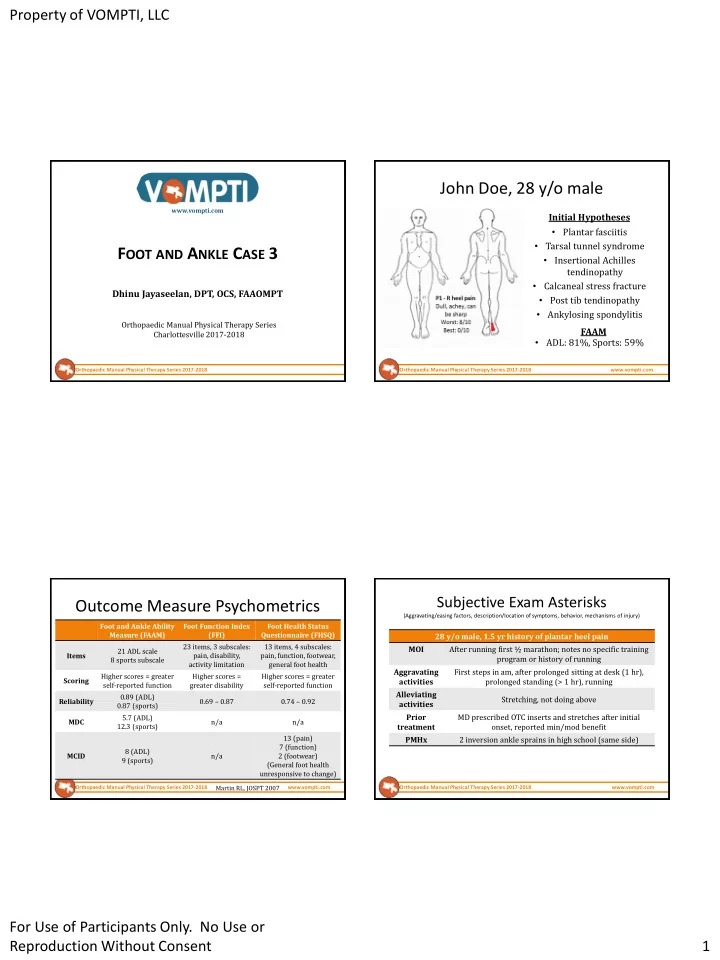
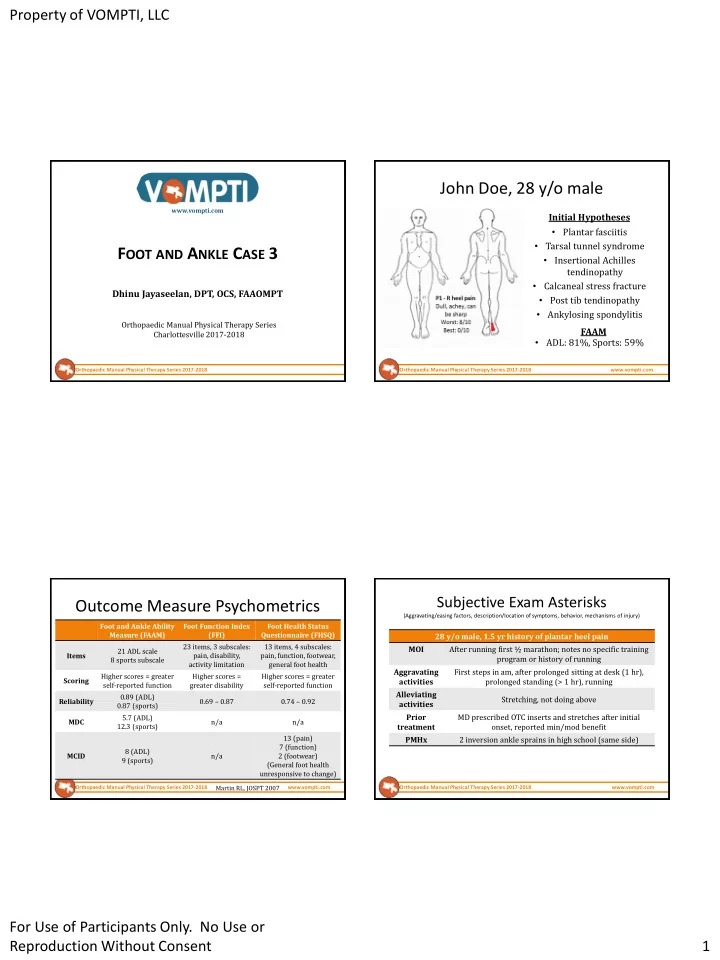
Property of VOMPTI, LLC John Doe, 28 y/o male www.vompti.com Initial Hypotheses • Plantar fasciitis • Tarsal tunnel syndrome F OOT AND A NKLE C ASE 3 • Insertional Achilles tendinopathy • Calcaneal stress fracture Dhinu Jayaseelan, DPT, OCS, FAAOMPT • Post tib tendinopathy • Ankylosing spondylitis Orthopaedic Manual Physical Therapy Series FAAM Charlottesville 2017-2018 • ADL: 81%, Sports: 59% Orthopaedic Manual Physical Therapy Series 2017-2018 Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Subjective Exam Asterisks Outcome Measure Psychometrics (Aggravating/easing factors, description/location of symptoms, behavior, mechanisms of injury) Foot and Ankle Ability Foot Function Index Foot Health Status Measure (FAAM) (FFI) Questionnaire (FHSQ) 28 y/o male, 1.5 yr history of plantar heel pain 23 items, 3 subscales: 13 items, 4 subscales: MOI After running first ½ marathon; notes no specific training 21 ADL scale Items pain, disability, pain, function, footwear, program or history of running 8 sports subscale activity limitation general foot health Aggravating First steps in am, after prolonged sitting at desk (1 hr), Higher scores = greater Higher scores = Higher scores = greater Scoring activities prolonged standing (> 1 hr), running self-reported function greater disability self-reported function Alleviating 0.89 (ADL) Stretching, not doing above Reliability 0.69 – 0.87 0.74 – 0.92 activities 0.87 (sports) 5.7 (ADL) Prior MD prescribed OTC inserts and stretches after initial MDC n/a n/a 12.3 (sports) treatment onset, reported min/mod benefit 13 (pain) PMHx 2 inversion ankle sprains in high school (same side) 7 (function) 8 (ADL) MCID n/a 2 (footwear) 9 (sports) (General foot health unresponsive to change) Martin RL, JOSPT 2007 Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com For Use of Participants Only. No Use or Reproduction Without Consent 1
Property of VOMPTI, LLC Physical Exam Asterisks Structure(s) at fault (Special tests, movement/joint dysfunction, posture, palpation, etc) Myofascial Non-contractile Other Joints in/refer Neural tissue 28 y/o male, 1.5 yr history of plantar heel pain tissue in/refer tissue in/refer structures to to painful in/refer to to painful to painful be examined Posture Pes cavus bilaterally region painful region region region (non-MSK) Decr DF (worse with knee straight) and ROM pronation Talocrural Plantar fascia Subtalar Achilles tendon Single leg heel raises L: 26 reps; R: 15 reps* Fat pad Distal tib-fib Post tib tendon Tibial n. (medial Calcaneal fx? Retrocalcaneal Special tests (+) windlass test, (-) SLR/slump, Tinel’s Talonavicular FHL, FDL calcaneal/plantar) Ankylosing bursa Calcaneocuboid Trigger point L5,S1 spondylitis? Stability tests (-) Deltoid, spring TMT joints referral ligaments TTP (+) R medial calcaneal tubercle and proximal Hip, SIJ, L-spine Palpation ½ plantar fascia (thickness also noted)* • Primary hypothesis after subjective: chronic plantar fasciitis Joint accessory Hypomobile R TCJ AP, STJ medial glide, midfoot throughout, 1 st MTP AP and PA glides Differential (rank order): tarsal tunnel, post tib tendinopathy, • motion insertional AT, myofascial pain syndrome, lumbar radic Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Rate your assessment of severity/irritability • Are the relationships between the areas on the body chart, the interview, and physical exam consistent? Justify your assessment with examples from the subjective and/or objective exam “Do the features fit” a recognizable clinical pattern? If Severity: None Min Mod Max • YES, what? – Impacts ability to run or WB for durations, not disabling in functional tasks Min • Irritability: None Mod Max Chronic plantar fasciitis – Symptoms brought on with prolonged activity reduced fairly rapidly (plantar fasciosis, plantar fasciopathy) Stage and stability? • Identify any potential risk factors (yellow, red flags, non-MSK involvement, biopsychosocial) Chronic • Acute Subacute Acute on chronic – 1.5 yr history, no recent mechanism or indicators of inflammatory processes Frustration with lack of improvement? • Stable Improving Worsening Fluctuating Red flags? – Symptoms generally the same, not better or worse, appears mechanical/MSK Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com For Use of Participants Only. No Use or Reproduction Without Consent 2
Property of VOMPTI, LLC Recommendations based on evidence published before Jan 2013 Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Plantar Fasciitis Plantar Fasciitis • Background/Demographics • Subjective Report – Most common foot condition treated in health care, up to – Pain in plantar aspect of heel 2 million Americans / year – Worse with initial steps after prolonged inactivity or – Affects athletic and non-athletic populations prolonged weight bearing – Mean symptom duration: 13.3 – 14.1 months – Precipitated by recent increase in WB activity • Risk Factors: • Objective Examination – Limited ankle DF ROM (Odds Ratio: 23.3) – Tenderness at plantar fascia (medial calcaneal tubercle) – High BMI in non-athletic patients (OR: 5.6) – (+) Windlass test – Work-related WB activities (OR: 3.6) – (-) Tarsal tunnel/neurodynamic tests – Decr A/PROM ankle DF; 1 st ray extension mobility – Running JBJS 2003 Riddle – Cavus foot, high arch JOSPT 2014 CPG JOSPT 2014 CPG Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com For Use of Participants Only. No Use or Reproduction Without Consent 3
Property of VOMPTI, LLC Treatment Planning Additional Considerations Impairments Functional Limitations Goals • Patients with chronic PF • Imaging not typically Pain demonstrate the following: necessary, unless ruling Inability to run Normalize joint mobility Foot/ankle hypomobility out other conditions Limited standing No walking or running (Fernandez-Lao, et al. 2016) Decr gastroc length – Widespread and bilateral tolerance gait deviations Plantarflexion weakness Pain free return to run hypersensitivity Altered gait – Lower Q of L – Increased thickness of the plantar fascia in the • What is your primary objective after intial eval? affected foot (+ correlation – Education: anatomy, pathology, prognosis to symptoms Mahowald S 2011 ) – Manual therapy: calf/PF STM, rearfoot mobilizations gr III-IV – Increased fascial – Exercise prescription: self-stretching, neuro re-ed (load vascularity (+ correlation dispersion, facilitate mid/medial foot loading) to symptoms Chen H 2013 ) Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Anatomy / Pathophysiology • 3 dense bands of connective tissue • O: medial calcaneal tubercle • I: fans distally into base of proximal phalanx • Usually chronic/degenerative process related to repetitive microtrauma • Histologic analysis: marked thickening/fibrosis of PF, collagen necrosis, chondroid metaplasia, calcification Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com Orthopaedic Manual Physical Therapy Series 2017-2018 www.vompti.com For Use of Participants Only. No Use or Reproduction Without Consent 4
Recommend
More recommend