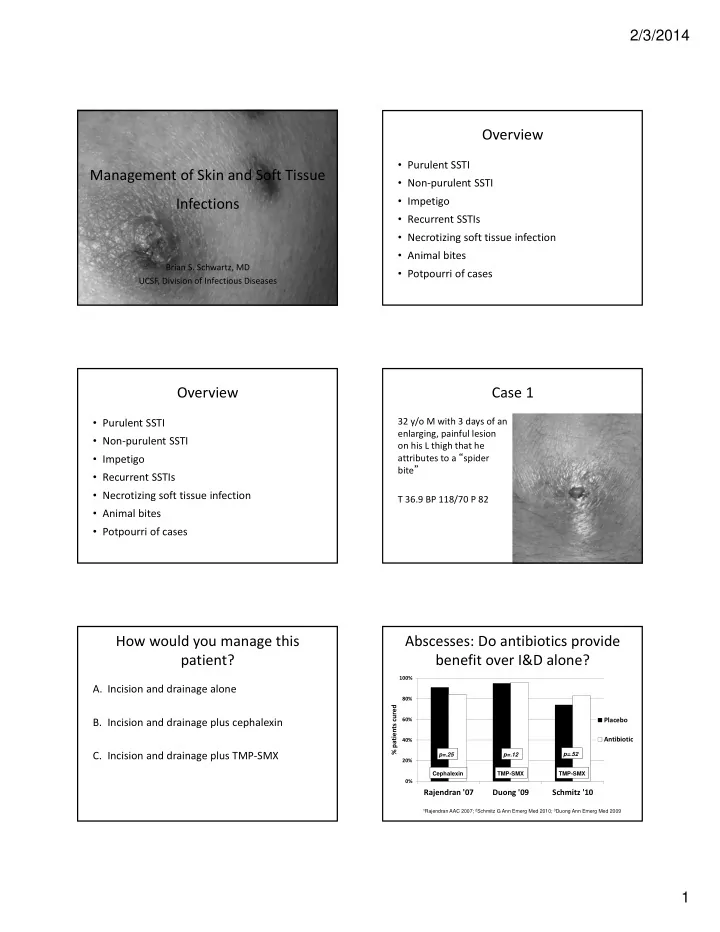
2/3/2014 Overview • Purulent SSTI Management of Skin and Soft Tissue • Non ‐ purulent SSTI • Impetigo Infections • Recurrent SSTIs • Necrotizing soft tissue infection • Animal bites Brian S. Schwartz, MD • Potpourri of cases UCSF, Division of Infectious Diseases Overview Case 1 32 y/o M with 3 days of an • Purulent SSTI enlarging, painful lesion • Non ‐ purulent SSTI on his L thigh that he attributes to a “ spider • Impetigo bite ” • Recurrent SSTIs • Necrotizing soft tissue infection T 36.9 BP 118/70 P 82 • Animal bites • Potpourri of cases How would you manage this Abscesses: Do antibiotics provide patient? benefit over I&D alone? 100% A. Incision and drainage alone 80% % patients cured B. Incision and drainage plus cephalexin 60% Placebo Antibiotic 40% C. Incision and drainage plus TMP ‐ SMX p=.52 p=.25 p=.12 20% Cephalexin TMP-SMX TMP-SMX 0% Rajendran '07 Duong '09 Schmitz '10 1 Rajendran AAC 2007; 2 Schmitz G Ann Emerg Med 2010; 3 Duong Ann Emerg Med 2009 1
2/3/2014 Is treatment failure the only Microbiology of Purulent SSTIs important endpoint? Recurrent SSTI? • Duong : 10 days – 9% TMP ‐ SMX vs. 28% placebo , p = .02 • Schmitz: 30 days – 13% TMP ‐ SMX vs 26% placebo, p= .04 Schmitz G Ann Emerg Med 2010; Duong Ann Emerg Med 2009 Moran NEJM 2006 Antibiotic therapy is recommended Empiric oral antibiotic Rx for abscesses associated with: for uncomplicated purulent SSTI • Severe disease, rapidly progressive with Drug Adult Dose associated cellulitis or septic phlebitis TMP/SMX DS 1 ‐ 2 BID • Signs or symptoms of systemic illness Doxycycline, Minocycline 100 BID • Associated comorbidities, immunosuppressed Clindamycin 300 ‐ 450 TID • Extremes of age Linezolid 600 BID • Difficult to drain area (face, hand, genitalia) *Rifampin is NOT recommended for routine treatment of SSTIs • Failure of prior I&D Liu C. Clin Infect Dis . 2011 Overview Inducible clindamycin resistance? • When to consider? • Purulent SSTI – erythromycin – resistant and • Non ‐ purulent SSTI clindamycin –susceptible • Frequency – 0 ‐ 7% • Impetigo • How to test ‐ D ‐ test • Recurrent SSTIs • What to do if D ‐ test + but • Necrotizing soft tissue infection clindamycin being used? – Improving – continue • Animal bites – Failing or moderate/severe C • Potpourri of cases E infection ‐ change 2
2/3/2014 How would you manage this Case 2 patient? 28 y/o woman presents with erythema of her left A. Clindamycin 300 mg TID foot over past 48 hrs No purulent drainage, B. Cephalexin 500 mg QID, monitor clinically exudate , or fluctuance. with addition of TMP/SMX if no response T 37.0 BP 132/70 P 78 C. Cephalexin 500 mg QID + TMP/ SMX 1 DS BID Eels SJ et al Epidemiology and Infection 2010 Nonpurulent Cellulitis: pathogen? Cephalexin vs. Cephalexin + TMP ‐ SMX in patients with Uncomplicated Cellulitis ‐ hemolytic strep vs. S. aureus ? • Prospective study, hospitalized patients (N=248) N=146 Methods – Acute and convalescent titers (ASO and anti ‐ DNaseB) – Rx with ‐ lactam antibiotics (cefazolin/oxacillin) Results – 73% due to ‐ hemolytic strep; 27% none identified – 96% response rate to ‐ lactam antibiotic Siljander T. Clin Infect Dis . 2008 Jeng A. Medicine 2010. Elliott Pediatrics 2009 Pallin CID 2013; 56: 1754 ‐ 1762 Empiric treatment of uncomplicated Summary: empiric management of SSTIs nonpurulent cellulitis? Purulent Non ‐ purulent • Anti ‐ ‐ hemolytic strep antibiotic (+/ ‐ anti ‐ MSSA) ( β‐ hemolytic strep) (MRSA) • Cephalexin 500 QID Drug Adult Dose • I&D • Dicloxacillin 500 QID Uncomplicated Consider addition of anti ‐ MRSA Cephalexin 500 QID Consider addition of MRSA active antibiotic in select situations 1 agent if no response 1 Dicloxacillin 500 QID • I&D plus vancomycin (or • Vancomycin (or Clindamycin* 300 ‐ 450 TID Complicated alternative) 2 alternative) 2 Linezolid* 600 BID 1. Systemic illness, purulent cellulitis/wound infection, comorbidities, extremes of age, *Have activity against MRSA abscess difficult to drain or face/hand, septic phlebitis, lack of response of to I&D alone. PO antibiotic : TMP ‐ SMX 1 DS BID, Clindamycin 300 mg TID, Doxycycline 100 PO BID • If poor response, add anti ‐ MRSA antibiotic 2. Daptomycin, linezolid, tigecycline, telavancin, ceftaroline 3
2/3/2014 Impetigo Overview • Purulent SSTI • Non ‐ purulent SSTI • Impetigo • Recurrent SSTIs Classic impetigo • Necrotizing soft tissue infection • Animal bites • Potpourri of cases Bullous impetigo Ecythema Impetigo Overview • Definition: superficial, intra ‐ epidermal infection • Purulent SSTI • Epi: Common in children, highly communicable • Non ‐ purulent SSTI • Impetigo • Pathogens: S. aureus, Group A strep • Recurrent SSTIs • Treatment: • Necrotizing soft tissue infection – Few lesions (topical = systemic) • Mupirocin or Retapamulin ointment • Animal bites – Multiple lesions (systemic >> topical) • Potpourri of cases • Pick agent(s) active against CA ‐ MRSA and Group A strep How would you manage this Case 3 patient? • Patient presents with 4 th abscess in 4 months A. Emphasize personal hygiene measures • Prior abscesses have been treated with I&D B. Decolonize with mupirocin and chlorhexidine and antibiotics with resolution C. Decolonize with TMP ‐ SMX and rifampin • He asks if there is anything he can do to prevent recurrences D. Give daily low dose clindamycin 4
2/3/2014 How to Manage Recurrent Skin and Decolonization strategies Soft Tissue Infections? • Intranasal mupirocin: + data in MSSA SSTI w/ + nasal Cx • Chlorhexidine washes alone: not effective Host • Suppressive oral antibiotics: clindamycin some efficacy • Bleach baths: no benefit in recent RCT • Oral therapy with rifamycins: personal experience Environment Pathogen Raz R. Arch Int Med. 1996; Ellis et al , AAC ’ 07. Rahimain et al , ICHE ’ 07; Whitman TJ. Infect Control Hosp Epidemiol. 2010; Klempner MS. JAMA 1988; Wheat J. JID. 1981. Kaplan SK. Clin Infect Dis. 2013 Combination therapy? Bleach baths alone? Mupirocin vs. mupirocin + chlorehexidine vs. mupirocin + bleach bath 80% • Population: 70% Colon. Clear 4m Repeat SSTI 6 m – Children with S. aureus SSTI or invasive infections 60% • Intervention: 50% 40% – Randomized to routine hygiene measures (N=492) +/ ‐ “bleach baths” 2x/week for 3 months (N=495) 30% 20% • Outcomes: 10% – Recurrent SSTI: 17% bleach baths vs. 21% control 0% Control Mup Mup+Chlor Mup+Bleach Kaplan SK. Clin Infect Dis. 2013 Fritz SA. Infect Control Hosp Epi. 2011 PCN for Prevention of Recurrent Recurrent SSTI among Cases and Household Contacts Cellulitis ( Mupirocin plus chlorhexidine ) • Multicenter, double ‐ blind RCT 274 pts with recurrent cellulitis p=.02 – Penicillin 250 mg BID vs. placebo x 12 months p=.008 • Patient characteristics: p=.02 – Chronic edema (66%), venous stasis (25%), tinea pedis (36%) p=.12 • Outcomes: – Recurrent cellulitis: 22% (PCN) vs. 37% (placebo), p=.01 – After treatment stopped, no difference Fritz CID 2012; 54: 743 ‐ 51 Thomas NEJM 2013; 368: 1695 ‐ 703 5
2/3/2014 Overview Case 4 • Purulent SSTI • 34 y/o M comes in with arm pain, fever • Non ‐ purulent SSTI • Temp 38.9, HR 105, SBP • Impetigo 100, RR 20 • Recurrent SSTIs • Appears ill and in more • Necrotizing soft tissue infection pain than what you • Animal bites would expect for • Potpourri of cases cellulitis What would your empiric therapy Necrotizing skin and skin structure be in this case? infections • Definition: infections of any layer within the soft A. Cephalexin plus TMP ‐ SMX, send home tissue compartment that are associated with necrotizing changes B. Clindamycin, piperacillin ‐ tazobactam, and vancomycin • Monomicrobial – associated w/ minor injuries C. Call surgery, vancomycin and ceftriaxone D. Call surgery, clindamycin, piperacillin ‐ • Polymicrobial – associated w/ abdominal surgery, decub ulcers, tazobactam, and vancomycin IVDU, spread from GI tract Necrotizing soft tissue infections: Why is early diagnosis so important? risk factors Mortality rate: > 30% • IVDU • Diabetes • Obesity • Chronic immune suppression Anaya DA. Clin Infect Dis . 2007 Wong CH. Jour of Bone and Joint Surg. 2003 6
Recommend
More recommend