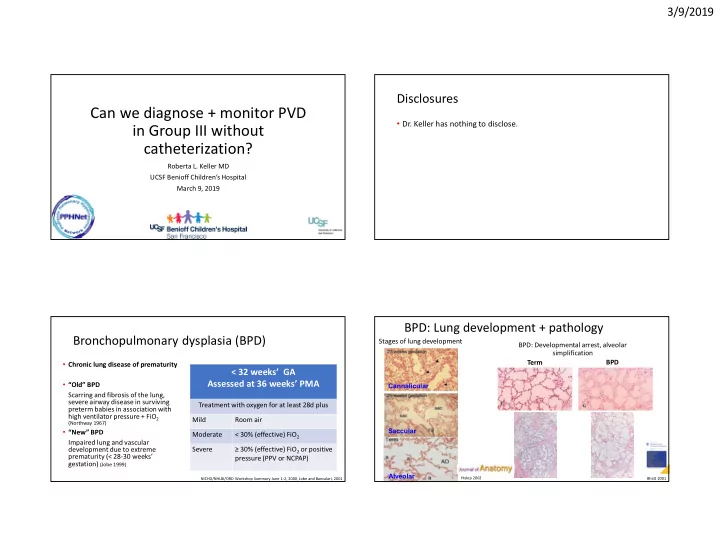
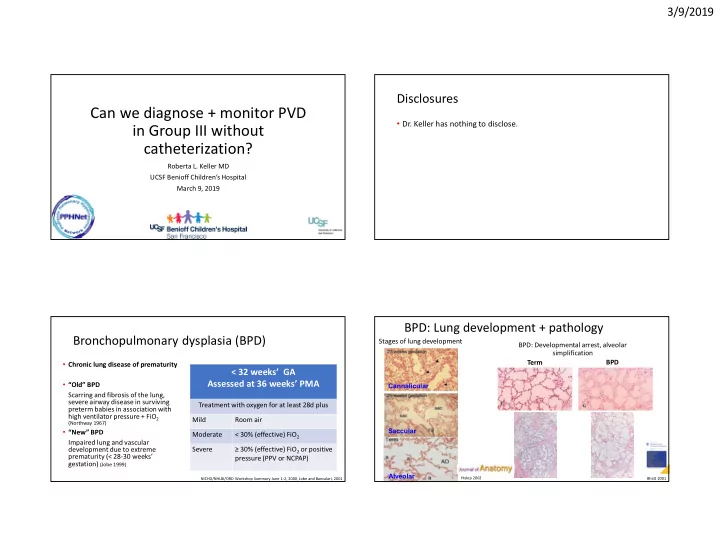
3/9/2019 Disclosures Can we diagnose + monitor PVD • Dr. Keller has nothing to disclose. in Group III without catheterization? Roberta L. Keller MD UCSF Benioff Children’s Hospital March 9, 2019 BPD: Lung development + pathology Bronchopulmonary dysplasia (BPD) Stages of lung development BPD: Developmental arrest, alveolar simplification BPD Term • Chronic lung disease of prematurity < 32 weeks’ GA Assessed at 36 weeks’ PMA • “Old” BPD Cannalicular Scarring and fibrosis of the lung, severe airway disease in surviving Treatment with oxygen for at least 28d plus preterm babies in association with high ventilator pressure + FiO 2 Mild Room air (Northway 1967) Saccular • “New” BPD Moderate < 30% (effective) FiO 2 Impaired lung and vascular development due to extreme Severe ≥ 30% (effective) FiO 2 or positive prematurity (< 28-30 weeks’ pressure (PPV or NCPAP) gestation) (Jobe 1999) Alveolar Hislop 2002 NICHD/NHLBI/ORD Workshop Summary June 1-2, 2000, Jobe and Bancalari, 2001 Bhatt 2001 1
3/9/2019 BPD + pulmonary vascular disease (PVD): Echocardiography: defining PH in BPD? echocardiography Pressure estimates Echo measurement Criteria used for classification* Tricuspid regurgitant (TR) jet Right ventricular systolic pressure (RVsp) > 40 velocity** mmHg [right atrial pressure (RAp) = 0] RVsp:SBP ratio ≥ 1/2 or 2/3 (RAp = 0 or 5 mmHg) Non-restrictive cardiac shunt Right-to-left or bidirectional flow RV (PDA, VSD, atrial septum) RV RV RV or PA pressure ≥ 1/2 or 2/3 systemic Interventricular septum (IVS) D-shaped or convex into LV position Flattened throughout the cardiac cycle Any flattening LV LV LV *Assumes no RV outflow tract obstruction Flat Normal D-shaped **By modified Bernoulli equation: RVsp = 4 x velocity 2 + RAp (assumed RAp noted) Echocardiography: interventricular septum (IVS) position Mourani 2008, Keller 2010, Mirza 2014, Mourani 2015, Lusk 2015 Cardiac cathetherization: defining PH Gold standard • Cardiac catheterization Mortality in infants with • Mean P PA ≥ 25 mmHg, and/or • PVR > 3 Woods Units bronchopulmonary dysplasia: • Wedge pressure ≤ 15 mmHg (no LA hypertension or PV obstruction) data from cardiac catheterization Steurer et al, Pediatric Pulmonology 2019, In Press 2
3/9/2019 Pulmonary vascular resistance (PVR) + Patient characteristics (n=30) oxygenation Characteristic n = 30 Gestational age 25 5/7 (24 4/7 – 26 6/7) Male sex 60% History of surgical PDA closure 30% Cardiac catheterization Postmenstrual age 49 2/7 (42 4/7 – 57 1/7) Weight 3750 (3100-5100) Respiratory support at catheterization None 3% Nasal cannula ≤ 2 LPM 27% Nasal cannula > 2 LPM 13% Nasal CPAP 33% PF Ratio vs PVR A-a gradient vs PVR Mechanical ventilation 23% Mortality 27% (8/30) Steurer 2019 Catheterization: Measured parameters + Catheterization: PH criteria + mortality mortality PVR mean PAP Cardiac index PV stenosis < 3 vs > 3 < 25 vs > 25 < 3.5 vs > 3.5 P=0.005 P=0.12 P=0.38 P=0.66 mean RAp A-a gradient PVR + mean PAP criteria < 8 vs > 8 < 110 vs > 110 P=0.15 P=0.77 P=0.28 Steurer 2019 Steurer 2019 3
3/9/2019 PH by echocardiogram: validity Mortality: Prematurity and PVS • Survival lower with severe PH # of veins Unilateral vs (classified by IVS position, systemic- affected bilateral to-suprasystemic at any time) < 3 vs ≥ 3 37% vs 78% at 1y from diagnosis • Any PH (> 50% systemic) at 36 weeks’ PMA associated with higher mortality (Mourani 2015) : 4/39 (10%) vs 3/238 (1%); P=0.009 SGA vs Age at Dx AGA/LGA < 6 mos vs ≥ 6 mos Echo diagnosis in only 56% (22/39) Khemani 2007 Mahgoub 2017 Severe BPD + PH (echo diagnosis) No PH PH P value Discharge status n=1307 n=370 Mortality after 36 weeks’ PMA 5% 21% <0.001 Remains hospitalized at 1y corrected 1% 5% <0.001 age PHIS linkage n=961 n=184 Congenital diaphragmatic hernia Home oxygen 69% 86% <0.001 Tracheostomy + home ventilation 9% 27% <0.001 Readmission by 1y corrected age 41% 51% 0.01 ICU admission 16% 30% <0.001 Mechanical ventilation 15% 30% <0.001 Mortality 1% 1% 0.80 Lagatta 2018 4
3/9/2019 Neonatal pulmonary vascular status in CDH PH assessment (echocardiography) assessment by echocardiography RV RV RV • Pulmonary hypertension (PH) due to increased pulmonary vascular resistance (PVR) • Classification of PH severity • < 2/3 systemic (no-mild) • ≥ 2/3 systemic – systemic (moderate) LV LV LV • systemic – suprasystemic (severe) Normal D-shaped Flat • Measurements (echocardiography): hierarchical evaluation • TR jet less common with lower pressure estimate • Patent ductus arteriosus flow direction + velocity • Interventricular septal (IVS) position • < 2/3 systemic: 17/44 (39%) • Normal, flattened, or D-shaped • ≥ 2/3 systemic: 29/47 (62%) • Tricuspid regurgitant (TR) jet velocity • suprasystemic: 34/49 (69%) • RVsp = 4 * velocity 2 + RAp • 4/144 (3%) echocardiograms indeterminate Keller 2010 Keller 2010 Time to resolution of PH (echo validation) Time to resolution of PH (echo validation) 19% 19% 11% 11% 70% 70% 17 d (IQR 7, 21 d) 5
3/9/2019 Death Death/Prolonged respiratory support (56d) Death Death/Prolonged respiratory support (56d) n (%) P n (%) P n (%) P n (%) P Week 1 Week 1 PH 23/128 (18) 0.35 52/128 (41) 0.02 PH 23/128 (18) 0.35 52/128 (41) 0.02 No PH 0/8 (0) 0/8 (0) No PH 0/8 (0) 0/8 (0) Week 2 Week 2 PH 20/86 (23) <0.001 47/86 (55) <0.001 PH 20/86 (23) <0.001 47/86 (55) <0.001 No PH 0 (0/47) 3/47 (6) No PH 0 (0/47) 3/47 (6) Week 3 Week 3 PH 15/55 (27) <0.001 36/55 (65) <0.001 PH 15/55 (27) <0.001 36/55 (65) <0.001 No PH 0 (0/73) 9/73 (12) No PH 0 (0/73) 9/73 (12) Week 4 Week 4 PH 13/46 (28) <0.001 30/46 (65) <0.001 PH 13/46 (28) <0.001 30/46 (65) <0.001 No PH 0 (0/80) 13/80 (16) No PH 0 (0/80) 13/80 (16) Week 6 Week 6 PH 9/34 (26) <0.001 21/34 (62) <0.001 PH 9/34 (26) <0.001 21/34 (62) <0.001 No PH 1/89 (1) 19/89 (21) No PH 1/89 (1) 19/89 (21) Lusk 2015 Lusk 2015 Death Death/Prolonged respiratory support (56d) Death Death/Prolonged respiratory support (56d) n (%) P n (%) P n (%) P n (%) P Week 1 Week 1 PH 23/128 (18) 0.35 52/128 (41) 0.02 PH 23/128 (18) 0.35 52/128 (41) 0.02 No PH 0/8 (0) 0/8 (0) No PH 0/8 (0) 0/8 (0) Week 2 Week 2 PH 20/86 (23) <0.001 47/86 (55) <0.001 PH 20/86 (23) <0.001 47/86 (55) <0.001 No PH 0 (0/47) 3/47 (6) No PH 0 (0/47) 3/47 (6) Week 3 Week 3 PH 15/55 (27) <0.001 36/55 (65) <0.001 PH 15/55 (27) <0.001 36/55 (65) <0.001 No PH 0 (0/73) 9/73 (12) No PH 0 (0/73) 9/73 (12) Week 4 Week 4 PH 13/46 (28) <0.001 30/46 (65) <0.001 PH 13/46 (28) <0.001 30/46 (65) <0.001 No PH 0 (0/80) 13/80 (16) No PH 0 (0/80) 13/80 (16) Week 6 Week 6 PH 9/34 (26) <0.001 21/34 (62) <0.001 PH 9/34 (26) <0.001 21/34 (62) <0.001 No PH 1/89 (1) 19/89 (21) No PH 1/89 (1) 19/89 (21) Lusk 2015 Lusk 2015 6
3/9/2019 Death Death/Prolonged respiratory support (56d) Death Death/Prolonged respiratory support (56d) n (%) P n (%) P n (%) P n (%) P Week 1 Week 1 PH 23/128 (18) 0.35 52/128 (41) 0.02 PH 23/128 (18) 0.35 52/128 (41) 0.02 No PH 0/8 (0) 0/8 (0) No PH 0/8 (0) 0/8 (0) Week 2 Week 2 PH 20/86 (23) <0.001 47/86 (55) <0.001 PH 20/86 (23) <0.001 47/86 (55) <0.001 No PH 0 (0/47) 3/47 (6) No PH 0 (0/47) 3/47 (6) Week 3 Week 3 PH 15/55 (27) <0.001 36/55 (65) <0.001 PH 15/55 (27) <0.001 36/55 (65) <0.001 No PH 0 (0/73) 9/73 (12) No PH 0 (0/73) 9/73 (12) Week 4 Week 4 PH 13/46 (28) <0.001 30/46 (65) <0.001 PH 13/46 (28) <0.001 30/46 (65) <0.001 No PH 0 (0/80) 13/80 (16) No PH 0 (0/80) 13/80 (16) Week 6 Week 6 PH 9/34 (26) <0.001 21/34 (62) <0.001 PH 9/34 (26) <0.001 21/34 (62) <0.001 No PH 1/89 (1) 19/89 (21) No PH 1/89 (1) 19/89 (21) Lusk 2015 Lusk 2015 Death Death/Prolonged respiratory support (56d) RV: systemic pressure ratio n (%) P n (%) P healthy newborns Week 1 PH 23/128 (18) 0.35 52/128 (41) 0.02 No PH 0/8 (0) 0/8 (0) • Term Week 2 ∆ Preterm PH 20/86 (23) <0.001 47/86 (55) <0.001 No PH 0 (0/47) 3/47 (6) Week 3 PH 15/55 (27) <0.001 36/55 (65) <0.001 No PH 0 (0/73) 9/73 (12) Week 4 PH 13/46 (28) <0.001 30/46 (65) <0.001 No PH 0 (0/80) 13/80 (16) Week 6 PH 9/34 (26) <0.001 21/34 (62) <0.001 No PH 1/89 (1) 19/89 (21) Lusk 2015 Skinner 1991 7
Recommend
More recommend