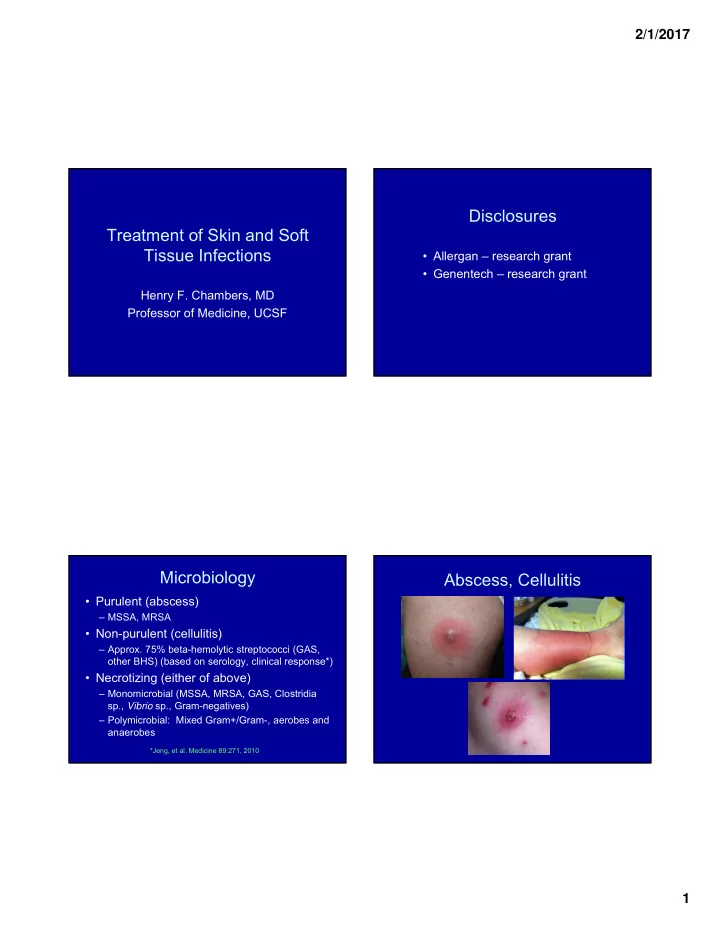
2/1/2017 Disclosures Treatment of Skin and Soft Tissue Infections • Allergan – research grant • Genentech – research grant Henry F. Chambers, MD Professor of Medicine, UCSF Microbiology Abscess, Cellulitis • Purulent (abscess) – MSSA, MRSA • Non-purulent (cellulitis) – Approx. 75% beta-hemolytic streptococci (GAS, other BHS) (based on serology, clinical response*) • Necrotizing (either of above) – Monomicrobial (MSSA, MRSA, GAS, Clostridia sp., Vibrio sp., Gram-negatives) – Polymicrobial: Mixed Gram+/Gram-, aerobes and anaerobes *Jeng, et al. Medicine 89:271, 2010 1
2/1/2017 Case 1 S. aureus Skin and Soft Tissue Infections An 18 year high school senior male is seen in your office for an approximately 2 cm abscess of the right buttock with 5 cm diameter of surrounding erythema. No allergies. He is afebrile, other vital signs are normal, and exam is normal • 95% of all S. aureus infections except for the abscess. Which of the following is the most • Community MRSA (methicillin- appropriate management? resistant S. aureus ) causes > 50% of 1. Incision and drainage SSTIs 2. Incision and drainage + cephalexin 3. Incision and drainage + TMP/SMX 4. Incision and drainage + clindamycin Study Subjects and Culture Results Randomized, Double-Blind Trial of Clindamycin, Single Abscess < 5 cm Trimethoprim-Sulfamethoxazole, or Placebo for Uncomplicated Skin and Soft Tissue Infections All Subjects (n=786) Caused by Community-Associated Methicillin- Resistant Staphylococcus aureus Male, n (%) 448 (57.0) > 18 years, n (%) 505 (64.2) Study Sponsor: Division of Microbiology and Diseases Positive culture, n (%) 718 (91.3) National Institute of Allergy and Infectious Diseases National Institutes of Health Staph. aureus , n (%) 527 (67.0) MRSA, n (%) 388 (49.8) PI: Henry F. Chambers, MD Co-Investigators: Loren Miller, MD (UCLA Harbor); Robert Daum, MD (University of Chicago) 2
2/1/2017 Efficacy at Test of Cure* Efficacy at Test of Cure Single Abscess < 5 cm Single Abscess < 5 cm Clinda TMP/SMX Placebo TMP-SMX Placebo vs Placebo vs 300 mg tid 160/800 bid vs Clinda Clinda TMP/SMX ITT ITT 221/266 215/263 177/257 Cure -1.3% -14.2% -12.9 ∆ cure rates 83.1% 81.7% 68.9% Cure rate -8.4% - 5.7% -22.0% - -6.4% -20.8% - -5.0% 95% CI 78.3% - 87.9% 76.8% - 86.7% 62.9% - 74.9% 95% CI 0.7324 0.0001 0.0008 p-value Evaluable – similar results but higher cure rates Evaluable – similar results * 10-14 days after 10-day course of therapy Efficacy at Test of Cure Reasons for Clinical Failure - ITT Staph. aureus, Single Abscess – Evaluable Population Clinda (n) TMP/SMX (n) Placebo (n) Clinda T/S Placebo (n=266) (n=263) (n=257) Staph. aureus Failures, N 45 48 80 94.4% (157) 93.1% (147) 76.1% (102) Cure rate Missed TOC, N 28 31 37 90.1% - 97.9% 88.9% - 97.4% 68.5% - 83.7% 95% CI Worse 1 o lesion, N 3 2 5 <0.0001 <0.0001 -- p-value vs Placebo New infection, N 6 9 32 Non- Staph. aureus Rescue meds, N 12 15 33 90.5% (57) 90.8% (59) 90.8% (69) Cure rate 1.0000 1.0000 -- p-value vs All other, N 9 6 4 Placebo 3
2/1/2017 Reasons for Clinical Failure – OMFU Other Outcomes Single Abscess < 5 cm Clinda T/S Placebo (n=266) (n=263) (n=257) Failures, N 57 71 96 • Cures rates similar for children and adults Missed TOC, N 32 37 39 • MRSA and MSSA cure rates similar Worse 1 o lesion, N 1 0 1 New infection, N 13 26 46 Rescue meds, N 12 15 33 All other, N 12 68 6 Main Results • TMP/SMX 320/1600 mg bid vs Placebo, 7d • Cure rates of 73.6% versus 80.5% – 6.9% higher (95% CI 2.1 – 11.7) for TMP/SMX • TMP/SMX with higher rate of secondary benefits • Adverse event rates similar New Engl J Med 374:823, 2016 New Engl J Med 374:823, 2016 4
2/1/2017 Key Points • 500 subjects with wound infections treated as out-patients – 2 DS TMP/SMX vs Clinda 300 mg qid, 7d • 65% S. aureus, 40% MRSA • Overall cure rate 92%, <1% difference between the two. • Fewer recurrences/new infections with clinda Clin Infect Disease 2016 Mar 29. pii: ciw177. [Epub ahead of print] Clin Infect Disease 2016 Mar 29. pii: ciw177. [Epub ahead of print] Case 2 28 year old female, otherwise healthy, is seen in your office with a tender lesion over her L lateral calf which she first noticed 2 days ago and is now more painful and has increased in size. No drug allergies. She is afebrile, other vital signs are normal and the exam is remarkable only for a 6.5 x 8 cm non-purulent, non-fluctuant, erythematous lesion that is tender and slightly swollen. Which antibiotic would you recommend? 1.No antibiotic needed 2.Cephalexin 3.TMP/SMX 4.Clindamycin 5
2/1/2017 Patient Characteristics Lesion Types Cellulitis, Abscess > 5 cm, Mixed, Multiple All Subjects (n=534) • Abscess only 30.6% – Mean Volume: 21.9 cm 3 (max 628 cm 3 ) Male, n (%) 247 (52.3) – Area of erythema: 44 cm 2 (range 0-528 cm 2 ) > 18 years, n (%) 369 (70.4) • Cellulitis only 53.6% I&D performed, n (%) 233 (44.5) – Area of erythema: 60.5 cm 2 (range 0-1131 Purulent drainage, n (%) 237 (45.2) cm 2 ) Positive culture, n (%) 277 (52.9) • Mixed 15.7% S. aureus , n (%) 219 (41.8) MRSA, n (%) 167 (31.9) Efficacy at Test of Cure Efficacy at Test of Cure* Cellulitis, Larger Abscess > 5 cm, Mixed, Multiple Cellulitis, Larger Abscess > 5 cm, Mixed, Multiple Clinda TMP/SMX TMP-SMX vs Clinda 300 mg tid 160/800 mg bid ITT ITT -2.6% 212/264 202/260 ∆ cure rates Cure -10.2% - 4.9% 80.3% 77.7% 95% CI Cure rate 0.52 75.2% - 85.4% 72.3% - 83.1% p-value 95% CI Evaluable Evaluable – similar results, higher cure rates -1.2% ∆ cure rates -7.6% - 5.1% 95% CI 0.77 p-value * 10-14 days after 10-day course of therapy 6
2/1/2017 Efficacy at Test of Cure: Cellulitis vs Abscess Other Outcomes Evaluable Population Clindamycin TMP/SMX Cellulitis, Larger Abscess > 5 cm, Mixed, Multiple Cellulitis Cure rate 110/121 110/127 • Cures rates similar for children and adults (90.9%) (86.6%) ∆ Clinda – TMP/SMX (95% CI) 4.3% (-4.6% – 13.1%) • MRSA and MSSA cure rates similar Abscess Cure rate (%) 63/73 64/72 (86.3%) (88.9%) ∆ Clinda – TMP/SMX (95% CI) -2.6 (-15.0 – 9.8) Logistic Regression Model: Treatment effect: p = 0.87 Disease group: p = 0.81 Interaction: p = 0.36 Clindamycin Resistance is Associated Recurrences at 1 Month in Cured Patients with Treatment Failure Stratum Clinda TMP/SMX Placebo Stratum Sensitive Resistant Abscess < 5 cm* 15/221 29/215 22/177 Abscess < 5 cm* 25/170 (14.7%) 6/13 (46.2%) (6.8%) (13.5%) (12.4%) Larger abscess, 11/102 20/92 n/a Larger abscess, 7/84 (8.3%) 4/15 (26.6%) cellulitis, mixed, (10.7%) (21.7%) cellulitis** multiple** Combined results ¶ 32/254 (12.6%) 10/28 (35.7%) Combined results ¶ 26/323 49/307 22/177 (8.0%) (16%) (12.4%) ∆ R-S (95% CI) 23.1% (6.0% - 43.6%) ∆ TMP/SMX-Clinda 7.9% (2.6% to 13.3%) (95% CI) *p = 0.01, **p = 0.06, ¶ p = 0.003 Clinda v TMP/SMX: *p = 0.025, **p = 0.049, ¶ p = 0.002 7
2/1/2017 Adverse Events - Combined Other Safety Data • Clindamycin (n=524) Clinda TMP/SM Placebo – 2 hospitalizations for infection: 1 peri-rectal X and 1 recurrent abscess at OMFU in IVDU Number of subjects 524 519 255 • TMP/SMX (n=519) Diarrhea* 73 (13.9%) 45 (8.7%) 20 (7.8%) – 6 hospitalizations for worsening cellulitis or abscess Any GI** 98 (18.7%) 74 40 (15.7%) – 1 drug-related SAE: rash, hepatitis, (14.2%) thrombocytopenia Rash ¶ 15 (2.9%) 5 (1%) 6 (2.4%) • Placebo (n=255) – 1 hospitalization for a peri-rectal abscess Clinda vs TMP/SMX: *p = 0.008, **p = 0.055 ¶ p = 0.04 Case 3 Clindamycin vs TMP/SMX for uSSSI Summary An 28 year old female, otherwise healthy, presents is seen in your office with a tender lesion over her L lateral calf which • Clindamycin and TMP/SMX were superior to placebo: she first noticed 2 days ago and is now more painful and has 12% higher marginal cure rates for abscess < 5 cm increased in size. No drug allergies. She is afebrile, other vital • Clindamycin and TMP/SMX had similar efficacies signs are normal and the exam is remarkable only for a 6.5 x 8 cm non-purulent, non-fluctuant, erythematous lesion that is – For patients with abscesses only tender and slightly swollen. What antibiotic would you – For patients with cellulitis only or mixed infections recommend? • Efficacies similar in children and adults, MRSA, MSSA • Recurrent infections more common in subjects treated 1. Cephalexin with TMP/SMX 2. Cephalexin + TMP/SMX • Side effects were similar, almost all mild or moderate • Either clindamycin or TMP/SMX is acceptable for treatment of abscess or cellulitis 8
Recommend
More recommend