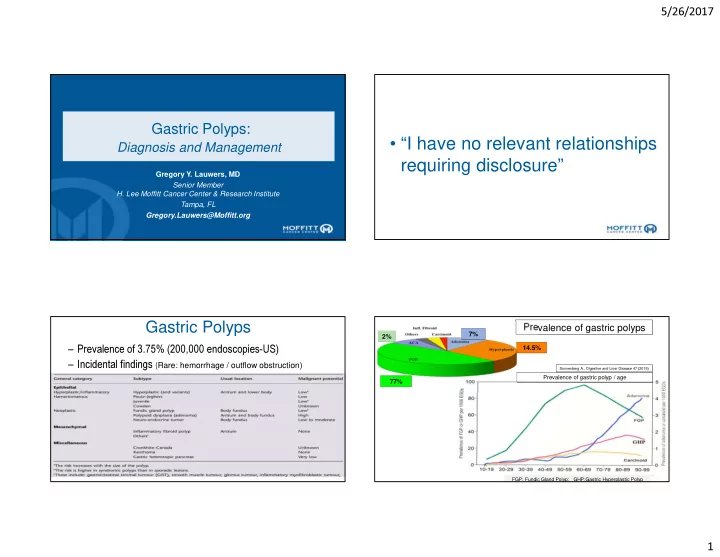
5/26/2017 Gastric Polyps: • “I have no relevant relationships Diagnosis and Management requiring disclosure” Gregory Y. Lauwers, MD Senior Member H. Lee Moffitt Cancer Center & Research Institute Tampa, FL Gregory.Lauwers@Moffitt.org Gastric Polyps Prevalence of gastric polyps 7% 2% 14.5% – Prevalence of 3.75% (200,000 endoscopies-US) – Incidental findings ( Rare: hemorrhage / outflow obstruction) Sonnenberg A., Digestive and Liver Disease 47 (2015) Prevalence of gastric polyp / age 77% FGP: Fundic Gland Polyp; GHP:Gastric Hyperplastic Polyp 1
5/26/2017 Fundic Gland Polyps • Oxyntic mucosa • Sessile: 1-5 mm • Multiple (40-60%) • Over time 40-50% are labile • Sporadic (0.09 to 5% of endoscoped pts; Female +). • FAP • Proton pump inhibitors • GAPPS ( Gastric Adenocarcinoma and Proximal Polyposis ) Sonnenberg A., Digestive and Liver Disease 47 (2015) • FAP: inactivating APC / chr 5q allelic loss • Sporadic: activating β catenin mutation (60%-90%) 2
5/26/2017 Sporadic FGP: Evolution of dysplastic FGP in FAP Dysplasia is rare (1-6%) Syndromic patients (FAP): Arnason T. Histopathology 2014, • [mean follow-up of 6 years]. 25-48% (LGD>HGD [0-12%]) – 33% “ regressed ” (n=8) Only 4 cases of ACA – 54% stable “persisted” (n=13) – 13% “progressed” to HGD/IMC (n=3) (sporadic GED progression rate: LGD: 5-14% and HGD: 24-37%) • Recommendations: – Follow q. 2/3 years: • Look for large polyps (>1cm) • Sample extensively Goddard AF. Gut 2010;59:1270-1276 3
5/26/2017 Courtesy of P. Kumarasinghe � Key features: • FG polyposis w/occasional hyperplastic & adenomatous polyps, – sparing the antrum – devt. of intestinal type GCA • Autosomal dominant inheritance (Incomplete penetrance). • No colonic polyps • Point mutations in exon 1B of APC Gut 2012, 61:774-779 The American Journal of Human Genetics 98, 1–13, May 5, 2016 Hyperplastic Polyps Mean age: 65yrs -Sessile/pedunculate -Antrum:60%. Multiplicity: 20%. 15% 25% HP gastritis • Sessile or pedunculated Auto Im. Gastritis React. Gastro. • Size is variable Others 27% 12% Normal 21% Mucosal background 4
5/26/2017 Polypoid foveolar hyperplasia <1cm 208 polypoid lesions reported as hyperplastic polyps Prolapse variant (of hyperplastic polyp) Glands in mid zone Thick muscle bands Polypoid fov. hyperplasia:49% Hyperplastic polyp:31% Thickened wall vessels Cystic glandular dilatation Prolapse polyp:20% 5
5/26/2017 Natural history of hyperplastic polyps Dysplasia:1.8-16.4%; Carcinoma:0.3-7.1% (avg 2.1%) ( > 2.0 27% 2% cm) Stable 3% Disappear Growth/Disappear Increased 68% Goddard AF. Gut 2010;59:1270-1276 Differential diagnosis of hyperplastic polyps is Hyperplastic Polyps – Diff. Dx challenging on a superficial pinch biopsies Peutz-Jeghers Cowden’s Cronkhite-Canada Juvenile polyposis Syndrome Disease Syndrome autosomic non-inherited Inheritance autosomal dominant autosomal dominant dominant (sporadic) Gene SMAD4 or BMPR1A STK11/LKB1 PTEN None Gastric location infrequent (15~25%) 25~50% common common antrum > body or Location of polyp random random random fundus usually small Size of polyp variable usually small (<1cm) variable (<1cm) Lifetime risk of gastric Ca. 15~20% 30% rare about 10% Menetrier ’ s disease •Other differential dx: – – Bile reflux/ post surgery gastritis – Gastritis Polyposa Cystica 6
5/26/2017 Disorganized pits / glands Disorganized pits / glands Juvenile polyps (polyposis) of varying sizes & shapes of varying sizes & shapes • Median age of pts presenting with gastric polyps ~40 years • Rounded and sessile when small but pedunculated with a lobular appearance as they enlarge. • No smooth muscle fibers Setia N. The Oncologist 2015; accepted for publication Subtle intervening septae of smooth muscle strands Peutz-jeghers Unremarkable lamina propria Median age of Dx:16 yrs Pits & glands are grouped/ packeted; Unremarkable epithelium 7
5/26/2017 Cronkhite-Canada Syndrome • Protein-losing enteropathy. • Ectodermal changes • Hamartomatous polyposis. • (IgG4 related condition?) • Variable natural history – 50-60% mortality • Increased risk of GI cancer through the hamartoma-adenoma- carcinoma sequence and de novo malignant change. – Electrolytes imbalance, GI bleeding, opportunistic • Dysplasia is noted in 2-3% of PJ polyps. infections • Malignant potential~10% Gastric Adenoma • Nodule of gastric “ Unequivocal neoplastic dysplasia: (non invasive) process ” Single in 82% of cases • • Broad based polyp w/ marked • Mixed inflammatory 80-90% < 2cm • stromal edema & unevenly infiltrate w/ prominent spaced glands. eosinophilia 8
5/26/2017 Low Grade Dysplasia High Grade Dysplasia Architectural/Cytologic Features of Gastric Dysplasia Glandular disarray,budding, branching and dilatation Nuclear pleomorphism High N/C ratio Loss of nuclear polarity w/ pseudostratification Lack of differentiation w/ mucus depletion Phenotypic Diversity of Gastric Dysplasia Adenomatous Foveolar Pyloric CD10 MUC2 MUC5AC MUC6 (+) (+) (-) (-) Intestinal (Apical membrane) (Goblet cells) (+) (+/-) Foveolar (-) (-) (glands) (-) (+) (+) Pyloric (-) Pre-pyloric nodule (surface) (glands) 9
5/26/2017 • Cuboidal to low columnar cells, • Clear/light eosinophilic cytoplasm, • Round to oval nuclei. Polypoid gastric dysplasia, foveolar type Park DY. AJSP 2008 Pyloric gland Prevalence of foveolar GED: 22% (Adenomatous: 45%, hybrid 33%) (n=69) (n=69) adenoma Type 2 Muc5AC • Foveolar GED is often depressed/flat & associated w/ HGD (p= 0.046). • HGD associated w/ MUC5AC expression regardless of the type (p=0.026). Immunophenotype MUC6 Grade p value Foveolar Intestinal (n=22) Hybrid (n=14) (n=24) HGD (n=25) 15* (63%) 4 (18%) 6 (43%) Low grade (n=35) 9 (37%) 18 (82%) 8 (57%) 0.010 * coexistent intramucosal carcinoma in 8 cases Foveolar differentiation is associated w/ HGD & coexistence of IMC MUC5 Valente P; Gastric Cancer 2014 10
5/26/2017 MUC6 What we know about PGA What is new about PGA • Older pts (mean age: 70 years) • Cardia (8%) , antrum (6%) , pylorus • Females > males (3:1) (3%) • Oxyntic mucosa • 27% in AIG but 73% not, w/ 9% in • Autoimmune gastritis + FAP & 36% in normal mucosa • FAP (no sex predominance); Lynch Sd • 55% LGD [ average size:1.7 cm ] while • 53% with HGD (23 cases) 37% HGD [avg: 3.4 cm] • Pyloric-phenotype (MUC6+, • TVA architecture more common in • < 30% MUC5AC+) HGD (52%) than LGD • GNAS mutation in 48% of cases • 51% coexpressed MUC5AC with (none in intestinal & foveolar dysplasia) MUC6 in an intermixed pattern • KRAS mutation in 41% of cases • Only 7% w/ recurrence at 1 year. Matsubara A. J Pathol 2013;229:579 High Grade Dysplasia Intramucosal adenocarcinomia Tubular PGA with LGD Tubulo-villous PGA with HGD 11
5/26/2017 Middle age female What is your diagnosis? 1. Tubular adenoma 2. Well diff. adenoCA H +/ K + ATP ase 3. Fundic gland polyp MUC6 Chief cells Parietal cells Pepsinogen I 48% 41% Singhi A AJSP. 2012;1030-1035. MUC6 Kushima R. Pathology International 2013 A morphologic continuum….. Anastomosing glands GNAS (55%); Mild atypia (58%) Uyema H AJSP. 2010;609-619. mutation Desmoplasia (16%) Necrosis (8%) Mixed polyps have been MUC5A seen C 12
5/26/2017 NET (Neuroendocrine Tumors) in Autoimmune Gastritis Gastric polyps: characteristics and management strategies Goddard AF. Gut 2010;59:1270-1276 Gastric Neuroendocrine Tumors Types 1,2, 3 are ECL cells tumors 2% of gastric malignancies (0.5% in ‘ 50) • Increasing prevalence (?increase in endoscopic examination) : 9% of intestinal neuroendocrine neoplasia (2.4% in ‘ 50) • • Type Background % Sex # of tumors Size Invasion Mets/ Prognosis Size > 0.5cm 1 Autoimmune Gastritis 70 F Multiple Most are superficial <10% Submucosal Invasion small ECL-cell hyperplasia (65%) (70%) Good CHR 2 MEN-I,ZES, 5-8 M=F Multiple (100%) Small superficial 10% (<1cm) SYN Hyperparathyroidism Good ECL-cell hyperplasia CD-56 Non atrophic or hypertrophic mucosa 3 Sporadic 20 M Single Variable deep 65% Normal or chronic gastritis but (80%) Mod/Poor (100%) no atrophy Grade 1 (<2 mitoses x 10 HPF; <2% Ki67 index) Grade 2 (<20 mitoses x 10 HPF; 3-20% Ki67 index) 13
Recommend
More recommend