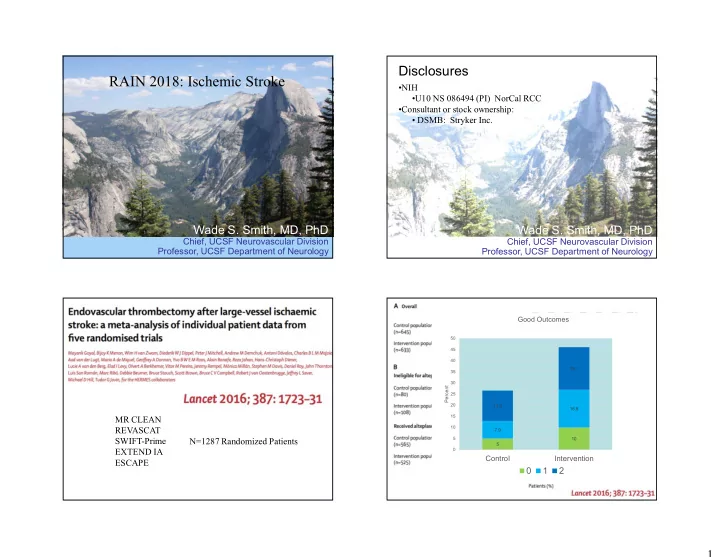
Disclosures RAIN 2018: Ischemic Stroke •NIH •U10 NS 086494 (PI) NorCal RCC •Consultant or stock ownership: • DSMB: Stryker Inc. Wade S. Smith, MD, PhD Wade S. Smith, MD, PhD Chief, UCSF Neurovascular Division Chief, UCSF Neurovascular Division Professor, UCSF Department of Neurology Professor, UCSF Department of Neurology Good Outcomes 50 45 40 19.1 35 30 Percent 25 20 13.6 16.9 MR CLEAN 15 REVASCAT 10 7.9 SWIFT-Prime N=1287 Randomized Patients 5 10 5 EXTEND IA 0 Control Intervention ESCAPE 0 1 2 1
2
Nogueira et al, NEJM 378: 11-21,2018 Nogueira et al, NEJM 378: 11-21,2018 Nogueira et al, NEJM 378: 11-21,2018 3
Albers, et al, Epub NEJM January 24, 2018 Nogueira et al, NEJM 378: 11-21,2018 Albers, et al, Epub NEJM January 24, 2018 4
Outcomes by Time IV t-PA effect? 60 Ischemic Creep? 49 50 46 45 40 30 27 20 17 13 10 0 HERMES DAWN DEFUSE-3 Control Thrombectomy Albers, et al, Epub NEJM January 24, 2018 Late Window Paradox UCSF Acute Stroke Protocol Albers, Stroke: 2017 ePub 5
2018 UCSF Acute Stroke Protocol Major Conclusions • Embolectomy with stent retrievers improve clinical outcome if done with 24 hours of symptom onset for anterior circulation ischemia • Earlier treatment improves outcome if onset < 6 hours • Thrombectomy is safe and effective from 6-24 hours provided they have favorable perfusion • You should be performing CTA in all patients seen within 24 hours of ischemic stroke onset University of California, San Francisco 6
Intracerebral Hemorrhage: Intracerebral Hemorrhage (ICH) - Case Acute and Long-Term Blood Pressure Management • 55 yo construction exec – Poorly controlled hypertension J. Claude Hemphill III, MD, MAS – Slumps over table at board meeting Kenneth Rainin Chair in Neurocritical Care • Arrives at ED 30 min after onset Professor of Neurology and Neurological Surgery – GCS 9 University of California, San Francisco – BP 225/110 Chief of Neurology, San Francisco General Hospital • What do you do with the BP? Past-President, Neurocritical Care Society – Now? UC SF – Later? Disclosures NEUROCRITICAL Research Support: NIH/NINDS; Cerebrotech Medical CARE PROGRAM Stock (options): Ornim 2015 AHA ICH Guidelines (used IV nicardipine infusions) Page 1
ATACH 2 • N=1000 – Worldwide – 56.2% of participants were Asian – More than half had GCS=15 – Median hematoma volume ~10 cc • Intervention – intravenous nicardipine infusion for 24 hours to meet systolic blood pressure target • Outcome – unable to walk or worse – 38.7% in SBP < 140 mmHg group • Difference in Blood Pressure – 37.1% in SBP < 180 mmHg group • No difference in outcome • Trend towards more adverse events at 3 months in < 140 mmHg group (esp renal [posthoc]) Qureshi NEJM 2016 Qureshi NEJM 2016 2015 AHA ICH Guidelines New Definition of Hypertension • American Heart Association recently dramatically revised its definition of high blood pressure and guidelines for management. – Whelton JACC 2017 Page 2
What About ICH? BP in ICH – Practical Considerations • High blood pressure is – The most common cause of ICH – Is present in most patients with acute ICH regardless of cause of ICH – Is the most important target for primary and secondary prevention of ICH • Acute BP treatment – May not be as beneficial as we hoped – Has not been compared against “no treatment” • “Update” to 2015 AHA/ASA ICH Guidelines as a result of ATACH2 – May be more complex than we hoped • So what is the target now? » Variability may be bad (Manning Lancet Neurol 2014) At UCSF and ZSFG we have changed to SBP < 160 mmHg » One size may not fit all – Precision Medicine needed • Example in periop care: Futier JAMA 2017 Whelton JACC 2017 BP in ICH – Practical Considerations What to Do? • Acute BP Management in ICH – Lower the BP – Select an intermediate target. » SBP < 160 mmHg for at least 3 days? • Long-term BP Management in ICH – Select a target. < 130/80 mmHg in most cases – Discharge patient on BP meds and write the target in the chart – Recognize high BP in the office and start treatment (time to dispense with notion of “white coat” hypertension) Page 3
2/16/2018 Will We Ever Truly Have Closure? The “Absolute Mess” PFO Following Stroke of PFO in Stroke • Around 20-25% of all patients have a PFO • PFO alone is not necessarily associated with higher risk of recurrent stroke – Higher risk: Larger PFO, associated atrial septal aneurysm, perhaps younger age • Three previous negative trials of closure S. Andrew Josephson MD devices but cardiologists pre-2017 were still Carmen Castro Franceschi and Gladyne K. Mitchell Neurohospitalist Distinguished Professor performing these procedures widely Chair, Department of Neurology Director, Neurohospitalist Program University of California, San Francisco The speaker has no disclosures New Data: N Engl J Med 2017 Case Study RESPECT Gore REDUCE CLOSE • A 76F presents to stroke clinic following an Stroke attributed to PFO + Cryptogenic stroke within Cryptogenic stroke within Inclusion Criteria atrial septal aneurysm OR past 270 days + PFO past 180 days + PFO large PFO embolic-appearing stroke Participants 980 participants 644 participants 663 participants • Workup for etiology was negative except Intervention Arm PFO closure PFO closure + antiplatelet PFO closure + antiplatelet ipsilateral 30% carotid stenosis Antiplatelet or Arm 1: antiplatelet Medical Rx Arm Antiplatelet • She has a “very small” PFO on TTE anticoagulation Arm 2: anticoagulation Less recurrent clinical and • I have an extensive discussion about the (lack Less recurrent stroke with clinical+radiographic Less recurrent stroke with Results PFO closure (NNT 42) stroke with PFO closure PFO closure (NNT 20) of) significance of this lesion and our plans to (NNT 28) not intervene: She is delighted 1
2/16/2018 2018 Meta-Analyses • Many more to come; all only as good as the primary trials they are examining • Each included 4 of the 5 trials as one device tested previously no longer commercially available and not particularly effective Shah R et al and DeRosa S et al Ann Intern Med 2018 Shah R et al and DeRosa S et al Ann Intern Med 2018 What now? “Let’s close all these PFOs!” • DO NOT close all these PFOs • DO screen patients for PFO (?how) • It is sensible to discuss with your cardiologists some “Rules of the Road” • At the end of the day, this is an exciting advance for some (young) people with stroke that can make a substantial impact on recurrence rates Shah R et al and DeRosa S et al Ann Intern Med 2018 2
2/16/2018 Rules of the Road Risks to Discuss With Your Patients • Atrial Fibrillation rates higher • Consider PFO closure if: • No great data beyond 5-10 years – The patient is younger than 60 years old • Antiplatelet regimens variable but most – AND you can be sure the PFO is the most include duals for some time and then likely etiology after a thorough workup monotherapy – AND the qualifying event is a stroke (not TIA) – And what if AF develops? that appears embolic (not lacunar) • Major risk for stroke is up front rather than – Likely concentrate on large PFOs or those with an atrial septal defect spread throughout subsequent years • Cardiologists new task: start counting bubbles • Medical management: Options appear equal 3
2/16/2018 Current controversies UPDATE ON • Screening for unruptured aneurysms INTRACRANIAL • Who to screen? ANEURYSM • What to do with small aneurysms? • When to screen? • How often? Nerissa U. Ko, MD, MAS • Predicting aneurysms at high risk for Recent Advances in Neurology rupture February 15, 2018 • Any risk factors? • When to treat? Guideline recommendations • Family history > 2 first • Non-invasive imaging degree family initially 6-12 months members with IA or (CTA/MRA/DSA) SAH • Follow-up one year or • Genetic risk factors every other year to determine if: • Polycystic kidney disease • Ehler’s-Danlos, aortic • Aneurysm size > 7mm coarctation, microcephalic • Aneurysm enlargement osteodysplastic primordial • Consideration for treatment dwarfism • History of prior SAH 1
2/16/2018 2
2/16/2018 3
2/16/2018 • PHASES score Summary • Population (Finnish, Japanese) • Small aneurysms have a very low risk of • HTN growth and rupture • Age > 70 • Recent modeling and systematic review • Size studies recommend no monitoring or • Hx SAH intervention in small aneurysms in the • Aneurysm location general population • Score < 3 associated • However, the dilemma of identifying which with lower, but not small aneurysm will rupture remains negligible risk of bleed problematic Future directions • Better selection of high risk patients to monitor, including women with FMD • Use of new grading scales like PHASES if validated • Biological imaging of growth, areas of activity • High resolution MRA, feromoxytol • Development of biomarkers to predict risk • DNA, mRNA, microRNAs, proteomics 4
Recommend
More recommend