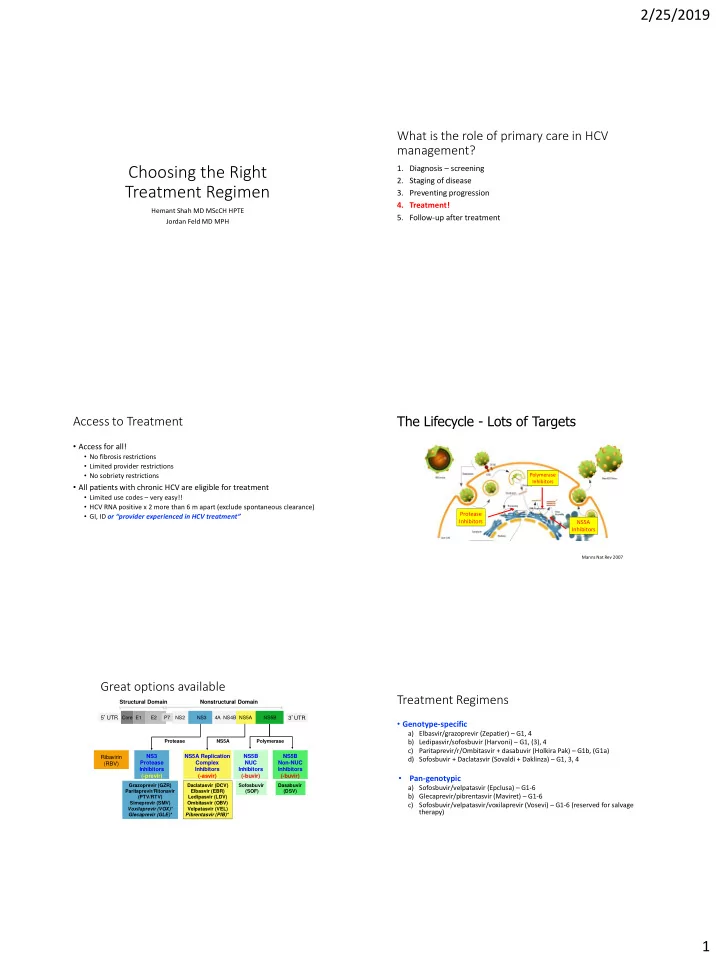
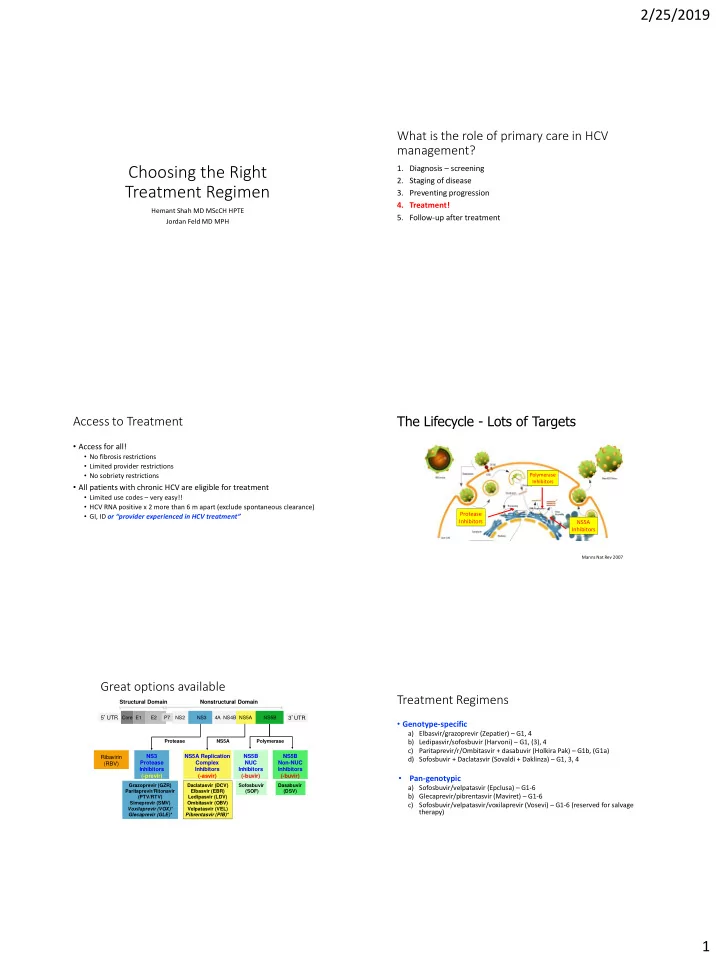
2/25/2019 What is the role of primary care in HCV management? Choosing the Right 1. Diagnosis – screening 2. Staging of disease Treatment Regimen 3. Preventing progression 4. Treatment! Hemant Shah MD MScCH HPTE 5. Follow-up after treatment Jordan Feld MD MPH The Lifecycle - Lots of Targets Access to Treatment • Access for all! • No fibrosis restrictions • Limited provider restrictions • No sobriety restrictions Polymerase Inhibitors • All patients with chronic HCV are eligible for treatment • Limited use codes – very easy!! • HCV RNA positive x 2 more than 6 m apart (exclude spontaneous clearance) Protease • GI, ID or “provider experienced in HCV treatment” Inhibitors NS5A Inhibitors Manns Nat Rev 2007 Great options available Treatment Regimens Structural Domain Nonstructural Domain 5 ’ UTR Core E1 E2 P7 NS2 NS3 4A NS4B NS5A NS5B 3 ’ UTR • Genotype-specific a) Elbasvir/grazoprevir (Zepatier) – G1, 4 Protease NS5A Polymerase b) Ledipasvir/sofosbuvir (Harvoni) – G1, (3), 4 c) Paritaprevir/r/Ombitasvir + dasabuvir (Holkira Pak) – G1b, (G1a) NS3 NS5A Replication NS5B NS5B Ribavirin d) Sofosbuvir + Daclatasvir (Sovaldi + Daklinza) – G1, 3, 4 Protease Complex NUC Non-NUC (RBV) Inhibitors Inhibitors Inhibitors Inhibitors • (-previr) (-asvir) (-buvir) (-buvir) Pan-genotypic Grazoprevir (GZR) Daclatasvir (DCV) Sofosbuvir Dasabuvir a) Sofosbuvir/velpatasvir (Epclusa) – G1-6 Paritaprevir/Ritonavir Elbasvir (EBR) (SOF) (DSV) b) Glecaprevir/pibrentasvir (Maviret) – G1-6 (PTV/RTV) Ledipasvir (LDV) Simeprevir (SMV) Ombitasvir (OBV) c) Sofosbuvir/velpatasvir/voxilaprevir (Vosevi) – G1-6 (reserved for salvage Voxilaprevir (VOX)* Velpatasvir (VEL) therapy) Glecaprevir (GLE)* Pibrentasvir (PIB)* 1
2/25/2019 Approved Regimens Approach to Treatment Individualized Simplified • Comprehensive assessment of • Basic assessment of each patient each patient • Choose a pan-genotypic agent • Identifying best drug for patient according to: according to: • Genotype • Genotype • Decompensated cirrhosis yes/no • Degree of fibrosis • Work with a couple of drugs • Past treatment history • Other characteristics • Work with all the drugs Individualized BUT simple approach to treatment SOF/LDV (Harvoni) or SOF/VEL (Epclusa) 1. Confirm infection – RNA + genotype • Single Tablet Regimen 2. Exclude cirrhosis – APRI < 0.7 3. Exclude drug interactions – www.hep-druginteractions.org • Well tolerated 4. Start! • Fatigue, headache common, occasionally severe • Some patients complain more than expected Regimen Genotype Duration Pills (weeks) per • SOF/LDV (not SOF/VEL) 1a 1b 2 3 4 5 6 day • can shorten to 8 weeks if HCV RNA<6 M IU/ML SOF/LDV 8-12 1 (Harvoni) • DDIs – NS5A adds some ELB/GZV • Acid Suppression : Reduce absorption up to 80%! (8)-12 1 (Zepatier) • PPI – best to avoid (can co-administer) • Antacid – 4 hrs apart SOF/VEL • H2RA – 12 hrs apart or together 12 1 (Epclusa) • Seizure meds : All seizure meds except Kepra • HBV/HIV - tenofovir – increase levels (renal toxicity) GLE/PIB* 8 3 • Cardiac: Digoxin – avoid (Mavyret) Crestor - increase risk of rhabdo – usually stop it * Non-cirrhotic, no prior treatment SOF/VEL/VOX (Vosevi) Elbasvir/Grazoprevir (Zepatier) • Single Tablet Regimen • Well tolerated • Single Tablet Regimen • Well tolerated • Fatigue, headache common, occasionally severe • Fatigue, headache • Additional side effect of mild diarrhea in about 15-20% of • Cannot be used in decompensated cirrhosis patients • Some patients complain more than expected • Resistance an issue with G1a (not with G1b) • Similar DDIs – NS5A adds some • If present extend to 16 weeks and add RBV • Either test everyone (guidelines) or Treat naïve/relapsers x 12w & non- • Acid Suppression : Reduce absorption up to 80%! responders for 16 weeks with RBV (Label) • Seizure meds : All seizure meds except Kepra • HBV/HIV - tenofovir – increase levels (renal toxicity) • DDIs – protease adds some • Cardiac: Digoxin – avoid Crestor - increase risk of rhabdo – - No PPI issue usually stop it - Limited Amio issue • Because of Voxilaprevir, cannot use in decompensated - Safe in renal failure including dialysis cirrhosis - Look up the others… 2
2/25/2019 Pibrentasvir/Glecaprevir (Maviret) Comparison of Pan-genotypic Regimens • Three Tablets Taken all at once • Well tolerated SOF/VEL GLE/PIB • Fatigue, headache • 1 pill per day • 3 pills per day • Cannot be used in decompensated cirrhosis • No issues with resistance to date • 12 weeks for all • 8 weeks – non-cirrhotic • For non-cirrhotic patients – 8 weeks • DDI • 12 weeks – cirrhotic (maybe 8 • For cirrhotic patients – 12 weeks (8 week study looks promising) • • PPI weeks??) Can be used in some patients who have failed prior DAA therapy, but not preferred • Statins • DDI • DDIs – protease adds some • BCP - No PPI issue • Statins - Limited Amio issue - Safe in renal failure including dialysis - Look up the others… When would I choose 1 first-line agent over Genotypes in Canada the other? • SOF/LDV (Harvoni) • G1a especially if HCV RNA<6 M IU/mL (8 weeks) • Decompensated cirrhosis (with RBV) • SOF/VEL (Epclusa) • Can’t think of any…maybe LDV resistance? • EBV/GZV (Zepatier) • G1b • Chronic kidney disease (eGFR<45 and for sure <30) • Cannot stop PPI • GLE/PIB (Maviret) • Chronic kidney disease (eGFR<45 and for sure <30) • All non-cirrhotic patients can have 8 weeks of treatment, even if high viral load What’s worth noting? - Genotype 1 subtype Centre for Disease Analysis 2014 - Genotype 3 + cirrhosis Why does G1 sub-type matter? Genotype 3 is important • 2 nd most common genotype globally – 10- G1b – EASY to cure G1a – Tougher to cure 15% in the US (more among S. Asian • No need for resistance testing – • Protease-based regimens a immigrants) no effect bit less effective • Associated with more • No need for RBV • Previously would rapid progression of occasionally need ribavirin • Protease-based regimens highly fibrosis and higher risk of or resistance testing (not HCC effective anymore) • Sub-optimal responses to DAAs with established cirrhosis Nkontchou J Viral Hep 2011 3
2/25/2019 Pangenotypic regimen Example For G3 Cirrhosis, ADD Ribavirin SOF + Velpatasvir (NS5A) x 12 wks in G3: SOF/RBV x 24 G1, 2, 4, 5, 6 – Naïve/Experienced +/- cirrhosis vs SOF/VEL x 12 99 99 100 100 97 100 98 97 100 100 91 80 SVR12 (%) 80 SVR12 (%) 60 60 40 1 relapse 1 relapse 1 death 40 2 lost to follow-up 1 withdrew consent 20 618 206 117 104 116 34 41 73/ 191/ 624 210 118 104 116 35 41 197 80 0 0 F0-3 F4 Total 1a 1b 2 4 5 6 Genotype Esteban et al. 2018 Feld NEJM 2015, Foster NEJM 2015 Back to a Super Duper Simplified Approach If you treat 1000 patients this way… **Assume refer decompensated to specialist Action Number of Patients Cured Not Cured • G1, 2, 3 * , 4, 5, 6 Treat First Line 1000 950 50 • SOF/VEL x 12 weeks Treat Second Line 50 45 5 • GLE/PIB x 8 weeks TOTAL TREATMENTS ADMINISTERED: 1050 • G3 Cirrhosis: • SOF/VEL/RBV x 12 weeks OVERALL CURE RATE: 99.5% • GLE/PIB x 12 weeks • Treatment Failures: • SOF/VEL/VOX x 12 weeks That’s why we’re doing ECHO! Treating HCV in Primary Care Project ECHO - Linking PCPs to specialists - Facilitates linkage to care • Therapy is getting MUCH easier - Allows people to be treated by people and in settings they know & trust • Simpler regimens - 20’ didactic followed by cases Nurses • Fewer contraindications • Minimal monitoring Other care providers • Support from hepatology/ID Primary Care MDs • Project ECHO • Preceptorships Now we cover more than HCV • Patients prefer it! HBV, fatty liver, alcohol, cirrhosis • Patients prefer local treatment by HCPs they know! Monday 12 to 1:30 PM – free, CME credits! • HIV a great model 4
2/25/2019 Summary • Hepatitis C treatment regimen selection is much easier than in the past • Simplified approach can utilized • Few scenarios to be aware of (Decompensation, DDIs, G1 subtype, G3 cirrhosis) • In the wheelhouse of primary care 5
Recommend
More recommend