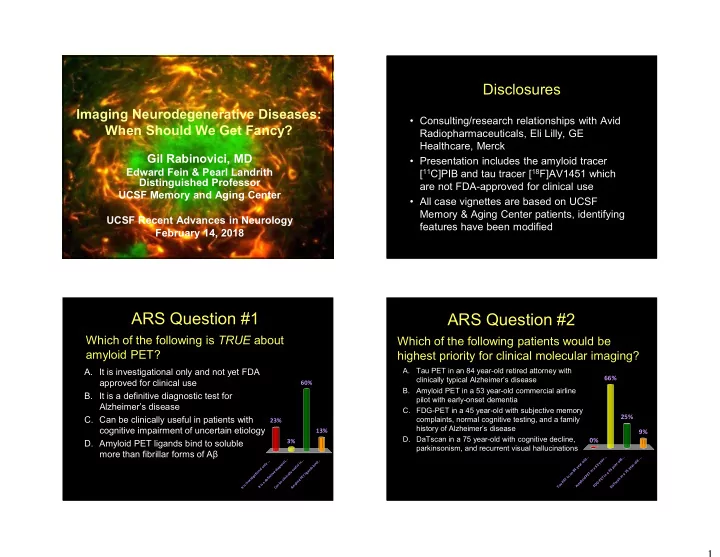
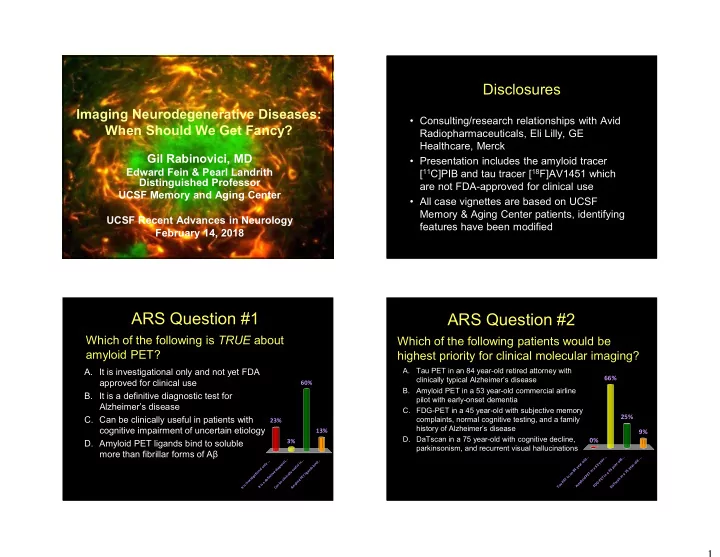
Disclosures Imaging Neurodegenerative Diseases: • Consulting/research relationships with Avid When Should We Get Fancy? Radiopharmaceuticals, Eli Lilly, GE Healthcare, Merck Gil Rabinovici, MD • Presentation includes the amyloid tracer Edward Fein & Pearl Landrith [ 11 C]PIB and tau tracer [ 18 F]AV1451 which Distinguished Professor are not FDA-approved for clinical use UCSF Memory and Aging Center • All case vignettes are based on UCSF Memory & Aging Center patients, identifying UCSF Recent Advances in Neurology features have been modified February 14, 2018 ARS Question #1 ARS Question #2 Which of the following is TRUE about Which of the following patients would be amyloid PET? highest priority for clinical molecular imaging? A. It is investigational only and not yet FDA A. Tau PET in an 84 year-old retired attorney with 66% clinically typical Alzheimer’s disease approved for clinical use 60% B. Amyloid PET in a 53 year-old commercial airline B. It is a definitive diagnostic test for pilot with early-onset dementia Alzheimer’s disease C. FDG-PET in a 45 year-old with subjective memory 25% C. Can be clinically useful in patients with complaints, normal cognitive testing, and a family 23% history of Alzheimer’s disease cognitive impairment of uncertain etiology 13% 9% D. DaTscan in a 75 year-old with cognitive decline, 0% D. Amyloid PET ligands bind to soluble 3% parkinsonism, and recurrent visual hallucinations more than fibrillar forms of Aβ . . . . . . . . . . . . d r d . . . . . . l a l d . . i . . o e o . t n d o l s n - y - y o i r r - l n l i a 3 a r n u b e 5 e a o g f e a e s y y l s d a y a d i 4 5 n u n 8 n 4 5 a i o e y g n 7 i v l T a t i a l i l a E a a t n i c T n P i n g n i E t i i n P i d T i s f i T E n e l o i e d c d E P a v e i P l - c n a o y G s b l m i s y u D T s n m a a i i A F t a T D I t I C A 1
Outline Clinical Diagnosis of AD Circa 1984 • Limitations of purely clinical diagnosis • MRI: more than just a “rule out” test • FDG-PET, DaTscan McKhann et al., Neurology 1984 • Amyloid PET “Clinical criteria for AD include insidious onset – Accuracy vs. neuropathology and progressive impairment in memory and other – Clinical applications cognitive functions. – Appropriate Use Criteria The diagnosis cannot be determined by laboratory tests – these tests are important – IDEAS: national study on clinical utility primarily in identifying other causes of dementia” • Preview of Tau imaging 1984 – 2018: Accuracy of Clinical Diagnosis of AD Evolution of AD Biomarkers U.S. Alzheimer’s Disease Centers 2005-10 • Probable AD (NINCDS-ADRDA) vs. autopsy* (n=526) – Sensitivity 71%, specificity 71% • Clinical diagnosis of non-AD dementia Structural FDG CSF Aβ 42 , Amyloid vs. autopsy* (n=271) MRI PET Tau, p-Tau PET In 2018, diagnosis of AD is still based on clinical – 39% found to have primary AD post-mortem symptoms and cognitive testing. Laboratory tests are still used primarily to exclude other causes of dementia. * Based on pathologic criteria of intermediate or high-likelihood AD (NIA-Reagan: CERAD-mod or freq; Braak III-VI) Beach et al., J Neuropathol Exp Neurol 2012 2
MRI: Not Just a “Rule Out” Test Limitations of Clinical Diagnosis • Atrophy patterns • Same clinical phenotype can be due to – Cortex, medial temporal, multiple pathologies basal ganglia, brainstem, cerebellum • Same pathology can lead to multiple • Cerebrovascular clinical phenotypes – Infarcts; white matter AD FTD hyperintensities • Clinical manifestations occur late in FTD mentioned in radiology • Diffusion abnormalities disease course report in only 10% of patients – Cortical and subcortical (Suarez et al., Neurology 2009) DWI in CJD – Long pre-clinical phase offers a therapeutic • “Pathognomonic” features window for early intervention – “Hummingbird” – PSP – “Hot cross buns” - MSA Clinical Quantitative MRI FDG-PET in Dementia Syndromes Desikan et al. AJNR Am J Neuroradiol. 2013 Bohnen et al. J Nucl Med 2012 3
Lost in Translation? Diagnostic Accuracy of FDG “AD” vs. “Non-AD” • Comparison of FDG reads in the community to expert clinical diagnosis (Shipley et al., Neurol Clin Pract 2013) Sensitivity Specificity – FDG performed in 49/1580 (3.1%) – PET reads discordant with final expert dx in 65% Silverman et al. 2001 94% 73% • Sources of error (mixed, n=138) Jagust et al. 2007 – Ambiguous metabolic patterns 84% 74% (mixed, n=44) • Very little use of SSP or other statistical displays Minoshima et al. 2001 – Limited radiologist experience with brain PET 90% 80% (AD vs. DLB, n=53) • 89% read by general radiologists or non- Foster et al. 2007 97% 86% radiologists (AD vs. FTD, n=45) – Non-specific or inappropriate clinical question • 7% ordered for AD vs. FTD Imaging Amyloid Plaques Dopamine Imaging: 123 I-FP-CIT ( 11 C-PIB PET) SPECT (DaTscan) Amyloid plaques Pittsburgh Compound B (PIB) • FDA approved for Parkinson’s disease vs. essential tremor • Some studies support utility in DLB vs. AD • More sensitive than clinical exam for Abnormal Normal dopaminergic deficit • Not useful in identifying McKeith et al . Lancet Neurol 2007 cause of degenerative parkinsonism (e.g. PD vs. MSA or PSP) Klunk et al ., Ann Neurol 2004 4
Pathology Validation: Florbetapir PET 18 F-florbetapir (Amyvid TM ) FDA approved April 2012 18 F O O O N NHCH 3 18 F-flutemetamol (Vizamyl TM ) FDA approved October 2013 18 F-florbetaben (Neuraceq TM ) FDA approved March 2014 Clark et al. JAMA 2011 Amyloid PET Visual Reads At a Loss for Words PET vs. Autopsy Studies • 57 year-old RH practicing internist with 2 years of progressive word-finding Tracer N Report Sensitivity Specificity difficulties Florbetapir (Amyvid) 1 59 Median 92% 95% Flutemetamol (Vizamyl) 2 68 Median 88% 88% – Struggles to come up with words that Florbetaben (Neuraceq) 3 82 Median 98% 80% should be familiar – Embarrassing socially and professionally Gold standard: moderate- frequent neuritic plauques (CERAD) – Feels less efficient at accomplishing tasks 1 – Clark et al., Lancet Neurol 2012 2 – Curtis et al., JAMA Neurol 2015 – No other cognitive or physical symptoms 3 – http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/204677s000lbl.pdf – Has not impacted daily function 5
At a Loss for Words At a Loss for Words • General physical and neurological exams wnl • Basic laboratory work-up normal • MMSE 30/30 • MRI: “age-appropriate global volume loss, mild periventricular white matter changes” • Fluent speech with occasional pauses; poor repetition; comprehension/reading/writing wnl • Patient’s questions: • Boston Naming Test 12/15 (normal≥14) – Is this normal aging? – If not, what is the diagnosis? • Average performance for age on tests of • I’m worried about Alzheimer’s but my memory executive functions is fine • Above average on verbal memory, superior – Can I keep working and if so for how long? visual memory – Should I take a cholinesterase inhibitor? Amyloid Positivity in Normal Older Adults: At a loss for Words: PET Results Concept of Preclinical AD [ 18 F]FDG-PET [ 11 C]PIB-PET 15%-30% of cognitively normal L R L R older adults are Aβ+ • More common in ApoE4+ and older age Aβ+ “controls” • AD-like structural and functional • Diagnosis: MCI – High likelihood due to AD (NIA-AA) brain changes Logopenic-variant primary progressive aphasia • Longitudinal cognitive decline • Treatment • Elevated risk of – Cholinesterase inhibitor incident cognitive – Referral to anti-A clinical trial impairment – Early retirement due to medical disability Mintun 2006; Pike 2007; Mormino 2009 & 2011; Sperling 2011; Chételat 2012; Petersen 2015 6
Recommend
More recommend