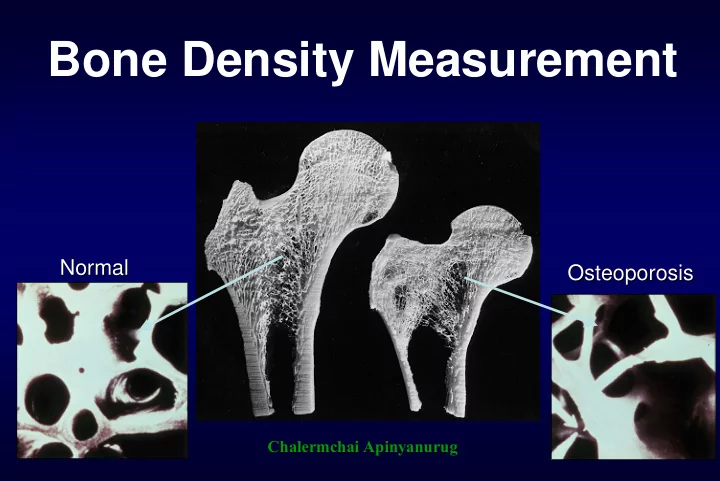
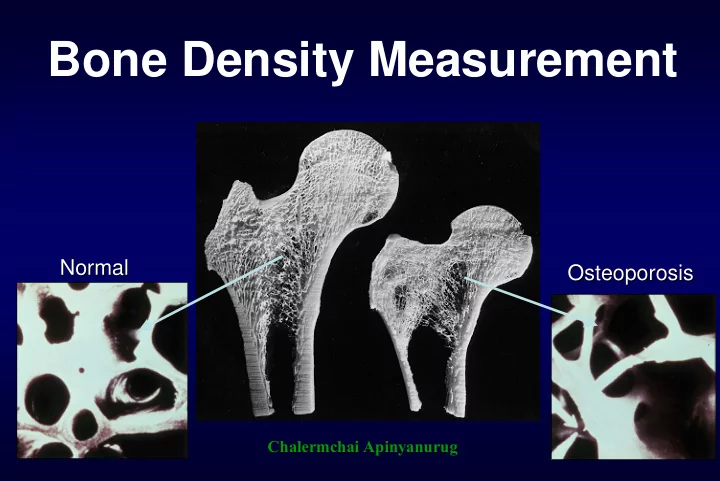
Bone Density Measurement Normal Normal Osteoporosis Osteoporosis Chalermchai Apinyanurug
Who should receive BMD testing? National Osteoporosis North American Menopause American Association of Foundation Society Clinical Endocrinolgist • All women age ≥ 65 yr • All women age ≥ 65 yr • All women age ≥ 65 yr • All women age ≥ 40 yr • Younger PM women • All women with with ≥ 1 risk factor medical causes of bone who have sustained a fracture unrelated to loss • PM women who major trauma present with fractures • Younger PM women with ≥ 1 risk factor • All peri- and PM women who have risk factors for fracture or bone loss
Indications for Bone Mineral Density (BMD) Testing From ISCD 2006 • Women aged 65 and older, Men aged 70 and older • Postmenopausal women under age 65 with risk factors • Adults with a fragility fracture • Adults with a disease or condition associated with low bone mass or bone loss • Adults taking medications associated with low bone mass or bone loss • Anyone being considered for pharmacologic therapy • Anyone being treated, to monitor treatment effect • Anyone not receiving therapy in whom evidence of bone loss would lead to treatment Women discontinuing estrogen should be considered for bone density testing according to the indications listed above
Densitometry Technologies Central BMD Measurements – QCT – DEXA Peripheral BMD Measurements – Conventional X-ray – RA – radiographic absorptiometry – X-Ray Radiogrammetry – Ultrasonometry – Peripheral DEXA
Routine radiographic –Low Radiation dose –Insensitive: bone loss is apparent only after a 30% loss
Radiographic Absorptiometry • measures the optical density • small, inexpensive • fingers only • poor hip fracture prediction
Radiogrammetry • Width of cortical bone in fingers using standard x-ray • Can be added to existing mammo / x-ray system (need computer and scanner) • fingers only • poor hip fracture prediction
QCT : Quantitative CT Disadvantage • High radiation dose • Less precise than DXA (2-5%) • Large accuracy errors (15%) • Expensive
Quantitative Ultrasound of Calcaneus Advantage • Portable • Low costs • Less time-consuming • No radiation • No need well-trained technician • May predict fracture Disadvantage • Not a gold standard • Diagnostic performance (High specificity but low sensitivity)
Investigations of osteoporosis : Update 2007
What’s new in DXA equipment's? New Detector : Direct-Digital Cadmium Zinc Telluride (CZT) Better image quality Low X-ray exposure High accuracy and precision
New technique : One Positioning One Position, 3 Scans • AP Spine • Left Femur • Right Femur
New DXA equipment : Better Image Quality New Old
New DXA equipment : Better Image Quality Old New
New Asian Reference Database • China • Korea • Indonesia • Japan • Thai
New software : Computer Assisted Densitometry • Automatic verification – Positioning – Bone edges – Analysis regions – Artifacts • Clinical Benefits – Reduce errors – Better scan evaluation
New Report • BMD results – Previous results – Reference Data Comparison – Trending – Bone strength assessments • Hip Axis Length • Femur Strength Index
New Hip Assessment • Hip Axis Length • Upper Neck • Dual femur study • Femur Strength Index “A Better Way to Look at the Femur” Osteoporosis International. January, 2006
Dual Femur study : Improved Diagnosis and Treatment Decisions American Society for Bone and Mineral Research : ASBMR 2005
Femur Strength Index Osteoporosis International. January, 2006 • 2,506 women. > 50 yr. • significant predictors of hip fracture • Power for predicting fracture was improved by combining T-score, FSI, and HAL compared with T- score alone.
Body Composition Methods Underwater Weighing DXA Imaging Methods Anthropometry (Hydrodensitometry) (Dual-energy X-Ray (CT, MRI) Absorptiometry) Near Infrared BIS BIA Air Displacement Interactance (Bioelectrical Impedance Analysis)
Body Composition with DXA • Directly measures fat, lean, and bone mass • Monitoring impact of treatment and exercise/diet regimens.
Body Composition and Cardiovascular Disease Ragi et al. ASBMR 2005 • Android/Gynoid Ratio identifies women with cardiovascular disease • Better than cholesterol, better than triglycerides
Estimated Total Body % Fat from Spine and Femur Scans ASBMR 2005
Interpreting T-scores (WHO) Correlates With Lifetime Fracture Risk for Caucasian Women Low Normal Osteoporosis Bone Mass Bone Mass (Osteopenia) -4.0 -3.5 -3.0 -2.5 -2.0 -1.5 -1.0 -0.5 0 +0.5 +1.0 Assessment of Fracture Risk and Its Application to Screening For Postmenopausal Osteoporosis WHO Study group; 1994.
Clinical Risk Score
Osteoporosis Self-Assessment Tool for Asians (OSTA) • 21 clinics, 8 countries: 860 PM women • 59% Chinese, 18% Korean, 11% Thai, 8% Filipinos, 4% Indian, Malay and others Index value = 0.2 x (weight - age), then drop the decimal digit OSTA index OSTA index ≤ -1: High risk < -4: High risk > -1: Low risk -1 to -4 : Medium risk > -1: Low risk Osteoporosis Self-Assessment Tool for Asians (OSTA) Research Group Osteoporos Int 2001;12:699-705
Validation of OSTA in Asians Countries N Age Sens Spec PPV 860 45-88 91 45 21 Original 722 43-81 88 54 34 Chinese 1127 47-91 90 38-43 NA Japanese 1101 48-87 87 67 24 Korean 1465 40-89 90 66 23 Filipinos 135 57-80 97 43 34 Singapore Thai 322 45-84 97 54 21 Khon Kaen 388 43-91 93 (93) 61 (30) 24 (15) Songkhla Sens: Sensitivity, Spec: Specificity, PPV: Positive predictive value
Khon Kaen Osteoporosis Study (KKOS) scoring system KKOS score Age (y) Score Weight (kg) Score • high risk ≤ -1 < 45 + 7.5 < 30 - 14 • low risk > -1 30 - 34 - 12 45 - 49 + 6.0 50 - 54 + 4.5 35 - 39 - 10 Sensitivity 86% 55 - 59 + 3.0 40 - 44 - 8 + 1.5 45 - 49 - 6 Specificity 65% 60 - 64 65 - 69 0 50 - 54 - 4 - 2 70 - 74 - 1.5 55 - 59 1.0 75 - 79 - 3.0 60 - 64 0 0.8 80 - 84 - 4.5 65 - 69 + 2 0.6 Sensitivity 70 - 74 + 4 85 – 89 - 6.0 0.4 > 90 - 7.5 75 - 79 + 6 AUC 0.85 0.2 80 - 84 + 8 0.0 0.0 0.2 0.4 0.6 0.8 1.0 85 - 89 + 10 1- Specificity > 90 + 12 Pongchaiyakul C. J Med Assoc Thai 2004;87:910-6.
Probability (%) of having osteoporosis for a given Age and Body weight Age (yr) Weight (kg) < 45 45-49 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-89 > 90 < 30 58.7 67.4 75.0 81.3 86.3 90.2 93.0 95.1 96.6 97.6 98.3 30-34 47.5 56.8 65.6 73.5 80.1 85.4 89.5 92.5 94.7 96.3 97.4 35-39 36.6 45.6 54.9 63.8 71.9 78.8 84.4 88.7 91.9 94.3 96.0 40-44 26.9 34.8 43.6 52.9 62.0 70.3 77.5 83.3 87.9 91.3 93.9 45-49 19.0 25.4 33.0 41.7 51.0 60.2 68.7 76.1 82.2 87.0 90.7 50-54 13.0 17.8 23.9 31.3 39.8 49.0 58.3 67.0 74.6 81.0 86.1 55-59 8.7 12.1 16.7 22.5 29.7 38.0 47.1 56.4 65.2 73.1 80.0 60-64 5.7 8.1 11.3 15.6 21.2 28.1 36.2 45.1 54.4 63.4 71.6 65-69 3.7 5.3 7.5 10.5 14.6 19.9 26.5 34.4 43.2 52.5 61.6 70-74 2.4 3.4 4.9 7.0 9.8 13.7 18.7 25.0 32.6 41.3 50.5 75-79 1.5 2.2 3.2 4.6 6.5 9.2 12.8 17.5 23.6 30.9 39.4 80-84 1.0 1.4 2.1 3.0 4.2 6.0 8.5 11.9 16.4 22.2 29.3 85-89 0.6 0.9 1.3 1.9 2.7 3.9 5.6 7.9 11.1 15.4 20.9 > 90 0.4 0.6 0.8 1.2 1.8 2.5 3.6 5.2 7.4 10.4 14.4 High risk Intermediate risk Low risk
56.7 (OR: 43.7) 60 Prevalence of osteoporosis 50 by DXA (%) 40 21.4 (OR: 9.1) 14.3 (OR: 5.6) 30 20 10 High risk OSTA Score (<-1) 2.9 0 Low risk (>-1) <-2.5 QUS of calcaneus (T-score) >-2.5 Figure 1. Prevalence of osteoporosis (by DXA) according to QUS of calcaneus and OSTA score
58.6 (OR: 60.9) 70 Prevalence of osteoporosis 60 50 by DXA (%) 40 16.7 (OR: 8.6) 20.7 (OR: 11.2) 30 20 10 High risk KKOS Score (<-1) 2.3 0 Low risk (>-1) <-2.5 QUS of calcaneus (T-score) >-2.5 Figure 2. Prevalence of osteoporosis (by DXA) according to QUS of calcaneus and KKOS score
Osteoporosis International 2007;18(4):525-31.
Predicted probability of having osteoporosis for a given age, weight and QUS Weight Age QUS T-score (SD) (kg) (yr) -4 -3 -2 -1 0 50 0.49 0.33 0.20 0.12 0.07 40 kg 55 0.59 0.43 0.28 0.17 0.10 60 0.68 0.53 0.37 0.23 0.14 65 0.77 0.63 0.47 0.32 0.19 70 0.83 0.72 0.57 0.41 0.27 75 0.88 0.79 0.67 0.51 0.35 80 0.92 0.85 0.75 0.61 0.45 85 0.94 0.90 0.82 0.70 0.55 50 0.28 0.17 0.10 0.05 0.03 50 kg 55 0.37 0.24 0.14 0.08 0.04 60 0.47 0.32 0.20 0.11 0.06 65 0.57 0.41 0.27 0.16 0.09 70 0.67 0.51 0.36 0.22 0.13 75 0.75 0.62 0.45 0.30 0.18 80 0.82 0.71 0.56 0.40 0.25 85 0.87 0.78 0.65 0.50 0.34
Recommend
More recommend