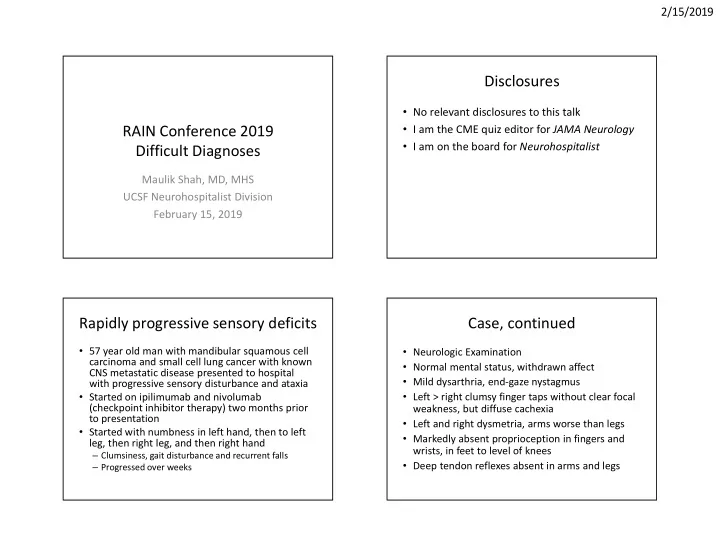
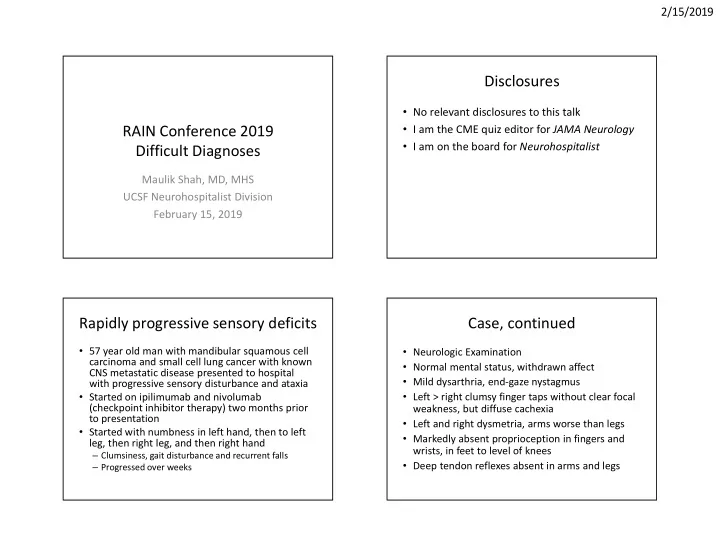
2/15/2019 Disclosures • No relevant disclosures to this talk • I am the CME quiz editor for JAMA Neurology RAIN Conference 2019 • I am on the board for Neurohospitalist Difficult Diagnoses Maulik Shah, MD, MHS UCSF Neurohospitalist Division February 15, 2019 Rapidly progressive sensory deficits Case, continued • 57 year old man with mandibular squamous cell • Neurologic Examination carcinoma and small cell lung cancer with known • Normal mental status, withdrawn affect CNS metastatic disease presented to hospital • Mild dysarthria, end-gaze nystagmus with progressive sensory disturbance and ataxia • Started on ipilimumab and nivolumab • Left > right clumsy finger taps without clear focal (checkpoint inhibitor therapy) two months prior weakness, but diffuse cachexia to presentation • Left and right dysmetria, arms worse than legs • Started with numbness in left hand, then to left • Markedly absent proprioception in fingers and leg, then right leg, and then right hand wrists, in feet to level of knees – Clumsiness, gait disturbance and recurrent falls • Deep tendon reflexes absent in arms and legs – Progressed over weeks 1
2/15/2019 Question #1 Which of the following has been reported as a neurologic complication of checkpoint inhibitor cancer therapy? A. Acute demyelinating polyneuropathy 88% B. Cerebellitis C. Limbic encephalitis D. Myasthenia gravis E. All of the above have been reported in 3% 3% 3% 2% the literature s s s i t t i v i . . l i i . . . l l a e l e a r b o b h g e p e p a r e i v g e n a n c C n e h t i e h a e t n c s v i b i a o l y b e m y M a m i L e h e d t e f o t u l l c A A Checkpoint Inhibitor Neurotoxicity, Checkpoint Inhibitor Neurotoxicity continued • Immune-mediated cancer therapy, the use of • Adverse events have included tissue/organ-specific autoimmune-based disease which has greatly expanded over last few years – Colitis and thyroiditis • Inhibit down-regulatory signals directed toward T • Neurologic complications range from 2-5% in various cells via targets such as cytotoxic T-lymphocyte- case series associated antigen 4 (CTLA4) and programmed – Rate >10% in some series of combination therapy cell death-1 (PD-1) leads to upregulation of – Often seen despite favorable response in terms of primary cytotoxic T-cell activity and tumor death malignancy • Used for melanoma, small cell lung cancer, renal • Pathophysiology unclear cell carcinoma, and increasingly for other – Shared antigen on healthy tissue and cancer cells treatment refractory neoplasms including – Activation of underlying autoimmune disease primary CNS malignancy – “Unmasking” of paraneoplastic syndrome 2
2/15/2019 Checkpoint Inhibitor Neurotoxicity, Case, continued continued Labs and Work-up • Peripheral nervous system complications • Serum labs notable for SIADH – Demyelinating polyneuropathy / AIDP • EMG/NCS: Non-length-dependent, generalized – Myositis including necrotizing myositis – Myasthenia gravis sensory neuropathy versus neuronopathy with – Vasculitis peripheral nerve disease multifocal involvement of motor nerves and • Central nervous system complications nerve roots and mild demyelinating findings – Aseptic meningitis – Encephalitis, NMDA-receptor limbic encephalitis • CSF with WBC 30 (95% lymphocytes), glucose 48, – Cerebellitis and protein 184 – Myelitis, necrotizing myelopathy • Exacerbation of other inflammatory conditions • MRI Brain and systemic imaging showing – Radiation toxicity improvement in burden of metastatic disease 3
2/15/2019 Question #2 Which of the following etiologies is of primary concern given results of diagnostic testing and MRI spine imaging? A. Viral myelitis 72% B. Autoimmune / paraneoplastic myelitis C. Metastatic disease with intramedullary involvement 16% 7% D. Compressive spondylotic myelopathy 5% 0% E. Metabolic myelopathy s y i t . . . . h i . . . . t e l p i . i a y o h t p m e t o i l o n w y l e a l a d r e n y r a m i s o V p a p c / e s s l i e i e o d n v b u c i s a m i s t t e e a m t r M s p i a o m t u t e o A M C 4
2/15/2019 Question #3 Which of the following MR imaging pattern of findings would be most suggestive of a paraneoplastic cause of myelitis? A. “Owl’s eye” appearance and hyperintensity of anterior spinal cord 85% B. Nodular leptomeningeal and exiting nerve root enhancement C. Short segment peripherally based asymmetric homogenously enhancing single lesion 10% 4% 1% D. Longitudinally extensive tract-specific symmetric T2 hyperintensity and contrast enhancement on Short segment peripheral.. Longitudinally extensive ... “Owl’s eye” appearance ... Nodular leptomeningeal... T1 Case, continued CRMP-5 Autoimmune Myelitis • Collapsing response-mediator protein 5 • CSF testing returned positive for CRMP-5-IgG – Intracellular antigen antibody • Associated with variety of neurologic • Treated with high-dose IV steroids followed by presentations including oral taper – Peripheral neuropathy • Given lack of improvement, plasmapheresis was – Retinopathy, optic neuropathy initiated and patient completed five exchanges – Chorea, cerebellar ataxia • Deficits stabilized but did not improve – Myelitis • Associated most commonly with small cell lung • No further treatments given goals of care and cancer patient desire to return home – Renal cell carcinoma, thymoma, seminoma, others 5
2/15/2019 Paraneoplastic Myelitis • In one case series, most patients had longitudinally extensive myelitis with symmetric enhancement that was tract-specific or gray matter restricted • CSF was inflammatory with pleocytosis, unique oligoclonal bands • Anti-amphiphysin antibody most common, CRMP-5 second • Onset could occur months prior to neoplasm discovery • Poor prognosis for recovery even with cancer therapy Checkpoint Inhibitor Neurotoxicity MRI of Spine Treatment CSF Analysis: Elevated WBC or • Guidelines suggest that treatment is based on severity IgG index or OCB of neurologic symptoms Vascular (Ischemic) • Discontinuation of immune therapy Dural AV fistula Vitamin B12 deficiency • High dose steroids followed by oral taper Nitrous Oxide toxicity Multiple Sclerosis HSV Lymphoma Vitamin E deficiency • Adjunct based on disease and severity Neuromyelitis optica CMV Intramedullary tumors: Copper deficiency ADEM – IVIg or plasmapheresis EBV -Ependymoma Adrenoleukodystrophy / SLE VZV -Astrocytoma Adrenomyeloneuropathy • Goal may be stabilization of deficits MOG HIV -Hemangioblastoma HIV vacuolar myelopathy Sjogren’s WNV (AHC) Paraneoplastic – In one case series, 30% of patients had minimal or no Sarcoid HTLV (not always -CRMP-5 significant improvement Vasculitis inflammatory) -Amphiphysin • Role of steroid-sparing agent Enterovirus 68, 71 -GFAP Fungal: cocci, histo – Rituximab, cyclophosphamide, azathioprine Tuberculosis Mycoplasma Lyme Syphilis 6
2/15/2019 Patterns of Myelitis on Imaging • There is broad differential for transverse myelitis and basic CSF results are unlikely to help discriminate between etiologies – There are now many possible antibodies and pathogens that can now be tested for – Test results may not return for weeks • Patterns on imaging may help narrow differential diagnosis – Focus diagnostic evaluation – Allow for earlier initiation of empiric therapy 7
2/15/2019 Multiple Sclerosis • Short lesions, spanning usually no more than 2 segments • Located in periphery of spinal cord on axial sequences, often asymmetric, involving dorsal or lateral columns • During time of acute flare, lesions enhance with gadolinium contrast NMO Real 1 • Characteristic brain lesions – Periventricular, juxta-cortical, infratentorial – Extending from corpus callosum Neuromyelitis Optica • Associated with aquaporin-4-antibody • Longitudinally extensive, 3 or more segments • Acute flare often associated with diffuse contrast enhancement and cord edema • On axial imaging, central cord usually involved, both gray and white matter • Can have brain lesions – Hypothalamus, periventricular – Area postrema, around third/fourth ventricle 8
Recommend
More recommend