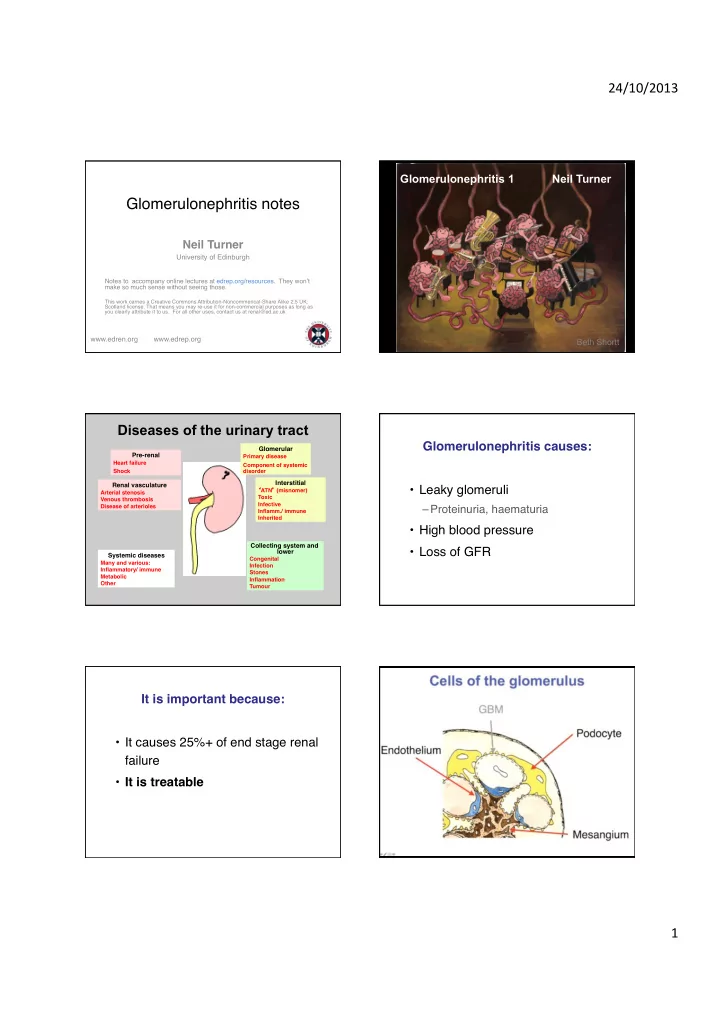
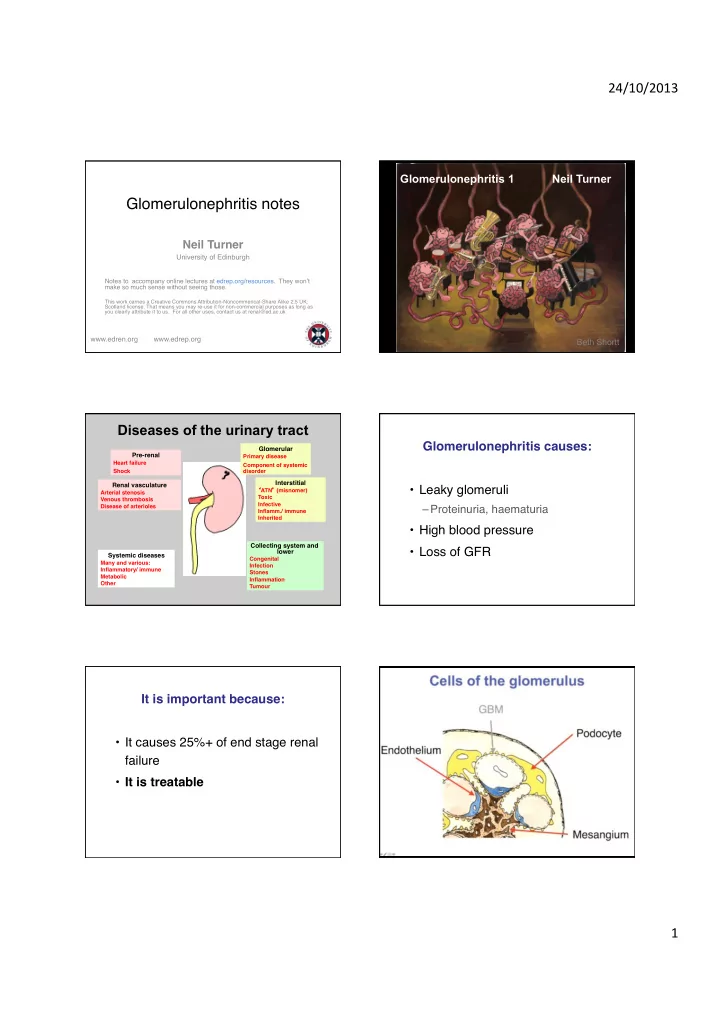
24/10/2013' Glomerulonephritis 1 Neil Turner Glomerulonephritis notes ! Neil Turner ! University of Edinburgh ! Notes to accompany online lectures at edrep.org/resources. They won’t make so much sense without seeing those. ! ! This work carries a Creative Commons Attribution-Noncommerical-Share Alike 2.5 UK: Scotland license. That means you may re-use it for non-commercial purposes as long as you clearly attribute it to us. For all other uses, contact us at renal@ed.ac.uk ! www.edren.org www.edrep.org ! Beth Shortt Diseases of the urinary tract Glomerulonephritis causes: ! Glomerular ! Pre-renal ! Primary disease ! Heart failure ! Component of systemic Shock !! !! disorder Interstitial ! Renal vasculature ! • Leaky glomeruli ! � ATN � (misnomer) ! Arterial stenosis ! Toxic ! Venous thrombosis ! Infective ! Disease of arterioles ! – Proteinuria, haematuria ! Inflamm./ immune ! Inherited ! • High blood pressure ! Collecting system and • Loss of GFR ! lower ! Systemic diseases ! Congenital ! Many and various: ! Infection ! Inflammatory/ immune ! Stones ! Metabolic ! Inflammation ! Other ! Tumour ! It is important because: ! • It causes 25%+ of end stage renal failure ! • It is treatable ! 1'
24/10/2013' … clinical signs of renal disease are often late or non-specific Clinical effects of glomerular disease Physical signs: problems with fluid Physical signs: problems with fluid This and similar figures from Kinsey Smith Increased extravascular fluid ! Increased intravascular fluid ! (e.g. nephrotic syndrome, liver failure, generalized chronic volume overload) ! Physical signs: loss of filtration Proteinuria Proteinuria Glomerular > 60kD filtration barrier < 20kD Tubular metabolism (saturable) Albumin 67kD β 2 microglobulin 12kD Ig light chain 25kD 2'
24/10/2013' Glomerular proteinuria Glomerular proteinuria • Albumin is the hallmark • Microalbuminuria can be helpful • Albuminuria may be transient in: – occurs before overt proteinuria in glomerular disease – Fever, CHF, exercise – Orthostatic – also in vascular disease (why?) • Otherwise implies significant glomerular • Quantity is helpful disease … and microalbuminuria Proteinuria: quantitative Haematuria per 24h prot/creat origin and microscopy <150mg <15 normal 1-3g 100-300 equivocal >3g 300mg/mmol glomerular Causes haematuria Schematic glom HAEMATURIA Cysts Tumour Vascular malformation Glomerular disease inflammatory degenerative Infarction Interstitial disease (incl. papillae) Clotting disorders Myoglobin Metabolites (porphyria) Colour (eg beetroot) INFECTION Drugs CANCER Stones Trauma Repeat if could be: ! Exercise Menstruation 3'
24/10/2013' Alport/N GBM pic Urine analysis by cell sorter Alp/N GBM Pic of tablets Normal and Alport GBM ANT Causes of glomerular disease ! Most glomerulonephritis is autoimmune ! There are some important ! The evidence for this is ! • Immunoglobulin deposits ! • Inherited (e.g. Alport syndrome) ! • Inflammatory cells ! • Metabolic (e.g. diabetes) ! • Response to treatment ! • Other ! • Evidence from animal models ! causes of glomerulopathies, but ….. ! – induced by immunisation/ sensitisation ! – dependence on antibodies or CMI ! Antigens in glomerulonephritis GBM The glomerulus has a Goodpasture ʼ s disease Podocyte restricted range of Endothelium Membranous ?Small vessel nephropathy responses to injury vasculitis Circulating Planted antigens immune ?SLE complexes ?infections Cryoglobulinaemia Serum sickness ?Endocarditis 4'
24/10/2013' The spectrum of glomerular diseases Glomerulonephritis 2 Neil Turner SLE IgA nephropathy Minimal change Anti-GBM nephropathy disease Small FSGS Diabetic vessel nephropathy vasculitis MCGN Membranous Post-streptococcal Amyloidosis nephropathy glomerulonephritis Nephrotic Nephritic Mechanism Mechanism • Injury to podocytes • Inflammation • Changed • Reactive cell architecture: proliferation • Scarring Haematuria • Breaks in GBM • Deposition of • Crescent formation matrix or other elements Proteinuria www.edren.org Beth Shortt Nephrotic syndrome ! Individual glomerular diseases ! • Proteinuria > 3.5 g/day ! Proteinuric diseases ! • Albumin < 30 g/l ! • Oedema ! ! ! Haematuric diseases ! ! A variety of complications arise, beginning at lower levels of proteinuria. ! Complications of nephrosis ! Causes of nephrotic syndrome ! Oedema (a manifestion) ! PODOCYTE DISEASES !! ! ! Sodium restriction, diuretics ! • Minimal change nephropathy ! ! • FSGS ! 1. Infection ! • Membranous nephropathy ! ! ! ! Prevention, immunisation ! SYSTEMIC DISEASES ! 2. Thrombosis (venous, arterial) ! • Diabetes mellitus ! ! ! ? anticoagulation ! • Amyloidosis ! 3. Hyperlipidaemia ! ! ! ! ? HMG CoA reductase inhibitors ! 5'
24/10/2013' Causes of nephrotic syndrome ! Management of nephrotic syndrome ! ! SCARRING !! Establish cause ! ! • after an inflammatory GN or other ! � Renal biopsy usually required ! cause of glomerular damage ! Treat cause ! ! ! if possible ! ! Treat / prevent oedema, complications ! ! ! Minimal change nephropathy ! FSGS: description not a diagnosis ! • Focal ! • Normal light microscopy ! • Segmental ! • Common in children (esp • GlomeruloSclerosis ! Caucasian) ! • Usually steroid-responsive ! • Little scars ! • Does not progress to renal failure ! FSGS ! Primary FSGS + nephrotic syndrome �! • Primary FSGS with nephrotic syndrome ! • More common as age rises ! • Old focal injury and other disorders ! • Relatively (?completely) steroid- – Previous thrombotic microangiopathy ! resistant ! – Microemboli ! • May progress to ESRF ! – HIV infection ! • May recur after renal transplantation ! – Morbid obesity ! – Reduced nephron number ! ! 6'
24/10/2013' Membranous nephropathy ! Membranous: treatment ! • Common cause of NS in adults ! 1. Maximise ‘nephroprotection’ ! • Autoantibody to podocyte antigen ! 2. Specific therapy ! • Usually idiopathic, but secondary in ! • Alkylating agents ! – Reaction to gold, Hg, some other drugs ! – Cyclophosphamide, chlorambucil ! – As part of some other conditions ! • Cyclosporin ! – Controversy about how often cancer-related ! – Lowers proteinuria transiently ! • Outcome - 1/3 : 1/3 : 1/3 ! ! • Rituximab (anti-B cell) ! – Anecdotally slow but may work ! – No RCT evidence. Expensive, toxic ! Nephritis and � nephritic syndrome � ! Features found to varying degrees in 3 nephritic diseases different conditions ! • Haematuria – always ! • Proteinuria – usually ; requires podo and 2 systemic ones ! injury ! • Sodium (fluid) retention ! • Hypertension ! Nephritis and � nephritic syndrome � Post-streptococcal GN ! ! • Follows Group A Strep infections ! Primary glomerular diseases ! • Post-Streptococcal (classic nephritic syndrome) ! • Full nephritic syndrome is characteristic, • IgA nephropathy ! but severity varies ! • Goodpastures (anti-GBM) ! • Ig and complement deposits under flom endothelium and epithelium ! Systemic diseases ! • SLE ! • Low C3 ! • Small vessel vasculitis ! • Fluid retention prominent; diuretics useful ! ! 7'
24/10/2013' IgA nephropathy ! Anti-GBM (Goodpasture’s) Disease ! • Very common ! • Rare (1/million/y) ! • IgA in mesangium; cause unknown ! • Autoantibody to α 3 chain of type IV (basement membrane) collagen ! • Spectrum of presentations ! • Renal or lung disease, or both ! ! Mild to severe ! (Goodpasture syndrome) ! ! Asymptomatic haematuria to ESRF ! ! • Characteristically very RPGN ! • No proven treatment ! !! • Plasma exch, cyclophos, steroid ! !! Crescentic nephritis ! Rapidly progressive glomerulonephritis, RPGN ! What about MCGN (MPGN)? � ! • Small vessel vasculitis ! • Mesangiocapillary = ! • SLE ! • Membranoproliferative ! • Anti-GBM (Goodpasture � s) disease ! • Complex! ! • Aggressive phase of other inflamm nephritis (eg IgA, post-Streptococcal) ! ! It’s not all over: Progressive deterioration after glomerular injury ! www.edren.org Beth Shortt Scarred kidneys 8'
24/10/2013' Prognostic markers in glomerular (and other renal) disease � ! • Creatinine (or GFR) ! • Proteinuria ! • Hypertension ! • Degree of scarring – especially interstitial scarring ! Preventing progression of renal Links ! injury ! Music of GN with music – www.edrep/resources ! • or … ! • Low protein diet ! not recommended ! historyofnephrology.blogspot.com – to read about ! • Lipid control ! ! no, but justified anyway ! • Dropsy (nephrotic syndrome) ! • Blood pressure ! YES ! • The MDRD study; BP and dietary protein ! • ACE inhibition ! YES ! www.edren.org www.edrep.org neil.turner@ed.ac.uk ! ! 9'
Recommend
More recommend