variations at respective centers – Progressive right heart failure • With rapid deterioration • Renal insufficiency • ↑ bilirubin, brain natriuretic peptide – LTx bridging strategies are an option but more • Recurrent ascites difficult Weill D et al. JHLT 2015;34:1-15 3
4/20/2018 Parental/Family Concerns Underappreciated Factors • Insight provided by parents • Far fewer & more distant LTx centers – Low success rate – Referral, evaluation, & relocation for listing is onerous – High rejection rate • Higher mortality on waitlist – High post-LTx mortality – Not a cure • Younger age donors – Potential need for another LTx – Lungs most compromised of transplantable organs – Buying time & not quality of life • Higher priority for 1A & 1B heart candidates – Poor quality of life when heart-lungs being considered • Anti-rejection meds, Prolonged care, Hospital stays – Most PH candidates listed for heart-lung are status – Other complications 2 on heart list • Diabetes, Cancer From George Mallory, MD – Heart pulls the lungs but not vice versa Prognosis of Pediatric PH Spanish Study Pediatric PH Cohort Pulmonary arterial hypertension (PAH) • Spanish Registry Study – 225 patients, 21 centers – Epidemiology/outcomes & phenotypical characterization of pediatric PH – First registry reporting moderate to severe PH in children using Nice groups II, III, IV, & V del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 4
4/20/2018 Prognosis of Pediatric PH Survival by “Nice Etiologic” Group • Mean age at diagnosis 4.3 ± 4.9 yrs – 50% < 2 yrs of age • Survival rates (whole cohort – pulmonary vascular disease) – 1-yr: 80% – 3-yr: 74% • Survival rates (PAH cohort) – 1-yr: 89% – 3-yr: 85% del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 Survival by (A) Functional Class (FC) at Mortality & Children with PH Diagnosis & (B) Age at Diagnosis • Risk factors for mortality – Etiologic group other than PAH – Age at diagnosis < 2 yrs – Advanced functional class at diagnosis – Elevated right atrial pressure at diagnosis del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 del Cerro Marín MJ et al. AJRCCM 2014;190:1421-9 5
4/20/2018 Post-Transplant Outcomes: Pediatric PH Pediatric PH Referred for LTx • Published work: cohorts of 5-23 patients 1-3 – Severely limiting the ability to predict post- transplant outcomes – 1-yr survival rates: range from 87-100% – Schaellibaum et al: 3-yr survival estimates of 84% – Goldstein et al: 5-yr survival of 61% . 1 Lammers AE et al. Pediatr Pulmonol 2010;45:263-9 2 Schaellibaum G et al. Pediatr Pulmonol 2011;46:1121-7 3 Goldstein BS et al. JHLT 2011;30:1148-52 Lammers AE et al. Pediatr Pulmonol 2010;45:263-9 UNOS Registry Analysis Pediatric PH Listed for LTx • United Network for Organ Sharing Registry – May 2005 to Dec 2015, F/U data through Dec 2016 • Analysis – Patient survival: Kaplan-Meier (KM) curves, log-rank tests, & univariate Cox proportional hazards regression • Results – 156 children < 18 yrs of age listed for LTx or HLTx for PPH • 29 died on waitlist – 65 children (26/39 boys/girls, age 10 ± 6 yrs) • 47 bilateral LTx; 18 combined heart-lung transplantation (HLTx) • Deaths after transplant – 19 in LTx cohort; 9 in HLTx cohort – KM curve: 5-year survival rates » 61% for LTx » 48% for HLTx Goldstein BS et al. JHLT 2011;30:1148-52 Unpublished Data 6
4/20/2018 KM Curve: Post-Transplant for PPH Univariate Cox Regression Age < 18 yrs compared to other indications, 5/05-12/15 1.00 Mean (SD) LTx for PPH LTx for other indications HR (95% CI) P HLTx for PPH HLTx for other indications or N (%) 0.80 Proportion surviving Age (y) 10 (6) 0.93 (0.88, 0.995) 0.036 0.60 Female 39 (60%) 1.47 (0.68, 3.21) 0.329 0.40 Calculated LAS (35 patients) 34 (4) 1.04 (0.92, 1.17) 0.555 0.20 Status 1A (18 patients) 15 (83%) 0.77 (0.20, 2.90) 0.700 0.00 Mean PAP (mmHg) (36 patients) 73 (21) 0.99 (0.97, 1.01) 0.282 0 1 2 3 4 5 6 7 8 9 10 Time after transplant (years) Unpublished Data Unpublished Data Conclusions • Children with PH should be considered for LTx • Early referral is absolutely OK! • Referral for transplantation – At diagnosis in non-PAH pulmonary vascular diseases – Poor functional class • WHO Class II with poor clinical trajectory • WHO Class III or IV – Elevated right atrial pressure • Clinical scenarios to consider referral • Hemoptysis, Declining cardiac function • Escalating therapy, Need for parenteral therapy • No reduction in PVRI with vasodilator testing • PVOD, pulmonary capillary hemangiomatosis, alveolar capillary dysplasia with misalignment of pulmonary veins 7
Recommend
More recommend