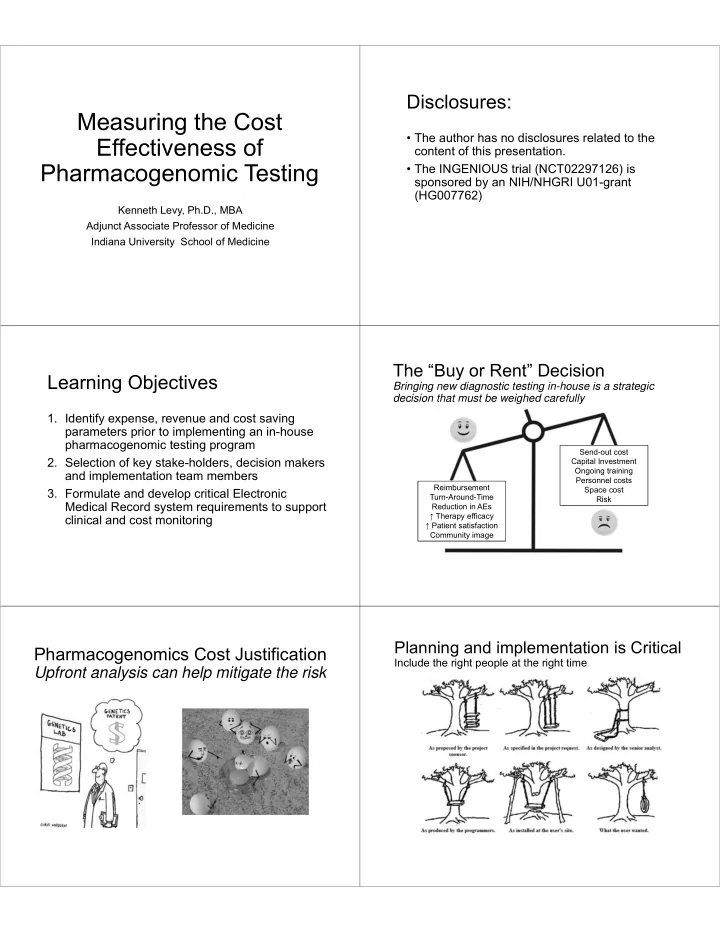
Disclosures: Measuring the Cost • The author has no disclosures related to the Effectiveness of content of this presentation. Pharmacogenomic Testing • The INGENIOUS trial (NCT02297126) is sponsored by an NIH/NHGRI U01-grant (HG007762) Kenneth Levy, Ph.D., MBA Adjunct Associate Professor of Medicine Indiana University School of Medicine The “Buy or Rent” Decision Learning Objectives Bringing new diagnostic testing in-house is a strategic decision that must be weighed carefully 1. Identify expense, revenue and cost saving parameters prior to implementing an in-house pharmacogenomic testing program Send-out cost 2. Selection of key stake-holders, decision makers Capital Investment Ongoing training and implementation team members Personnel costs Reimbursement Space cost 3. Formulate and develop critical Electronic Turn-Around-Time Risk Medical Record system requirements to support Reduction in AEs ↑ Therapy efficacy clinical and cost monitoring ↑ Patient satisfaction Community image Planning and implementation is Critical Pharmacogenomics Cost Justification Include the right people at the right time Upfront analysis can help mitigate the risk
Project Planning Cost Effectiveness and Sustainability Understanding current and future processes Keys to a successful program Graphic example only • Detailed pre-planning (with timelines and • Identifies gaps and management tools) risks • Experienced project manager • Confirms sources of costs • Alignment with key stakeholder’s needs • Staff training and clinical education • Validates workflow • Full integration (input and output) with the • Builds cross-functional Electronic Medical Records system alignment • Patient and community education Project Planning and Workflow Stakeholder Alignment • Transitions workflow into tasks • Senior Executive leadership (CEO/President, • Creates dependency relationships between tasks CMO, CFO, Chief Legal Officer and CIO) • Helps to prevent surprises and keep project on-schedule and on-budget • Senior Clinical leadership (clinical divisions, nursing and pharmacy) • Pathology services • Clinical staff • P&T committee 1 • Third party payers Graphic example only • Patient advocates (community awareness) 1 ASHP Guidelines on the Pharmacy and Therapeutics Committee and the Formulary System Key Drivers by Stakeholder Key Drivers by Stakeholder Senior Clinical leadership (clinical divisions, nursing and pharmacy) Senior Executive leadership (CEO/President, CMO, CFO, Chief Legal Officer and CIO) • Technology adoption (National standards of • Impact on clinical outcomes care) • Capital budget • Impact on malpractice liability • Headcount requirements • Education and training (staff turnover) • Standards of Care and legal liability • Impact on department headcount • Impact on community relations/Patient advocacy groups • Added time and work burden for clinical staff • Clinical relevance for each clinical specialty • Health Economics, return on overall investment • Added time and work burden for clinical staff (reimbursement vs cost) • Alignment with current workflow • Integration into LIS/HIS (time and cost)
Key Drivers by Stakeholder Key Drivers by Stakeholder Clinical Staff (physicians, nurses and clinical pharmacists) Third party payers • Clinical validation (Peer-reviewed articles, National Standards) • Clinical validation (National Standards) • Clinical Pharmacy consultation availability • CMS/other third-party adoption (CPT • Liability (to act or not act) MoPath code/tier assignment and • Education (impact on current clinical decision making) reimbursement direction) • Alignment with current workflow • Demonstrated/documented clinical and • Test turn-around time economic data addressing investment • Test reporting format versus cost prevention (short and long- • Patient education support term plus hard and soft costs) Implementation Team Structure Key Drivers by Stakeholder Patient advocates • Alignment community needs • Impact on patient care • Cost (out of pocket) to patients • Patient/community education programs Testing Choices Test Selection – Where to Start Key Questions/Decisions: • Identify institution’s most common adverse • Will third party payers reimburse for PGx events associated with gene mediated drug tests not directly linked to an ICD-9 code metabolism (informatics committee) (i.e panel testing)? • Quantify frequency (12 to 24 months) of selected adverse events within your patient population • Prospective (prevention) vs. reactive (at- (informatics committee) risk) testing (short vs. long-term impact) • Obtain institutions drug volume (in and out- • Individual tests versus disease or patient) for selected medications (informatics medication oriented PGx panels committee and pharmacy benefit manager) • Turnaround time (TAT). What is needed vs • Quantify internal costs (at the patient level) required? Cost impact linked to changes in associated with each adverse event identified TAT
Drug Gene Selection Process Pharmacogenomics Laboratory Nominate Input : Team members : Technology my be the least challenging aspect drug-gene pair Peer-reviewed publications FDA labels Pharmacogeneticist Clinical Pharmacologist • Driven by laboratory services committee Internal data prepublication Pharmacists Guidelines: CLIA lab director • Space and staff requirements CPIC Physicians (representing) Dutch PGx working group Recommendations Nephrologist Canadian (CPNDS) • Test selection and volume may direct choices Cardiologist Gastroenterologist (automated vs. manual) Infectious Disease Oncologist • Equipment acquisition (buy versus lease) Pediatrician Obstetrician Reports and Develop clinical Geriatrician • Plan for future expansion consultation action flowcharts services • Plan for obsolescence Electronic Medical Records Staff Education EMR is the key to a successful program It takes time to change clinical practice • Driven by Informatics Committee Clinical Training: • Functional specifications require input from • Critical for short and long-term sustainability stakeholders • Physician, Nursing and Pharmacy teams • Lead time – planning, coding, implementing • Pre and post-implementation survey (what and testing went well and what can be improved) • Prioritization (internal and vendor) • Training and re-training (consider turnover) • Data input and data mining critical • CME/CE • User defined flexibility (change friendly) Measuring Cost Effectiveness Patient Education A challenging task Demystify genetics Hard versus Soft Costs: Supporting Patient Ownership: • Out of pocket costs (capital and variable • Alignment of patient education tools and costs are straight forward measures how to deliver (clinical teams) • Compare your adverse event rates to • Patient education tools must simplify the national averages concept of pharmacogenomics • Benchmark costs per adverse event • Educated patients are associated with • Analyze accuracy of adverse event recording better outcomes 1 • Quantifying soft costs takes time (plan for it) 1 Risk Manag Healthc Policy. 2010;3:61-72. doi: 10.2147/RMHP.S7500. Epub 2010 Oct 14
And Finally the Money Summary Profit and Loss Analysis • Adopting in-house pharmacogenomic testing Graphic example only requires clinical and financial strategic • Justification for Laboratory • Justification for Laboratory commitments • Driven by finance committee • Driven by finance committee • Project teams require engagement from • Establish metrics to achieve and • Establish metrics to achieve and measure periodically measure periodically cross-functional areas within the institution • Cash flow, break-even analysis • Cash flow, break-even analysis • EMR integration is critical for reporting and and Net present Value (NPV) and Net present Value (NPV) data mining • Operating Profit (OP) before tax • Operating Profit (OP) before tax and depreciation and depreciation • Education of clinical staff and patients is • Cumulative Income minimum of 5 • Cumulative Income minimum of 5 required for sustainability years years
Recommend
More recommend