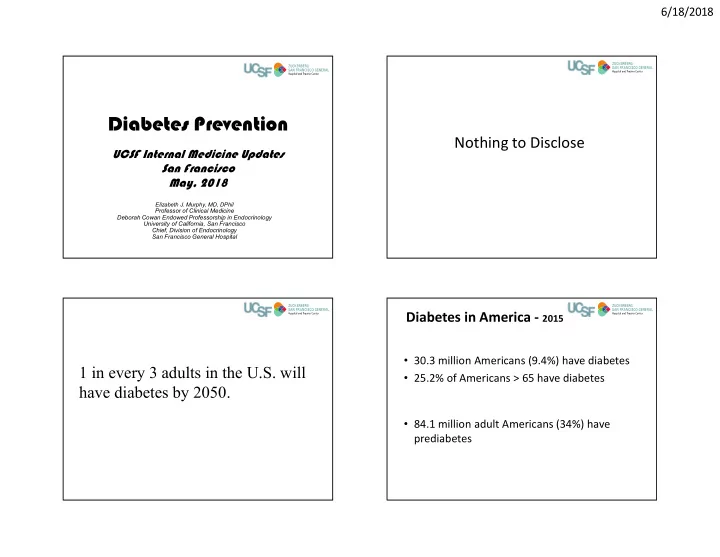
6/18/2018 Diabetes Prevention Nothing to Disclose UCSF Internal Medicine Updates San Francisco May, 2018 Elizabeth J. Murphy, MD, DPhil Professor of Clinical Medicine Deborah Cowan Endowed Professorship in Endocrinology University of California, San Francisco Chief, Division of Endocrinology San Francisco General Hospital Diabetes in America - 2015 • 30.3 million Americans (9.4%) have diabetes 1 in every 3 adults in the U.S. will • 25.2% of Americans > 65 have diabetes have diabetes by 2050. • 84.1 million adult Americans (34%) have prediabetes 1
6/18/2018 What is the only safe way to cure and treat DM2 long-term? Don’t develop it in the first place. Societal Change Basic Assumptions for today • Weight loss will prevent/delay diabetes • Increased activity will prevent/delay diabetes • Eating less leads to weight loss • Weight loss and increased activity are good no matter what • Harms associated with behavioral interventions to promote weight loss are minimal to non-existent 2
6/18/2018 My Assumptions Discrepancy Between Reported and Actual Energy Intake and Expenditure • Intensive lifestyle methods are beneficial Activity Energy Energy Intake 3000 for everyone and we should not just focus * Expenditure on those at highest immediate risk 2500 • We should focus lifestyle interventions on 2000 Kcal/d patients who are motivated 1500 * • Widespread lifestyle change will have spill 1000 over effects 500 0 Reported Actual Reported Actual * P <0.05 vs reported. Lichtman et al. N Engl J Med 1992;327:1893. Slide Source: www.obesityonline.org Key Questions Key Questions • Who is at highest risk of diabetes and how do • Who is at highest risk of diabetes and how do we easily identify them? we easily identify them? • What does the evidence show about success • What does the evidence show about success of interventions? of interventions? • What options are available for Diabetes • What options are available for Diabetes Prevention? Prevention? • What about cost and what will get paid for? • What about cost and what will get paid for? 3
6/18/2018 ADA/AMA/CDC National Ad Campaign Ad Council • Push for self testing of diabetes risk • In English, Spanish • With hedgehogs, disco goats or puppies What was your score? Who is at Highest Risk for DM? BMI cut points were roughly • History of gestational diabetes 25-30 = 1 point • Family history of diabetes 30-40 = 2 points >= 5 High Diabetes Risk >40 = 3 points • Age 66% • Overweight and obese A. A = 0-4 points • Sedentary B. B = 5-6 points • High risk ethnic group 22% C. C = 7 or more points • Impaired glucose metabolism 6% 6% D. D = I have diabetes • High waist to hip ratio A = 0-4 points B = 5-6 points C = 7 or more points D = I have diabetes 4
6/18/2018 Diabetes Prevalence by Ethnicity – Northern California 35 year old sedentary Asian woman, BMI 29.5 history of GDM with a brother, mother and father with diabetes. Karter et al, Diabetes Care 2015 Do I have diabetes.org (ADA/AMA/CDC/Ad Council) 5 or more at increased risk 0 0 1 1 0 1 1 4 BMI 25-30 30-40 >40 5
6/18/2018 35 year old sedentary Asian woman, BMI 29.5 history of GDM with a brother, mother and father with diabetes. • TV screen – 3 points (5) low risk = 13 • ADA paper screen – 4 points (5) low risk • Doihaveprediabetes.org – 4 points (5) low risk • National Diabetes Prevention Program Screen – 13 points (9) High risk 9 or more, high risk BMI >27 Includes questions on smoking, eating fruits and vegetables, waist circumference 6
6/18/2018 Conclusions – Who and How to Screen? • Use a screening tool that will capture the largest number of people • Use tools that include Asian specific BMI cut-offs • As with screening for gestational diabetes, perhaps easiest to screen widely Laboratory Screening Recommendations Prediabetes • CDC DPP – Positive on high risk on screening tools AND • Fasting glucose 100 or 110-125 mg/dl • BMI ≥ 24 kg/m 2 or ≥ 22 kg/m 2 in Asian-Americans OR • History of GDM • ADA • A1C 5.7-6.4% – Everyone over age 45 – Adults who are overweight or obese and an additional risk factor (BMI ≥ 25 kg/m 2 or ≥ 23 kg/m 2 in Asian-Americans) • 2h glucose post 75 OGTT 140-199 mg/dl • USPSTF – Age 40-75 with BMI ≥ 25 kg/m 2 7
6/18/2018 % Dysglycemic Patients USPSTF Recommendations Captured by USPSTF Screening Guideline • No ethnicity appropriate BMI cut-offs 100% • Doesn’t allow for screening of < 40 90% • Poor sensitivity (45%) and may detect only 80% 70% 25% of dysglycemic patients in 3 year f/u 1 60% 50% 40% 30% 20% 10% 0% 1 O ’ Brien MJ, Lee JY, Carnethon MR, Ackermann RT, Vargas MC, et al. (2016) Detecting Dysglycemia White African American Latino Using the 2015 United States Preventive Services Task Force Screening Criteria: A Cohort Analysis of O ’ Brien MJ, Lee JY, Carnethon MR, Ackermann RT, Vargas MC, et al. (2016) Detecting Dysglycemia Using the 2015 United States Community Health Center Patients. PLoS Med 13(7): e1002074. Preventive Services Task Force Screening Criteria: A Cohort Analysis of Community Health Center Patients. PLoS Med 13(7): e1002074. doi:10.1371/journal.pmed.1002074 Key Questions USPSTF • Who is at highest risk of diabetes and how do • Weight Loss to Prevent Obesity-Related we easily identify them? Morbidity and Mortality in Adults: Behavioral • What does the evidence show about success Interventions of interventions? – Behavioral interventions led to weight loss, • What options are available for Diabetes reduced DM2, less weight regain (moderate Prevention? benefit) • What about cost and what will get paid for? – Harms are small to none 8
6/18/2018 Diabetes Prevention Program Lifestyle Intervention • 3234 Participants • High Risk: • 16 week curriculum with individual sessions • Good diversity – 25 years or older – BMI ≥ 24 kg/m 2 or ≥ 22 kg/m 2 – 19% African American over 24 weeks in Asian-Americans – 16% Hispanic • After 24 weeks follow up individual and group – Fasting glucose 95 - 125 – 5% American Indian mg/dL and OGTT glucose 140 – 4% Asian and Pacific Islanders sessions for reinforcement to 199 mg/dL • Healthy low fat, low calorie diet • Randomized • metformin (850 mg BID) OR • 150 minutes of moderate-intensity physical • extensive, individual lifestyle intervention activity per week NEJM 346:393, 2002; Lancet 374:1677, 2009. Lifestyle Group 7% weight loss at one year 4% weight loss at 4 years 150 minutes of moderate-intensity physical activity per week Diabetes Prevention Program Research Group. N Engl J Med 2002;346:393-403. 9
6/18/2018 Sub Group Findings Reduction in Diabetes by Weight Loss • Metformin – most effective in < 60 years old and BMI > 35 or if a history of gestational diabetes – As effective as lifestyle in that group – Least effective in lower fasting glucose and lower BMI • Lifestyle – more effective with lower base-line OGTT glucose. • No significant differences based on sex, race or ethnic group NEJM 346:393, 2002. Lancet. 2009; 374: 1677–1686 Risk Reduction DPP 15 years DPP- Outcomes Study 18% with metformin 34% with Lifestyle • All subjects offered lifestyle intervention in a group format for one year • Everyone offered maintenance group sessions quarterly • Lifestyle group offered further supplementary group programs and an individual lifestyle check in twice a year • 88% of DPP enrolled 10
6/18/2018 Microvascular Outcomes Finnish Diabetes Prevention Study • Followed for Microvascular Outcomes • 500+ Finnish participants, – Nephropathy • Abnl OGTT; Ave BMI 31 – Retinopathy • Diabetes diagnosed as FBG>140 or OGTT>200 – Neuropathy • Lifestyle intervention • Lower prevalence in those who did not – Exercise = Gardening, snow shoveling, berry develop diabetes picking, gathering mushrooms, rowing, forest work • No significant treatment effect (yet) • Weight loss 5% • ~3 years follow up NEJM 2001;344:1343-1350 Finnish DPP Results Finnish DPP 7 years • 58% reduction in incidence of diabetes • Diabetes developed in 6% vs. 14% • As with US DPP, success was dependent on achieving the goals NEJM 2001;344:1343-1350 Lancet 2006; 368: 1673–79 11
6/18/2018 Da Qing Study- 20 and 23 years Da Qing Study • 43% reduction in incidence of DM over 20 years • No difference in rate of CV events or CVD death at 20yr • 577 participants with IGT in China • At 23 years, CV and all-cause mortality were reduced – Control vs. Diet, Exercise, or Diet AND Exercise – HR 0.59 and 0.71 – 6 year follow up CV mortality – 30-45% reduction in incidence of diabetes in intervention groups All-cause mortality – Different interventions were comparable Lancet 2008; 371: 1783–89 Lancet Diabetes & Endocrinology, 2014, 2(6): 474-480 Diabetes Care. 1997. 20(4): 537-44. The Future of Type 2 DPP Translational Studies Diabetes Care • Focus on more cost efficient delivery • Focused on weight loss – All achieve early weight loss – Long term durability of weight loss not as clear • Don’t yet have diabetes prevention data for translational programs • Other potential benefits – Lipids – HTN – Depression 12
Recommend
More recommend