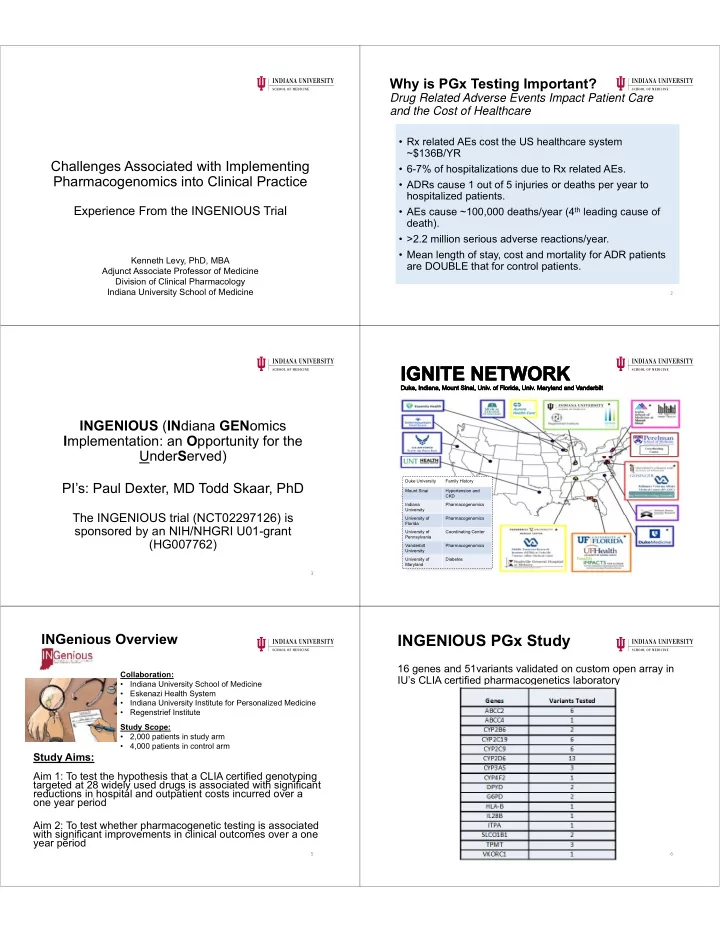
Why is PGx Testing Important? Drug Related Adverse Events Impact Patient Care and the Cost of Healthcare • Rx related AEs cost the US healthcare system ~$136B/YR Challenges Associated with Implementing • 6-7% of hospitalizations due to Rx related AEs. Pharmacogenomics into Clinical Practice • ADRs cause 1 out of 5 injuries or deaths per year to hospitalized patients. • AEs cause ~100,000 deaths/year (4 th leading cause of Experience From the INGENIOUS Trial death). • >2.2 million serious adverse reactions/year. • Mean length of stay, cost and mortality for ADR patients Kenneth Levy, PhD, MBA are DOUBLE that for control patients. Adjunct Associate Professor of Medicine Division of Clinical Pharmacology Indiana University School of Medicine 2 INGENIOUS ( IN diana GEN omics I mplementation: an O pportunity for the Under S erved) Duke University Family History PI’s: Paul Dexter, MD Todd Skaar, PhD Mount Sinai Hypertension and CKD Indiana Pharmacogenomics University The INGENIOUS trial (NCT02297126) is University of Pharmacogenomics Florida sponsored by an NIH/NHGRI U01-grant University of Coordinating Center Pennsylvania (HG007762) Vanderbilt Pharmacogenomics University University of Diabetes Maryland 3 INGenious Overview INGENIOUS PGx Study 16 genes and 51variants validated on custom open array in Collaboration: IU’s CLIA certified pharmacogenetics laboratory • Indiana University School of Medicine • Eskenazi Health System • Indiana University Institute for Personalized Medicine • Regenstrief Institute Study Scope: • 2,000 patients in study arm • 4,000 patients in control arm Study Aims: Aim 1: To test the hypothesis that a CLIA certified genotyping targeted at 28 widely used drugs is associated with significant reductions in hospital and outpatient costs incurred over a one year period Aim 2: To test whether pharmacogenetic testing is associated with significant improvements in clinical outcomes over a one year period 5 6
INGENIOUS Work Flow INGENIOUS PGx 27 Targeted Drug List Patient • Amitryptyline • Escitalopram • Simvastatin Consented • Aripiprazole • Esomeprazole • Tacrolimus Yes • Atomoxetine • 5-Fluorouracil • Thioguanine Blood Draw/Saliva • Azathioprine • Lansoprazole • Tramadol Sample Transported to PGx Remaining Sample to IU • Capcitabine • Mercaptopurine • Venlafaxine Biobank Lab • Citalopram • Nortriptyline • Voriconazole Sample Analyzed and • Clopidogrel • Omeprazole • Warfarin Results into EMR/CDS • Codeine • Pantoprazole • Doxepin • Phenytoin PGx Reports and Clinical PGx Consult if requested Alerts in EMR • Efavirenz • Rasburicase 7 7 PGx EMR Alerts INGENIOUS PGx Report Created by Clinical Decision Support Rules Page 1 Pharmacogenomic Alert! This patient has pharmacogenomic information that may impact this prescription Medication: Clopidogrel Gene(s) involved: CYP2C19 Pharma Phenotype: Poor Metabolizer Recommendation: Consider an alternative antiplatelet therapy, e.g. prasugrel, or ticagrelor. This patient’s poor metabolizer status predicts poor clopidogrel efficacy. Level of Evidence: Strong* * Clinical Pharmacogenetics Implementation Consortium (CPIC) CPIC guidelines reflect expert consensus based on clinical evidence and peer‐reviewed literature available at the time they are written and are intended only to assist clinicians in decision making Click for PGx Report Click for PGx Report Click for PM Consult Click for PM Consult 9 10 INGENIOUS PGx Report INGENIOUS PGx Report Page 2 Page 3 (CLIA Requirements) Genotype/Phenotype Results Variants Tested 11 12
INGENIOUS Consult Workflow The Tug-of-War All results for Technology Adoption and Changes to Standards of PGx lab Full PGx panel sent to EMR (G3) Care Abnormal results PGx lab forwards abnormal results to Adjudication All CPIC variants Abnormal genotype data (based on CPIC) Committee. INGENIOUS entered into G3 problem list via MD Fellow co-Investigator and Fellow (manually Phase I/ IT in phase 2 and 3) pulls medication list from EMR and presents to Consult Committee Actionable variants Phone Consult with Written consult and drug current Clinical request through U01 Pharmacologists consult committee Contact PCP or enrolling physician and ask if consult is desired/Add note to EHR Inpatient consult Outpatient consult with Clinical scheduled at MDC Pharmacologist through IUH Researchers, Educators and Clinicians Payers, Administrators and Regulators 13 14 Key Challenges to PGx Adoption How to Address the Challenges It Starts with Stakeholder Alignment As identified by IGNITE Common Measures Working Group Analysis • Senior Executive leadership (CEO/President, • Lack of reimbursement for many genomic tests CMO, CFO, Chief Legal Officer and CIO) • Few FDA approved or cleared PGx tests • Senior Clinical leadership (clinical divisions, • Lack of Provider knowledge and Education nursing and pharmacy) • Lack of Patient understanding and Education • Pathology services • EMR systems lacking PGx results entry or reporting • CDS systems do not support PGx decision making • Clinical staff and reporting • P&T committee 1 • Lack of clinical data supporting benefits of PGx • Third party payers • Clinician concerns on liability associated with genomic Incidentalomes • Patient advocates (community awareness) • Concerns regarding FDA LDT enforcement 1 ASHP Guidelines on the Pharmacy and Therapeutics Committee and the Formulary System 15 16 Implementation Team Structure Genomic Implementation Many Healthcare Systems Don’t Practice Good Implementation Requires Integrations with the Electronic Medical Record and Science Clinical Decision and Support Systems EMR is the key to a successful program • Short-term solution Driven by Informatics Committee Functional specifications require input from stakeholders Lead time – planning, coding, implementing and testing Prioritization (internal and vendor) and funding Data input and data mining critical User defined flexibility (change friendly) • Long-term Solution EMR systems programming to address genomic medicine Development of standardized CDS algorithms for genomics 17 18
Staff Education Patient Education It takes time to change clinical practice Demystify genetics Clinical Training: Supporting Patient Ownership: • Critical for short and long-term sustainability • Alignment of patient education tools and • Physician, Nursing and Pharmacy teams how to deliver (clinical teams) • Pre and post-implementation survey (what went well and what can be improved) • Patient education tools must simplify the • Training and re-training (consider turnover) concept of pharmacogenomics • CME/CE (Industry support?) • Educated patients are associated with • Adoption of Clinical Pharmacology into Medical better outcomes 1 School curriculum 1 Risk Manag Healthc Policy. 2010;3:61‐72. doi: 10.2147/RMHP.S7500. Epub 2010 Oct 14 19 20 Sustainability Changing the Standards of Care In the end, sustainability may boil down to cost justification Measuring cost effectiveness a challenging task Establishing the medical evidence Hard versus Soft Costs: • Out of pocket costs (capital and variable costs are straight forward measures Defining Establishing Creating • Ability to capture and quantify Adverse Events • Compare your adverse event rates (prevalence) to national averages Medical intended Evidence based Spreading the use Medicine message • Benchmark costs per Adverse Event • Analyze accuracy of adverse event recording • Quantifying soft costs takes time (must plan for it) 22 21 Technology Adoption Takes Time National Practice Guidelines Studies providing evidence for improved patient outcomes drive publications Define Standard of Care and fuel educational programs Effectiveness of Pharmacogenomics must be supported by Evidence Based Adoption Medicine. Guidelines define requirements and make recommendation for their Late Adopters usefulness in clinical practice Standard of Care Followers Standard Time for Adoption 10 Years Quality Measures National • What are Early criteria? Practice Adopters • Performance Guidelines measurement Thought and reporting • Do we see Publication of Leaders effect of Trial Results procedure? • How certain are • Efficacy & Safety that effect is Time • Improved HE real? Standard Timeframe 10 Years 23 24
Are We There Yet? Clinical Pharmacogenomics Conclusions: • Pharmacogenomic medicine is a powerful tool to inform drug selection and clinical decision-making • Demonstrated potential to improve efficacy and safety of medications • As more clinical data emerges and genotyping costs fall, there will be increasing utilization and presence in clinical medicine • Changes in standards of care take time Not Quite, we must continue to align academic research and the IVD industry to expedite adoption of new technology 26 25 Questions? 27
Recommend
More recommend