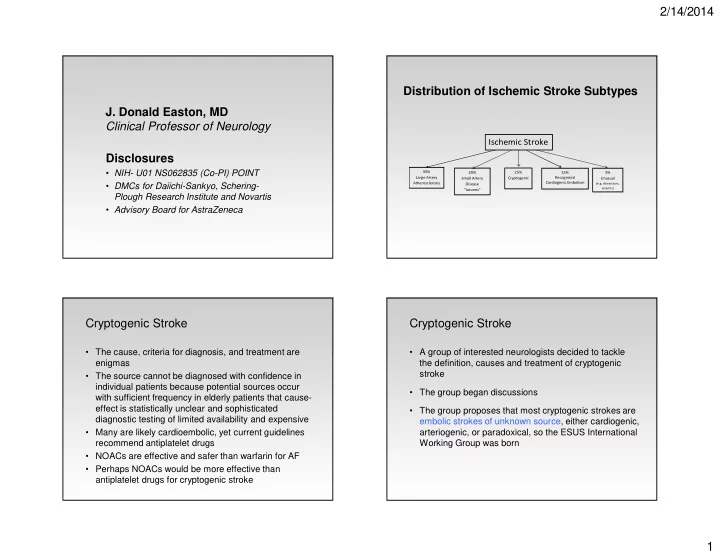
2/14/2014 Distribution of Ischemic Stroke Subtypes J. Donald Easton, MD Clinical Professor of Neurology Ischemic Stroke Disclosures • NIH- U01 NS062835 (Co-PI) POINT 35% 20% 25% 15% 5% Large Artery Small Artery Cryptogenic Recognized Unusual • DMCs for Daiichi-Sankyo, Schering- Cardiogenic Embolism Atherosclerosis (e.g. dissections, Disease arteritis) “lacunes” Plough Research Institute and Novartis • Advisory Board for AstraZeneca Cryptogenic Stroke Cryptogenic Stroke • The cause, criteria for diagnosis, and treatment are • A group of interested neurologists decided to tackle enigmas the definition, causes and treatment of cryptogenic stroke • The source cannot be diagnosed with confidence in individual patients because potential sources occur • The group began discussions with sufficient frequency in elderly patients that cause- effect is statistically unclear and sophisticated • The group proposes that most cryptogenic strokes are diagnostic testing of limited availability and expensive embolic strokes of unknown source, either cardiogenic, • Many are likely cardioembolic, yet current guidelines arteriogenic, or paradoxical, so the ESUS International recommend antiplatelet drugs Working Group was born • NOACs are effective and safer than warfarin for AF • Perhaps NOACs would be more effective than antiplatelet drugs for cryptogenic stroke 1
2/14/2014 Major Causes of Ischemic Stroke Atherosclerosis is Widespread at Autopsy Small Artery Disease Intracranial Atherosclerosis Carotid Stenosis Carotid Plaque with Emboli Atrial Fibrillation Aortic Arch Plaque Valve Disease Cardiogenic Emboli Ventricular Thrombi Thromboembolism plays a role almost all ischemic strokes. Cryptogenic Stroke: current ESUS: proposed • An ischemic stroke of “otherwise undetermined cause” • It is proposed that ESUS replace cryptogenic stroke • Embolic strokes of undetermined source are defined as • Depends on the extent of diagnostic evaluation (the non-lacunar brain infarcts without proximal arterial harder you look, the more you find) stenoses or cardioembolic sources with a clear indication for anticoagulation • No standard criteria for “determined cause” • Because emboli consist mainly of thrombus, it is likely that • It is an old term that is itself cryptic, vague and has anticoagulants will reduce recurrent brain ischemia more impeded clinical research effectively than antiplatelet agents. Randomized trials testing direct-acting oral anticoagulants for secondary • So, this description defines what it isn’t, and we want to prevention are warranted know what it is! 2
2/14/2014 Diagnostic Criteria for Embolic Stroke of Diagnostic Studies Required for ESUS Undetermined Source (ESUS) must be sufficient to: • Brain CT* or MRI to demonstrate non-lacunar stroke (*visualization usually requires delayed imaging >24 hrs after onset) • Demonstrate acute brain infarct on neuroimaging that is non-lacunar • Imaging of both extracranial and intracranial arteries supplying the area of the infarct • Demonstrate absence of occlusive proximal (conventional, MR, or CT angiography, or transcranial Doppler atherosclerosis ultrasonography) • Demonstrate no major-risk cardioembolic source • Exclude major cardioembolic source (12-lead EKG, cardiac monitoring >24 hours with automated rhythm detection, echocardiography) Embolic strokes of undetermined source: ESUS in Summary: A novel construct The case for a new clinical construct Cryptogenic Stroke / ESUS International Working Group • Most cryptogenic strokes are embolic (cardiogenic, arteriogenic, paradoxic) Writing Committee: • Extensive diagnostic efforts to define the specific cause are Robert G. Hart often futile and may be unnecessary Hans-Christoph Diener • ESUS (embolic strokes of undetermined source) is a new, Shelagh B. Coutts clinically useful construct J. Donald Easton Christopher B. Granger • For secondary prevention of ESUS, anticoagulants are likely to be more efficacious than antiplatelet drugs Martin J. O’Donnell Ralph L. Sacco Stuart J. Connolly Lancet Neurol 2014 (in press April 2014) 3
2/14/2014 The ESUS group then discussed treatment trials for ESUS with the FDA R andomized E valuation in S econdary stroke P r e vention C omparing the T hrombin inhibitor dabigatran etexilate versus ASA in E mbolic • The FDA enthusiastically supported a comparison S troke of U ndetermined S ource (ESUS) of NOACs vs. ASA ~20% of ischaemic strokes have been categorized in recent studies as ESUS • – 20-30% of ischemic strokes Primary endpoint: stroke – No previous trials to define optimal care Event-driven: 350 End of treatment Index Index – High likelihood that anticoagulants effective Dabigatran (150 or 110 mg BID)** ischaemic ischaemic n=3000 – Widespread equipoise for anticoagulant vs. aspirin for stroke (ESUS)* stroke (ESUS)* Placebo (matching ASA) secondary prevention R ‘Diagnostic Pathway’: – Enthusiasm high in the stroke research community Placebo (matching dabigatran) assess with MRI/CT to n=3000 rule out lacunae; carotid ASA (100 mg OD) U/S and ≥24 hour • The ESUS group has contributed to launching two rhythm monitoring to rule out AF 30-day large trials comparing NOACs to aspirin 0 days – 3 months 0.5–3 years follow-up *mRS ≤3, age ≥60 or 50–59 with additional risk factors. Includes TIA with pathological imaging evidence.**All patients receive dabigatran 150 mg BID, unless ≥75 years or CrCl <50 mL/min. These patients receive dabigatran 110 mg BID ASA = acetylsalicylic acid; BID = twice daily; CrCl = creatinine clearance; CT = computed tomography; ESUS= embolic stroke of undetermined source; MRI = magnetic resonance imaging; mRS = modified Rankin score; OD = once daily; SE = systemic embolism; TIA = transient ischaemic attack 4
Recommend
More recommend