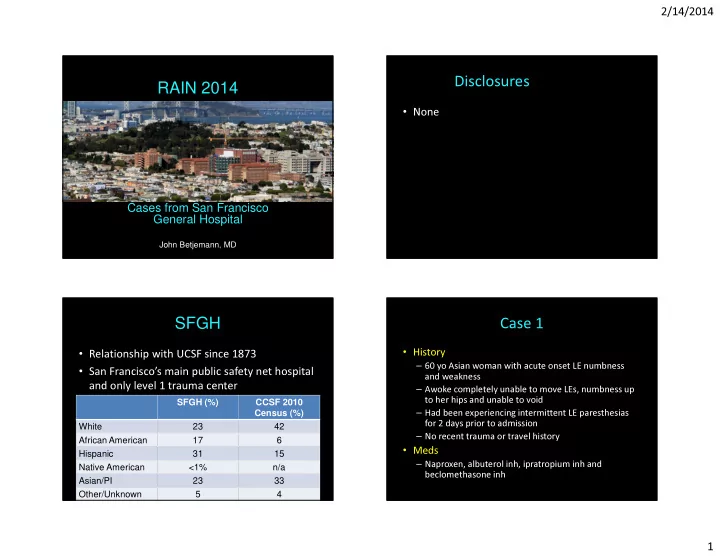
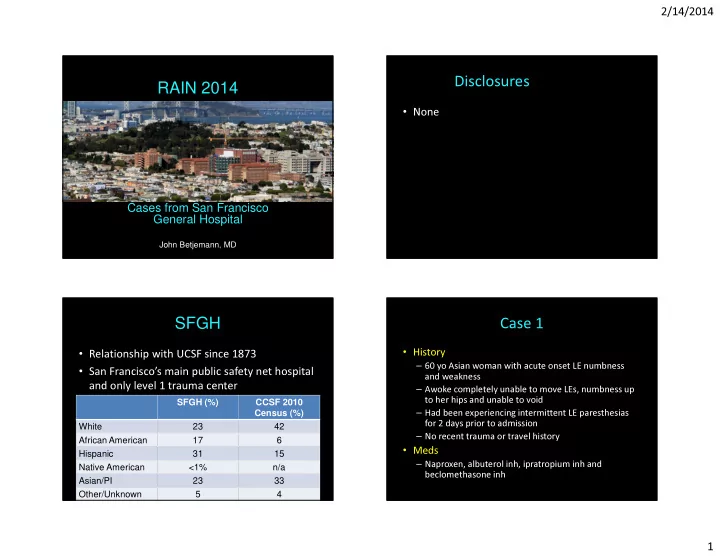
2/14/2014 Disclosures RAIN 2014 • None Cases from San Francisco General Hospital John Betjemann, MD SFGH Case 1 • History • Relationship with UCSF since 1873 – 60 yo Asian woman with acute onset LE numbness • San Francisco’s main public safety net hospital and weakness and only level 1 trauma center – Awoke completely unable to move LEs, numbness up SFGH (%) CCSF 2010 to her hips and unable to void Census (%) – Had been experiencing intermittent LE paresthesias White 23 42 for 2 days prior to admission – No recent trauma or travel history African American 17 6 • Meds Hispanic 31 15 – Naproxen, albuterol inh, ipratropium inh and Native American <1% n/a beclomethasone inh Asian/PI 23 33 Other/Unknown 5 4 1
2/14/2014 Case 1 Case 1: Exam • PMH • MS and CN exam unremarkable (including – Breast CA s/p lumpectomy and XRT in 2011 ophthalmologic exam) – Gastritis and asthma • Motor exam • Review of Systems – No pronator drift, symmetric fast finger taps – 10 lb unintentional wt loss over last 1-2 weeks – Flaccid paraparesis – Gastroenteritis 3 days prior to admission • No movement of LLE • Flicker of movement in proximal RLE and 4-/5 distally – Chronic cough with chest CT concerning for • Reflexes: 2+ in the UEs and absent in the LEs interstitial lung disease • Sensation: decreased to all modalities to nipple – Recent arthralgia in hands – Recent night sweats but no fevers line • Rectal tone was decreased – No issues with vision, speech or swallowing Case 1: Imaging Case 1: Question 1 Which is the first diagnostic test you would like to perform? 1. CT brain 83% 2. MRI brain 3. MRI C spine 4. MRI total spine 5. Lumbar puncture 8% 6% 2% 0% n n e . . . a i a i n . . . i n r r r p i u b b s p s t T I C c C R l n M I a u R t o p M t r I a R b M m u L Sag T2 Sag T2 Sag T1 post con 2
2/14/2014 Case 1: Question 2 Case 1: Imaging and Labs • What is your most likely diagnosis? CBC, Chem-7, LFTs normal 41% • CSF 1. Infectious (viral, TB etc.) • 161 RBC, 374 WBC (97% myelitis 22% 2. Multiple sclerosis neut), 194 protein, 16% 14% 3. Sarcoidosis glucose 51 (120) 6% • 0% 4. Neuromyelitis optica Serum ACE, dsDNA, ANA, . . s . . . . . . . s i . . . . v i r o . . c i ( e d s i c t l t i t e s s c o i l i a s 5. Paraneoplastic myelitis u c e n o e r y p l n i l a m o o RF, RPR, B12, PPD and HIV c t p S c e t i o e l r n d n f u u a e I M r x e a i N P M 6. Mixed connective tissue all negative/normal disorder with autoimmune • SSA/SSB, NMO, IgG index, myelitis (i.e. Sjogren’s, lupus) oligoclonal bands all pending Axial FLAIR Axial T2 Case 1: Question 4 Case 1: Question 3 Based on the current information, what is your Given the LP results, now what is your most next step? likely diagnosis? 60% 1. Infectious (viral, TB etc.) myelitis 50% 1. Start IV solumedrol 2. Multiple sclerosis 2. Start broad spectrum IV antibiotics 35% 3. Sarcoidosis and acyclovir 4. Neuromyelitis optica 3. Initiate IVIG 20% 5. Paraneoplastic myelitis 4. Place a line for plasma exchange 10% 10% 8% 6. Mixed connective tissue disorder with 2% 5. Await pending labs prior to initiating 0% 2% 2% autoimmune myelitis (i.e. Sjogrens, Lupus) treatment . . . . s . . . . . . i . . . . . i r s c i v e o s t ( d i t i c l t e . . G . s c i i s . . . . . u s o e l a n . . I . . l n m p V f o e c y p g i l r o u s I e n t p a m o e n c S e c l d i i o o a t l i d e t n d s a n f u l r o i a n u a e V r t e M r x b i e I e a i I n p N M c P t t I a t r r i a a P l a t w S t S A 3
2/14/2014 Case 1: Question 5 Case 1: Diagnosis After 5 days of IV solumedrol the patient experienced • Initiated empiric solumedrol 1g IV x5 days minimal improvement. The preferred next step in management is? • CSF: 1. Prednisone taper and IVIG – No oligoclonal bands 67% 2. Prednisone taper and immunosuppression – IgG index: 0.77 (0.23-0.64) (Rituximab) • SSA (Ro) Ab: 156 (0-40 AU/mL) 3. Prednisone taper and immunomodulators (interferon) • SSB (La) Ab: 0 (0-40 AU/mL) 23% 4. Another course of IV solumedrol • NMO ab: >160 U/mL (<4) 7% 2% 2% 5. Prednisone taper and plasma exchange followed by immunosuppression (Rituximab) . . . . . . . . . . . . . . . p p p e p a a a s a r t t t u t e e e e o n n n c n o o o o r s s s e s i i i i n n n h n d d d t d o e e e e r r r n r P P P A P Case 1: Follow up Case 1: Pearls • NMO • s/p plasma exchange and 2 doses of Rituximab – Demographics: Asian and African Americans • MRI breast negative for tumor recurrence – Near complete LETM v. partial TM in MS • 2.5 months out with no further attacks – CSF: neutrophilic pleocytosis, eosinophils, relative – Ambulating with cane/walker absence of oligoclonal bands • NMO spectrum disorder – Has not regained bladder function – Overlap with ANA and ENA (particularly SSA/SSB) – Demographics: female, median age at onset 56, more Caucasians – LETM more common than optic neuritis at presentation 4
2/14/2014 Case 2 Case 2 • History • PMH – 33 yo man presents with psychosis and suicidal – Suicide attempt in 9/12 – 1.5 years of paranoid delusions following the end ideation – 1 week prior to admission had intermittent LE of a serious relationship – History of polysubstance abuse (marijuana, paresthesias and numbness – 2-3 days prior to admission the LE symptoms ecstasy and methamphetamine) with rare etoh worsened and he was unable to walk use • Meds • Review of Systems – Noncompliant with risperidone and lorazepam – Recent weight loss but unclear how much – Otherwise unremarkable ROS Case 2: Exam Case 2: Imaging • MS: oriented, normal digit span, 0/3 recall • CN: unremarkable • Motor: normal bulk and tone. 5/5 throughout except 4+/5 in left triceps, interossei and hamstrings • Reflexes: 1+ in the UEs, 3 knees, 2+ ankles, toes down going • Sens: decreased to vibration and proprioception throughout (legs> arms). Pinprick and temperature intact • Coord: dysmetria in all 4 extremities with truncal ataxia • Gait: unable to stand without assistance Sag T2 Axial FLAIR 5
2/14/2014 Case 2: Question 1 Case 2: SG What do you think will be most useful in guiding • More history the differential diagnosis? – Patient admitted to using 1. Serum labs 90% whippets twice daily for a 2. Lumbar puncture year and recently had been 3. More of a history regarding attempting to overdose substance abuse – “thousands of cartridges” 4. All of the above covering his apartment 4% 4% 2% s . . . . b . . . . a . t o r s l u i b m t h a c n a u e r u h o f e p t S r e o f a r o b l m M A l u L Case 2: Question 2 Case 2: Labs Which labs would you expect to be abnormal? • CBC unremarkable 49% – Peripheral smear: hypersegmented neutrophils 1. Vit B12 • Vit B12: 294 (236-888 pg/dL) 2. Homocysteine – was 618 on 9/19/12 3. Methylmalonic acid 24% • Homocysteine: 197 (<10 umol/L) 4. Peripheral smear 16% • Methylmalonic Acid: 3.85 (0-0.4) 5. Answers 1-4 4% 4% 2% – (1-9.99 consistent with mild B12 deficiency) 6. Answers 2-4 2 e . . 4 4 • HIV, RPR, Chem-7 all unremarkable . . 1 n . . - - B e 1 2 i c m e i s s t t n i s r r V s o e e y l l a w w c a o r s s m e m n n h y l A A o p h H i t r e e M P 6
2/14/2014 Case 2: Question 3 Case 2: SG How would you treat this patient? • No improvement in symptoms despite high dose B12 – B12 level: 1108 pg/dL 91% 1. Supportive care – Homocysteine 12 umol/L 2. Daily oral B12 supplementation 3. Daily high dose IM B12 supplementation 6% 4% . . . . . . . . r . 2 s a 1 o c B d e h a l v g i r t o h i r o y y p i l l p a i a u D D S Case 2: Repeat imaging Case 2: Question 4 Would you perform an LP at this time 70% 1. Yes 2. No 30% s o e N Y Sag T2 Axial T2 7
2/14/2014 Case 2: follow up Case 2: Pearls • N 2 0 is an increasingly common drug of abuse • CSF – 1 RBC, 0 WBC, gluc 60 mg/dL, prot 78 mg/dL and is readily available • N 2 O causes the oxidation of Co + to Co ++ , – CSF gram stain and culture negative thereby inactivating B12 in vivo – Oligoclonal bands not detected • B12 is necessary for the synthesis of – IgG index 0.52 methionine which is needed for myelin sheath • Continued with high dose B12 protein supplementation. Patient has not returned • B12 levels may be normal but the patient is for follow up yet functionally B12 deficient Thank You • Questions? 8
Recommend
More recommend