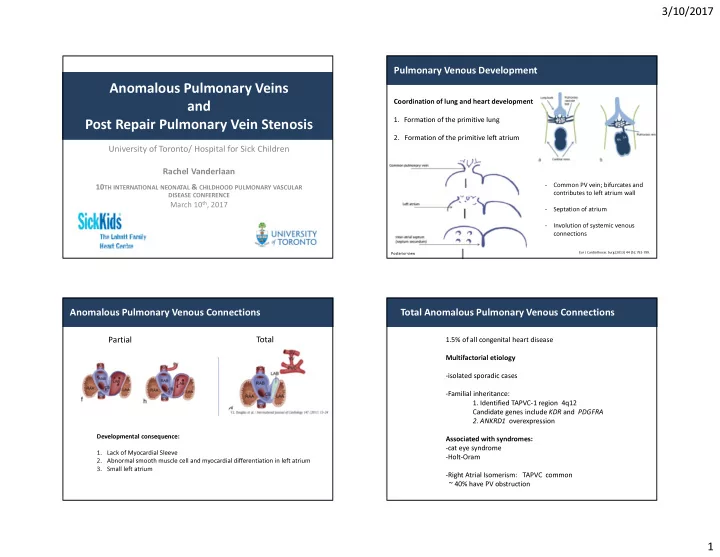
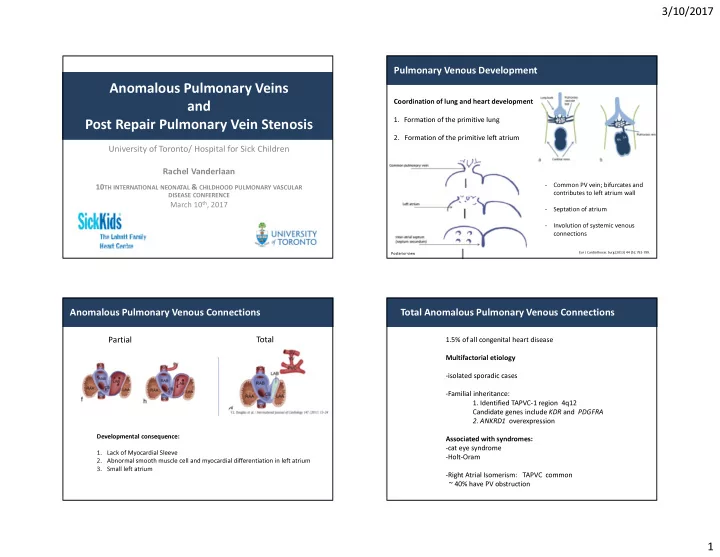
3/10/2017 Pulmonary Venous Development Anomalous Pulmonary Veins Coordination of lung and heart development and 1. Formation of the primitive lung Post Repair Pulmonary Vein Stenosis 2. Formation of the primitive left atrium University of Toronto/ Hospital for Sick Children Rachel Vanderlaan - Common PV vein; bifurcates and 10 TH INTERNATIONAL NEONATAL & CHILDHOOD PULMONARY VASCULAR contributes to left atrium wall DISEASE CONFERENCE March 10 th , 2017 - Septation of atrium - Involution of systemic venous connections Eur J Cardiothorac Surg (2013) 44 (5): 792-799. Posterior view Anomalous Pulmonary Venous Connections Total Anomalous Pulmonary Venous Connections Total Partial 1.5% of all congenital heart disease Multifactorial etiology -isolated sporadic cases -Familial inheritance: 1. Identified TAPVC-1 region 4q12 Candidate genes include KDR and PDGFRA 2. ANKRD1 overexpression Developmental consequence: Associated with syndromes: -cat eye syndrome 1. Lack of Myocardial Sleeve -Holt-Oram 2. Abnormal smooth muscle cell and myocardial differentiation in left atrium 3. Small left atrium -Right Atrial Isomerism: TAPVC common ~ 40% have PV obstruction 1
3/10/2017 Types of TAPVC TAPVC : Clinical presentation Supracardiac ; Type I ~45% Cardiac ; Type II ~25% 1. Degree of obstruction to pulmonary venous drainage Innominate vein Coronary Sinus 2. Degree of restriction to the compensatory right-to-left shunt (right cardinal veins) (left cardinal veins) Neonate- unobstructed Neonate- obstructed Spectrum Infracardiac/Mixed Supracardiac/Cardiac Infracardiac ; Type III ~25% Symptoms of RV Mixed ; Type IV ~5% Pulm edema, hypoxemia, volume overload cardiogenic shock Hepatic vein / IVC ( umbilicovitelline ) Definitive Management: Surgery Kirlin Cardiac Surgery TAPVC : Risk Factors and Outcomes TAPVC : Risk Factors and Outcomes Post Repair Pulmonary Vein Stenosis Intervention for post-repair PVS PVS after TAPV repair Cardiac and Supracardiac (1998-2004) Risk Factors - Preoperative PVO Infracardiac and Mixed - 40% of patients - associated with infracardiac - Younger age at presentation - Postoperative PVS Recurrence common Occurs in ~10-15% High mortality Risk factor for death Seale AN, JTCVS 2013 Significant Morbidity: recurrent infections, hemoptysis, pneumonectomy Shi G, 2017 2
3/10/2017 Bringing PVS into Focus Bringing PVS into Focus : PVS Team PVS Team Post repair PVS: High mortality and morbidity -Cardiologists- Echo, MRI, PH, interventionalist , CCCU and surgeons -Adjunct teams: Lung Transplant, PACT 1. Interventions Clinical Surveillance Protocol- ‘Standard of Care’ Echo -Surgery - Patients with congenital or post repair PVS -Catheter based interventions - Children with RAI- small PV confluence (Cath) CT/MRI -Transplant - GOAL: Early detection, Early intervention - Complementary use of multiple imaging modalities 2. Medical Therapies/ Experimental therapies 3. Enhanced Surveillance- Echo + CTA/MRA/Cath Basic CSP: 1, 6, 12 months post intervention 4. Team/ Collaborative Approach Echo , CTA/MRA (cath) Patient specific: Match surveillance to velocity of disease 5. Research: Understanding mechanisms of disease Clinical Impact of PVS Team Pre–CSP cohort Post-CSP cohort Surgical repair of PVS (2010- sept 2015) (Sept 2015-Sept 2016) Number of Patients n=30 n=9 Number of patients with 3D 21/30 (70%) 9/9 ( 100%) * imaging for diagnosis Time from 3D imaging to surgery 50 days (22-109) 16 days ( 9-40) (median , IQR) Number of patients with 3D 9/16 ( 56%) 9/9 (100%) * imaging for follow up ( 16 patients with f/u data) Time from surgery to 3D imaging 131 days (91-219) 52 days (42-62)* (median , IQR) Improved performance and surveillance Growth in knowledge of PVS Disease Stabilization/Cure Transplantation Palliation Maturation of team 3
3/10/2017 Collaboration: PVS Network Collaboration: PVS Network Advancing Research and Clinical Care Absence of Clinical Guidelines for Children with Pulmonary Vein Stenosis Heterogeneous Presentation Regional/ Diverse Over 12 Institutions and growing Institutional Individual North Imaging PVS Clinician Practices American Modalities practices 1. Registry study practices Multiple PVS Team PVS Network First analysis: clinical practice patterns and contemporary Treatment outcomes Options Practice Based Evidence Evidence based Practice 2. Resources: parents and clinicians www.pvsnetwork.org 3. Generation of consensus guidelines Collaboration to improve outcomes for children with PVS Pig Surgical Model: Disease Mechanisms in PVS Laboratory Model of PVS Bringing PVS into focus: Understanding Disease Mechanisms 3 wk 5 wk 7 wk PVS Research Sequential Sacrifice bilateral PV Genomics Molecular mechanism banding losartan LB7 Therapies SHAM B3 Clinical Trial RV weight- PA systolic indexed pressure 50 * 100 * mmHg 40 PVS Team Surveillance B7 30 B5 50 20 10 0 0 Sham B7 Sham B7 Modified model from LaBourene, Circ Res 1990; Kato et al. JTCVS 2012 4
3/10/2017 Progressive Disease: Myofibroblast Deposition Progressive Disease: Myofibroblast Deposition SHAM Stage 1 Stage 2 Stage 3 7 * α-SMA/CD31 6 mRNA expression Fold Increase in * * 5 S B3 B5 B7 * 4 * * MMP2 1. Proliferating Cells 3 Fibronectin Col1A1 2 -Fibroblasts, SMC Gapdh 1 0 2. Endothelial to mesenchymal transition B3 B5 B7 3. Circulating Progenitors Endothelial to mesenchymal transition : source of myofibroblasts Proliferation contributes to neointimal lesions FN/DAPI/VE PV Endothelial cells Mechanical Growth Stress TGF-B factors Veh 5 mRNA expression TGFB Ki 67 Fold Increase in * SNAIL mRNA expression 4 Fold Increase in 2 * * * Veh EndMT * 3 1.5 * FN/DAPI/VE CD31 α-SMA, FSP-1 2 1 * VE Cadherin FN 1 0.5 EC markers Fibroblast 0 0 markers Sham B5 TGFB B3 B5 B7 MET % Ki-67 positive cells 8 Intima Media Adventitia Sham * 7 mRNA expression 15 Fold Increase in p=0.06 * 10 15 * 6 * * * 8 Snail 10 5 * * 10 * 6 Twist 4 4 α-SMA\CD31 5 5 3 2 2 0 0 B5 0 1 Sham B3 B5 B7 Sham B3 B5 B7 Sham B3 B5 B7 0 B3 B5 B7 Enhanced proliferation in the intimal and adventitial compartments Supportive of EndMT in PVS neointimal formation 5
3/10/2017 Altered vasoreactivity in upstream pulm veins Therapeutic Adjuncts in PVS Losartan ↑TGF B and AngII signaling Acetylcholine 20 Adventitial fibroblast Fold Increase in mRNA Protein * 0 * Carbonylation proliferation and 7 Nox 2 Nox4 p22phox p47phox EndMT * -20 activation 6 * Sham B7 expression * % Relaxation -40 5 0.06 * * * * -60 4 Anti- DNP -80 Myofibroblasts 3 * * Banded -100 ECM deposition 2 -120 1 Sham Losartan + Sham Banded 0 -140 Banded B- 10 -9 10 -8 10 -7 10 -6 10 -5 10 -4 B3 B5 B7 actin Early upstream endothelial dysfunction prior to overt neointimal lesions Zhu J et al. JTCVS 2014 -> Health Canada Safety and Feasibility Trial Summary Acknowledgements PVS Research Program PVS team PVS Network Post repair PVS has significant impact on survival following Christopher Caldarone Christopher Caldarone Site investigators and TAPVC primary repair Rachel Vanderlaan Andreea Dragulescu research coordinators Lars Grosse-Wortmann Post repair PVS and congenital PVS : Many Tools Members/ Trainees Tilman Humpl Donor Families Anouk Martine-Teichert Hartmut Grasemann -requires team approach and sharing of knowledge Yana Fu Jennifer Russell -multi-institutional collaboration key for progress Yanting Wang Luc Mertens Mauro Lo Rito Andrea Wan Haruki Ide Rachel Vanderlaan Research will insights into disease mechanisms Jiaquan Zhu -Identification of targets for developing therapeutic adjuncts Hideyuki Kato Collaborators John Coles Jason Maynes Richard Wiesel Jaques Belik Boris Hinz 6
3/10/2017 Post Repair PVS - Histological neointimal lesions similar to primary PVS Diffuse NeoIntimal lesions and fibrosis - Can be progressive into upstream intraparenchymal veins - Unilateral / bilateral 7
Recommend
More recommend